Pelvic fracture – An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Pelvic fracture
Classifications of pelvic fracture: Injuries of the pelvis fall into four groups, 1) Isolated fractures with an intact pelvic ring: Avulsion, direct, stress fracture.
2) Fractures pelvic ring: Anteropostero compression, Lateral compression, Vertical compression.
3) Fractures of the acetabulum: Although these are ring fractures, involvement of the joint raises special problems and therefore they are considered separately.
4) Sacrococygeal fractures.
[Ref-Apley’s “System of Orthopaedics and Fractures” 9″ edition page-832]
Mechanisms of pelvic fracture:
There are four mechanisms by which pelvic ring fractures are produced:
1) Lateral compression.
2) Anteroposterior compression.
3) Vertical shears forces.
4) Inferior forces (e.g. fall on buttocks).
The first two mechanisms are common in RTA and may cause stable or unstable fractures. Vertical shear forces are due to fall from a height and will cause grossly unstable fracture.
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4th edition page-301]
A) Symptoms:
1. The patient most often gives a history of high-velocity trauma.
2. Usually presents in a state of hypovolaemic shock.
3. Features of shock
4. Intra-abdominal injuries.
5. Genitourinary injuries.
Clinical signs:
1. Signs of shock: Tachycardia, low BP, Cold clamy skin, Decrease urinary output,and Unconsciousness.
2. Tenderness over the fracture site.
3. Three important signs described by Milch:
a) Destot’s sign; Large hematoma above inguinal ligament or scrotum.
b) Roux’s sign: Distance from greater trochanter to pubic spine is increase on affected side. ”
4. Clinical test:
a) Compression test = + ve
b) Distraction test = + ve
c) Direct pressure test = +ve
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4th edition page-303]
Short Note:
1. Compression test: When a compressive force is applied through the two iliac bones, the patient complaints of pain in pelvic fracture.
2. Distraction test: When distraction force is applied to the two iliac bones at the anterosuperior iliac spine The pelvic fracture patients complaints of pain,
3. Direct pressure test: Direct pressure over the symphysis pubis elicits pain of pelvic fracture patients.
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4th edition page-30]
Treatment methods of pelvic fracture:
A) If the patients in shock:
1) Resuscitation and other general measures, to improve the general condition of the patient,
2) Blood transfusion and other medical and surgical emergency measures are carried out.
B) Management of pelvic fracture:
1) Avulsion fracture: Conservative treatment like
- Bed rest.
- Traction.
- Physiotherapy.
- They rarely need surgery.
2) Undisplaced fracture: Respond to bed rest, traction, pelvic slings, nonsteroidal anti- inflammatory drug (NSAIDs) etc.
3) Displaced fractures: If the displacement is <2.5 cm conservative treatment from avove discussion. If displacement >2.5 cm reduction by lateral compression methods as described by Watson Jones is very helpful. Retention is by spica cast, canvas sling or external fixators.
But the fractures associated with multiples system injuries need to be stabilized either by external fixators or by open reduction and internal fixation (ORIF).
These two methods have the following advantages:
a) Gives firm stability.
b) Helps early mobilization.
c) Reduces period of bed rest.
d) Helps early control of osseous bleeding.

[Ref-John Ebnezar’s “Textbook of Orthopedics” 4th edition page-304-306)
Complications of pelvic fracture:
1) Hemorrhage: It is usually intra-abdominal and the incidence is around 20 percent.
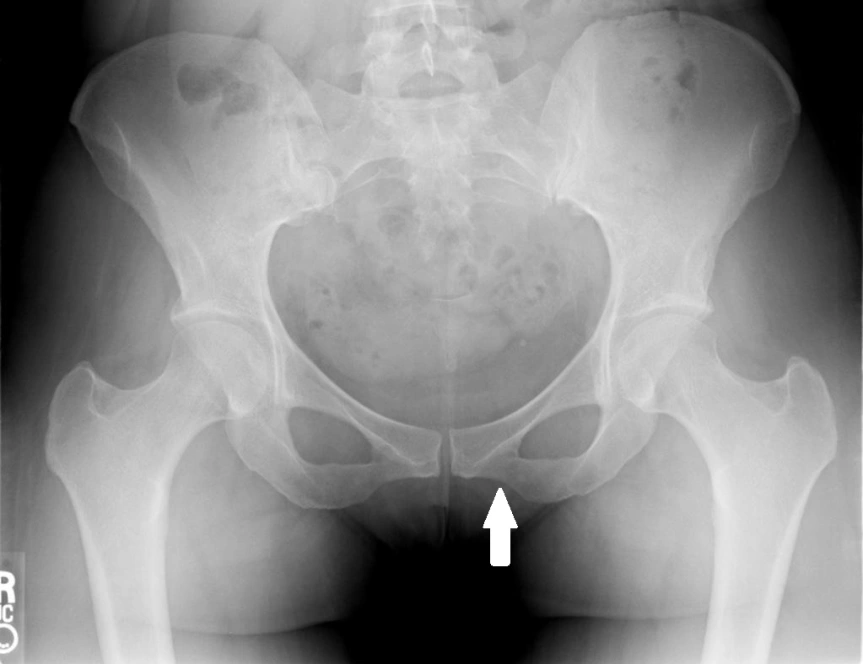
2) Injuries of lower urinary tract: Rupture of urethra and rupture of urinary bladder are the common lower urinary tract injuries frequently seen in separation of pubic symphysis and fracture pubic rami.
3) Other injuries:
- Testicular injuries,
- Vaginal lacerations,
- Bowel and rectal injuries,
- Urethral injuries.
4) Other complications:
- Loss of reduction.
- Sepsis,
- Thrombophlebitis,
- Delayed union.
- Non-union,
- Post-traumatic arthritis,
- Fat embolism,
- Major arterial injuries,
- Abdominal wall injury.
- Neurological injuries usually L5, SI roots due to sacral fracture.
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4th edition page-306]
Nursing management of pelvic fracture:
B) If the patients is in shock:
1. Checking vital signs frequently until stable.
2. Assess for ABC-If needed give it.
3. Check GCS level of the patients,
4. Opening an I/V channel give Hartman solution /Blood transfusion to prevent hypovolaemia.
5. Assess for any external bleeding-if present stop it.
6. Check urinary output every hourly and also great concern on color of urine because it may mixed with blood mixed due to pelvic injury.
7. Give Antibiotics, ATS, AGGS, painkiller etc.
8. Inspect the patients for head, neck, abdomen, chest injuries.
9. Carry out X ray on the pelvis to detect severity of fracture.
C) Nursing care once the patients is stable:
1. Care of the back: Keeping the back dry, turning the patient 2 hourly, Applying back message, apply powder on the bony prominences.
2. Care of the bladder: catheterized the patients with Foleys catheter, Check color of urine, Monitor daily output, clean the catheter every 3 days if long time residual.
3. Care of the bowel: Bad pen should be given catiously, without causing stress on the fracture area.
4. Prevention of DVT: Ensuring active exercise on the toes, foot,ankles, knees. Massaging the calf muscle. All are prevent venous stasis in the leg there by prevent DVT.
5. Prevention of fat embolisms: If restlessness, disorientation, tachycardia found, immediately inform the doctors.
6. Sponge bath the patients everyday, keep nail short, hair washed, Perineal area clean.
7. Institute active exercise on the unaffected joints and isometric exercise to the affected extremity.
8. Give mental support to the patients to reduce the anxiety.
[Ref-BT. Basavanthappa, Orthopedics for nurses, Page-315-316]