Nephrotic Syndrome – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Nephrotic Syndrome
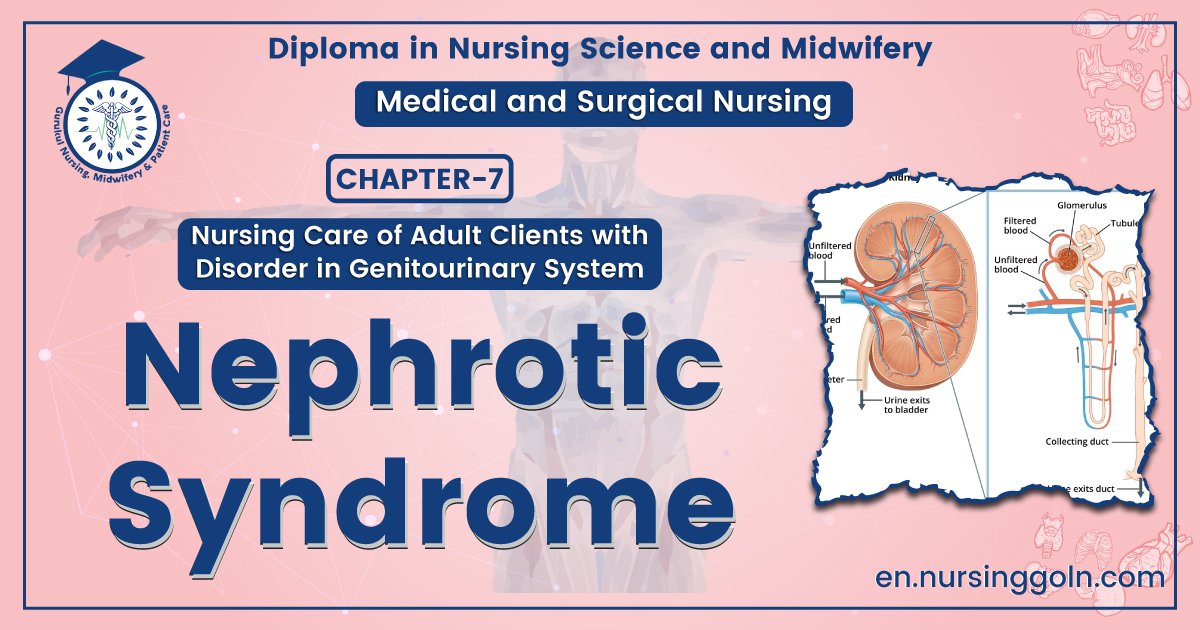
Definition of Nephrotic Syndrome:
It is clinical condition characterized by –
- Massive proteinuria (>3.5 gm/day)
- Hypo albuminaemia (<30 gm/L)
- Generalized oedema and
- Hypercholesterolemia
Or
Nephrotic syndrome is a symptoms complex characterized by massive proteinuria, hypo albuminaemia, generalized oedema, hyperlipidemia and lipiduria.
Or
Nephrotic syndrome is an alteration of kidney function caused by increased glomerular basement membrane permeability to plasma protein (albumin).
Causes of Nephrotic Syndrome:
A. Primary glomerulonephritis:
- Minimal change nephropathy
- Focal segmental glomerulosclerosis
- Membranous GN
- Proliferative GN-mesangial focal
- Mesangiocapillary GN
B. Secondary:
a. Systemic disease:
- Systemic lupus erythematosus
- Polyarthritis nodosa
- Amyloidosis
- Diabetes mellitus
b.Infection:
- Bacterial endocarditis
- Malaria
- Hepatitis B
c. Tumours: Carcinoma, Hodgkin’s disease
d. Drugs: Penicillamine, captopril, gold, mercury
C. Congenital nephrotic syndrome
Management of Nephrotic Syndrome:
Clinical Features:
a. Symptoms:
- Generalized oedema – First appears on the face then become generalized.
- Scanty micturition
- Abdominal distension and discomfort
- Thromboembolism
- Infection
- Massive proteinuria
- Non specific symptoms: Nausea, anorexia, malaise, weakness
- Sudden abdominal pain due to renal vein thrombosis
b. Signs:
- Puffy face
- Anaemia
- Ascitis and oedema
- BP-normal or raised
- Bilateral pleural effusion may be present
Investigation:
- Urine for RME
- 24 hour urinary protein estimation: >3.5 gm/24 hrs/1.73 m² body surface
- Serum total protein: <30 gm/L, albumin, globulin
- Rerial function test
- Blood for TC, DC, ESR, Hb%
- Serum complement level
- USG of KUB region
- X-ray chest P/A view
- HBsAg and other specific test to find out secondary causes
- Renal biopsy

Treatment of nephrotic syndrome:
- Diet: Salt restriction
- Normal protein diet
- Fluid restriction – previous day output + 400 ml/m² body surface
Control of oedema by diuretics –
- Thiazide diuretic eg. bendrofluazide 5-10 mg daily or
- Loop diuretic eg. Frusemide 80-120 mg daily
- In some cases IV salt poor albumin infusion may help to establish a diuresis
Specific measures:
Prednisolone 60 mg/m²/day in 3 divided for 4 weeks followed by alternate day prednisolone 40 mg/m²/48 14 hours as a single dose for another 4 weeks.
Treatment of complication:
- Infection by appropriate antibiotic
- Venous thrombosis: IV heparin 20 IU/kg/hour followed by oral anticoagulant
- Hyperlipidaemia: HMG-CoA reductase inhibitor
- Treatment of oliguric renal failure
Nursing Management of Nephrotic Syndrome
- Assessment and Document the location and character of the patient’s edema.
- Measure blood pressure with the patient lying down and standing. Immediately report a decrease in systolic or diastolic pressure exceeding 20 mm Hg.
- If the patients receive a renal biopsy, watch for bleeding and signs of shock.
- Monitor intake and output and weigh the patient each morning after he voids and before he eats.Make sure he’s wearing the same amount of clothing each time you weigh him.
- Ask the dietitian to plan a low-sodium diet with moderate amounts of protein.
- Frequently check urine for protein.
- Monitor plasma albumin and transferrin concentrations to evaluate overall nutritional status.
- Provide meticulous skin care to combat the edema that usually occurs with nephrotic syndrome.
- Use a reduced-pressure mattress or padding to help prevent pressure ulcers.
- To prevent the occurrence of thrombophlebitis, encourage activity and exercise, and provide antiembolism stockings as ordered.
- Give the patient and family reassurance and support, especially during the acute phase, when edema is severe and the patient’s body image changes
Patient teaching and home health care guide for Nephrotic Syndrome
- If the patients receive immunosuppressants, teach him and family members to report even mild signs of infection.
- If the patients receive long-term corticosteroid therapy, teach him and family members to report muscle weakness and mental changes.
- To prevent GI complications, suggest to the patient that he take steroids with an antacid or with cimetidine or ranitidine. Explain that the adverse effects of steroids subside when therapy stops, but warn the patient not to discontinue the drug abruptly or without a physician’s consent.
- Stress the importance of adhering to the special diet.
- If the physician prescribes antiembolism stockings for home use, show the patient how to safely apply and remove them.
Complication:
Hypovolaemia
Infection eg.
✔ Pneumococcal peritonitis
✔ Pneumococcal UTI
✔Pneumococcal pneumonia
✔ Pneumococcal meningitis
- Thrombo embolism
- Renal failure
- Electrolytes imbalance
- Hyperlipidaemia and atherosclerosis