Hip arthoplasty – An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Define arthroplasty:
Arthroplasty is an orthopedic surgery where the articular surface of a musculoskeletal joint is replaced, remodeled, or realigned by osteotomy or some other procedure. It is an elective procedure that is done to relieve pain and restore function to the joint after damage by arthritis or some other type of trauma.
Or
[Reference: en.wikipedia.org]
An arthroplasty is the surgical formulation or reformation of a joint. [Ref-Adult orthopedic Nursing, Lippincott, P-295)
Or
Arthoplasty is a procedure of orthopedic surgery in which the arthritic or disfunctional joint surface is replaced with an orthopedic prosthesis.
[Ref- Marry powell, Orthopedic Nursing and rehabilitation,, Page95]
Or
Arthroplasty is an operation to construct a new mobile joint. [Ref-John Ebnezar’s, “Textbook of Orthopedics”, edition, P-370/
Or
Arthroplasty means that the joint has been re-made, often by the employment of a implant to replace one or more of the joint components.
[Ref-J N ASTON’s, “Orthopedics and Traumatology”, 2nd edition]
Aims of arthroplasty:
1. To relive pain.
2. To retain or restore movement
3. To correct deformity.
4. To restore joint function.
5. To re fashioning of joint.
[Ref-Appleys System of orthopedic and fracture, 9th edition]
The followings are the indications of arthroplasty:
1. Osteoarthritis (OA).
2. Rheumatoid arthritis (RA).
3. Avascular Necrosis (AV) of the head of femur.
4. Failed hemi replacement arthroplasty.
5. Ankylosed hip.
6. Tuberculosis of hip.
7. Frozen Shoulder & Lose shoulder.
8. Traumatized and malignant joint.
9. Acetabular dysplasia (shallow hip socket).
10. Osteonecrosis.
[Ref-John Ehnezar’s, “Textbook of Orthopedics”, ” edition]
There are three methods of arthroplasty:
These are given bellow:
1. Excision arthroplasty (Girdlestone): Here one or both the articular surfaces are excised; fibrous tissue fills up in the gap thus created and provides mobility. It usually done in hip, elbow and metatarsophalangeal joint of the great toe.
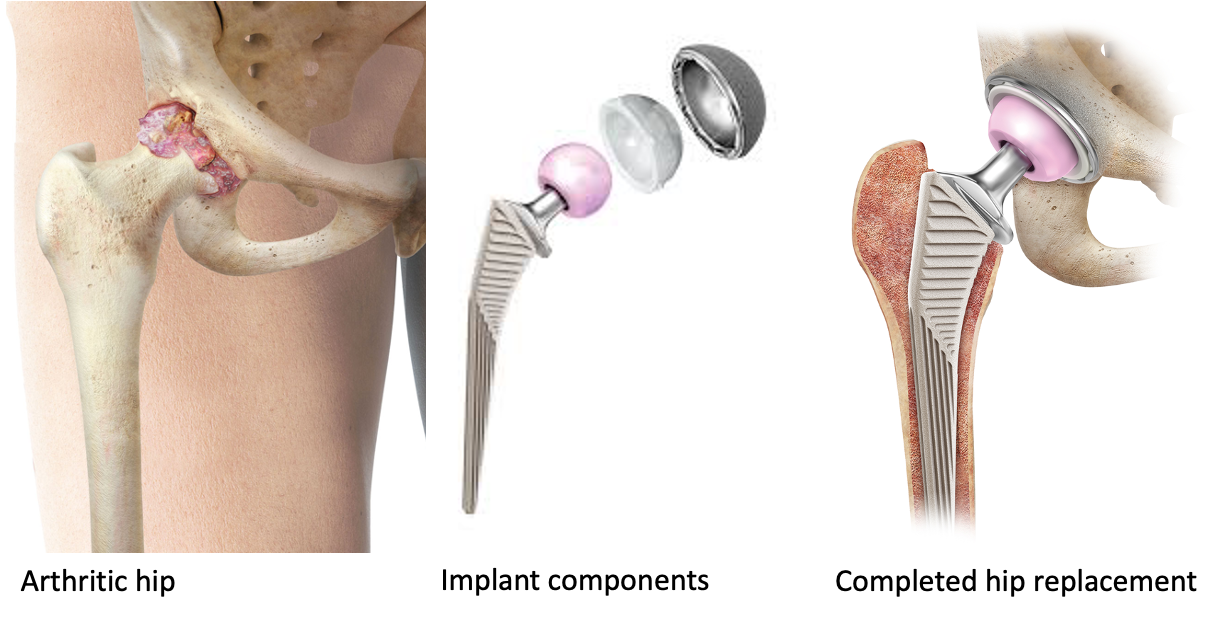
2. Hemireplacement arthroplasty: Either of the articulating surfaces is removed or replaced by prosthesis of similar shape and size, e.g. Austin Moore’s prosthesis in the fracture neck nonunion. Here one of the articular surface is excised and replaced with prosthesis. Other normal articular surface is left behind.It is commonly done in hip joint where in femoral head is removed and prosthesis is placed.
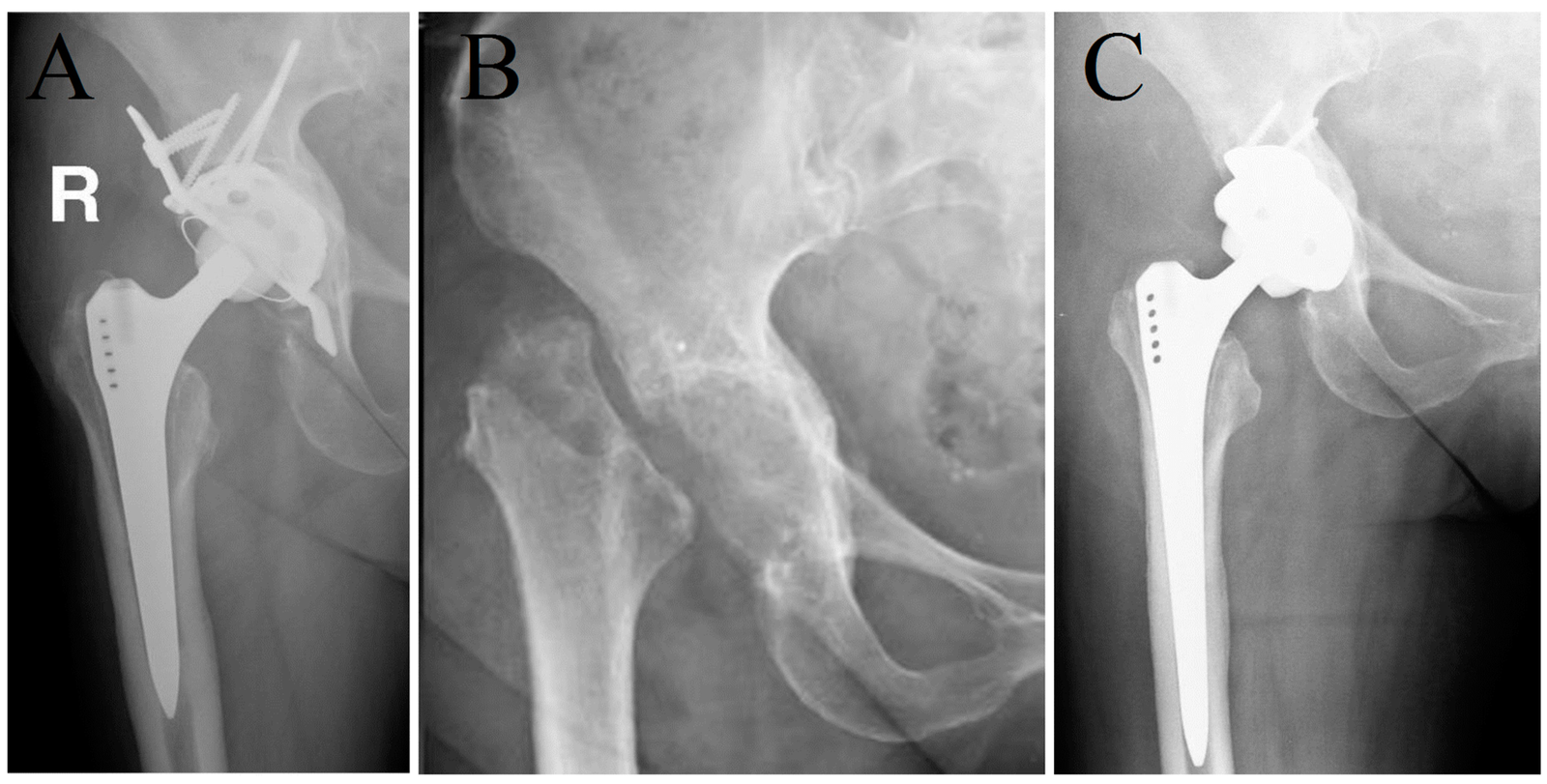
2. Hemireplacement arthroplasty: Either of the articulating surfaces is removed or replaced by prosthesis of similar shape and size, e.g. Austin Moore’s prosthesis in the fracture neck nonunion. Here one of the articular surface is excised and replaced with prosthesis. Other normal articular surface is left behind.It is commonly done in hip joint where in femoral head is removed and prosthesis is placed.
3. Total replacement arthroplasty: Here both the articular surfaces are excised and replaced by prosthetic components; the larger joint is replaced by a metallic prosthesis and the smaller joint by high density polyethylene. Both the components are fixed byacrylic cement, e.g. total hip replacement for advanced intractable osteoarthritis or rheumatoid arthritis. It is commonly done in hip joint. Often used in knee and other joint.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, edition, P-370,371+ SRBS Surgery for nurses, P-441,442]
Complications of Arthroplasty:
1. DVT (Deep vein thrombosis)
2. Fat embolisms
3. Infection
4. Breakage of implants.
5. Lossening of implants.
6. Osteolysis.
7. Periprosthetic fracture.
8. Dislocation.
9. Heterotrophic ossification
10. Vascular or nerve injuris.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, 4 edition, P-817]
Or
A) Medical risk:
1. Heart attack.
2. Stroke
3. Venous thromboembolisms.
4. Pneumonia
5. Urinary tract infection.
B) Intraoperative risk:
1. Malpositioning of components,
a) Shortening
b) Instability.
c) Dislocation
d) Fracture of adjacent bone.
2. Nerve damage and blood vessels.
C) Immediate Risk:
1. Infection: Deep, superficial.
2. Dislocation
D) Late risk:
1. Loosening of component
2. Polythene synovitis.
Common arthroplasty done in orthopedic surgery unit:
1. Hip arthroplasty (total or hemi arthroplasty).
2. Knee arthroplasty.
3. Ankle arthroplasty.
4. Shoulder arthroplasty.
5. Metacarpophalangeal arthroplasty.
Hip arthoplasty
Hip arthroplasty is the surgical formulation or reformation of hip joint.
Indications of Total hip arthroplasty:
1. Age 60 years
2. Indicated to younger patients with destructive hip disorder.
3. Children severely crippled with rheumatoid diseases.
[Ref-Appleys, System of orthopedic and fracture, P-537]
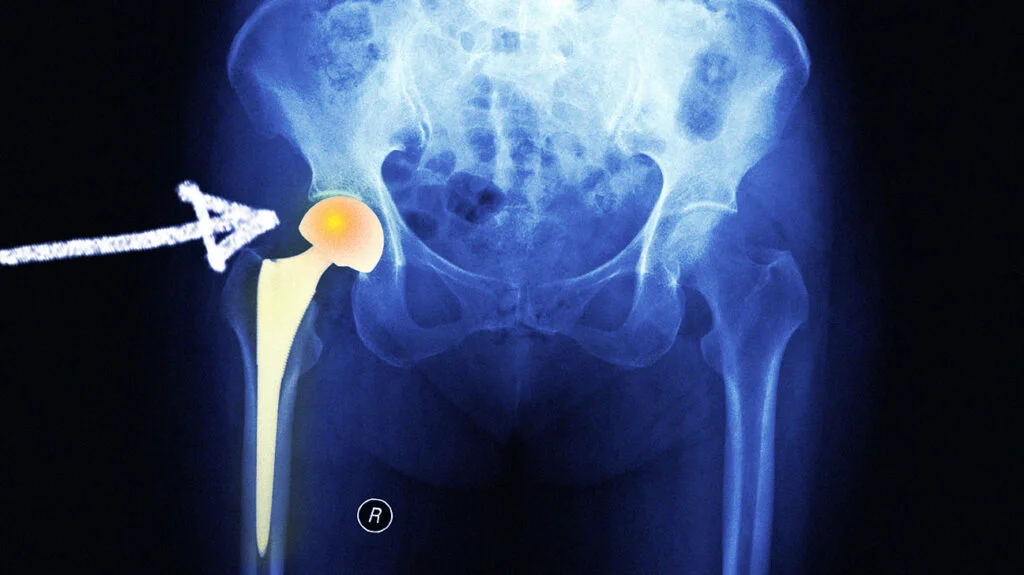
Types of hip arthroplasty:
1) Cup or mold arthroplasty: In cup arthroplasty, the acetabulum and the head of femur are reamed down to an un traumatized surface and an appropriate size metal cup is fitted over the head of femur
2) Total hip arthroplasty: In total hip arthroplasty, the femoral head and neck, ream the femoral canal and insert a metal femoral component (which includes head neck and steam) into the femoral shaft.
[Ref-Lippincott, Adult orthopedic Nursing, P-295]

Nursing management of a total hip arthroplasty patients:
1) Assessment:
a) Immediately after operation patients should be assessed for any evidence of 2)shock or cardio- pulmonary abnormality.
b) Check blood pressure due to risk of hypotension.
c) Assess central venous pressure(CVP)
d) Check urinary output.
e) Look for DVT(deep vein thrombosis.)
f) Assess neurovascular status involved in leg.
g) Observe the correct alignment of the leg.
h) Check for any complication already developed
2) Nursing diagnosis:
a) Pain and discomfort related to surgery and soft tissue trauma. b) Impaired physical mobility related to instability in the hip joint.
c) Impaired skin integrity related to immobility.
d) Anxiety related to knowledge deficit and rehabilitation process.
e ) Risk of development of infection due to lack of care.
3) Nursing intervention:
a) Alleviation of pain:
i) Assess the level of pain and find out the cause of pain.
ii) Keep the patients as comfortable position.
iii) Keep the Hip join in correct alignment.
iv) Encourage the patients to use the relaxation technique such as deep breathing, listening song, watching TV.
v) Give analgesics according to doctor order and monitor relief of pain outcome.
b) Improve physical mobility:
i) Immobilized the hip joint by splint or cast to prevent further complications.e.g. dislocation of hip.
ii) Maintain in correct positions in internal rotation,adduction, and hyperflexion.
iii) Allow the patients to turn in opposite or unaffected side.
iv) Use pillows or an an abductor pillow betweens the patient leg to keep the patients legs in abduction.
v) Mild active and passive exercise (Active ROM ankle, ankle pumps,quadriceps and gluteal setting exercise) are carried out every 2 hours while the patients is awake.
vi) Assist in daily activities
vii) Sitting in chair may be started as early as the 1 or 2 postoperative day.
viii) The hip should not be flexed more than 90 degrees and bending forward when getting out of a chair.
ix) Hip should be keept higher than the knee.
x) Bathroom privileges, which allows the use of the toilet stool, require the use of an elevated seat.
xi) Patients with anterior arthroplasty are allowed to sit erect with 90 degrees of flexion at the hip posoperatively.
c) Maintaining skin integrity:
i) Observe the bony prominence of back.
ii) Change the position 2 hourly.
iii) Assess signs and symptoms of bed sores.
iv) Give back message to improve circulations.
v) Give cotton pad under the bonny prominence to reduce chance of pressure sores.
vi) Keep linen dry free of wrinkles.
vii) Keep the bony prominent soft by applying lubricate or powder.
viii) Keep the patients well hydrated and maintain well balance diet.
d) Reducing anxiety:
i) Assess the cause of anxiety.
ii) Assurance of the patients that he will cure readily.
iii) Tell him that nurses and doctors will do the best.
iv) Encourage the patients and family to verbalize questions.
v) Encourage to use relaxation technique, such as exercise, deep breathing, listening song, watching movie.
[Ref- Adult orthopedic Nursing, Lippincott, P-300]
Preoperative care for total replacement surgery:
1) Assess the client’s knowledge and understanding of the planned operative procedure. Provide further explanations and clarification as needed. It is important that the client have a clear and realistic understanding of the surgical procedure and expected results. Knowledge decreases anxiety and increases the client’s ability to assist with postoperative care procedures.
2) Obtain a nursing history and physical assessment, including range of motion of the affected joints. This information not only allows nurses to tailor care to the needs of the individual but also serves as a baseline for comparison of postoperative assessment data.
3) Explain necessary postoperative activity restrictions. Teach how to use the overhead trapeze for changing positions, The client who learns and practices moving techniques before: surgery can use them more effectively in thepostoperative period.
4) Provide or reinforce teaching of postoperative exercises specific to the joint on which surgery is to be performed. Exercises are prescribed postoperatively to
(a) Strengthen muscles providing joint stability and support,
(b) Prevent muscle atrophy and joint contractures; and
(c) Prevent venous stasis and possible thromboembolism.
5) Teach respiratory hygiene procedures such as the use of incentive spirometry, coughing, and deep breathing. Adequate respiratory hygiene is imperative for all clients undergoing joint replacement to prevent respiratory complications associated with immobility and the effects of anesthesia. In addition, many clients undergoing total joint replacement are elderly and may have reduced mucociliary clearance.
6) Discuss postoperative pain control measures, including use of patient-controlled analgesia (PCA) or epidural infusion as appropriate. It is important for the client to understand the purpose and use of postoperative pain control measures to allow early mobility and reduce complications associated with immobility.
7) Teach or provide prescribed preoperative skin preparation such as shower, shampoo, and skin scrub with antibacterial solution. These measures help reduce transient bacteria that may be introduced into the surgical site.
8) Administer intravenous antibiotic as ordered. Antibiotic therapy is initiated before or during surgery and continued postoperatively to further reduce the risk of infection.

Postoperative care for a total replacement surgery:
1) Check vital signs, including temperature and level of consciousness, every 4 hours or more frequently as indicated. Report significant changes to the physician. These routine assessments provide information about the client’s cardiovascular status and can give early indications of complications such as excessive bleeding, fluid volume deficit,and infection.
2) Perform neurovascular checks (color, temperature, pulses and capillary refill, movement, and sensation) on the affected limb hourly for the first 12 to 24 hours, then every 2 to 4 hours. Report abnormal findings to the physician immediately. Surgery can disrupt the blood supply to or innervation of the affected extremity. If so, rapid intervention is important to preserve the function of the extremity.
3) Monitor incisional bleeding by emptying and recording suction drainage every 4 hours and assessing the dressing frequently. Significant blood loss can occur with a total joint replacement, particularly a total hip replacement.
4) Reinforce the dressing as needed. The dressing is usually changed 24 to 48 hours after surgery but may need reinforcement if excess bleeding occurs.
5) Maintain intravenous infusion and accurate intake and output records during the initial postoperative period. The client is at risk for fluid volume deficit in the initial postoperative period because of blood and fluid loss during surgery, as well as the effects of the anesthetic.
6) Maintain bed rest and prescribed position of the affected extremity using a sling, abduction splint, brace, immobilizer, or other prescribed device. Proper positioning of the affected extremity is vital in the initial postoperative period so that the joint prosthesis does not become dislocated or displaced.
7) Help the client shift position at least every 2 hours while on bed rest. Shifting of position helps prevent pressure sores and other complications of immobility.
8) Remind the client to use the incentive spirometer, to cough, and to breathe deeply at least every 2 hours. These measures are important to prevent respiratory complications such as pneumonia.
9) Assess the client’s level of comfort frequently. Maintain PCA, epidural infusion, or other prescribed analgesia to promote comfort. Adequate pain management promotes healing and mobility.
10) Help the client get out of bed as soon as allowed. Teach and reinforce the use of techniques to prevent weight bearing on the affected extremity, such as the over-head trapeze, pivot turning, and toe-touch. Early mobility prevents complications such as pneumonia and thromboembolism, but appropriate techniques must be used to prevent injury to the operative site.
11) Initiate physical therapy and exercises as prescribed for the specific joint replaced, such as uadriceps setting. leg raising, and passive and active range-of-motion exercises. These exercises help prevent muscle atrophy and thromboembolism and strengthen the muscles of the affected extremity so that it cansupport the prosthetic joint.
12) Use sequential compression devices or antiembolism stockings as prescribed. These help prevent thromboembolism and pulmonary embolus for the client who must remain immobile following surgery.
13) For the client with a total hip replacement, prevent hip flexion of greater than 90 degrees or adduction of the affected leg. Provide a seat riser for the toilet or commode. These measures prevent dislocation of the joint.
14) Assess the client with a total hip replacement for signs of prosthesis dislocation, including pain in the affected hip or shortening and internal rotation of the affected leg.
15) For the client with a total knee replacement, use a continuous passive range-of-motion (CPM) device or range-of- motion exercises as prescribed. Dislocation is not a problem with a knee replacement, and more emphasis is placed on range-of-motion exercises in the early postoperative period.
16) Maintain fluid intake and encourage a high-fiber diet. Administer stool softeners or rectal suppositories as needed. Immobility contributes to the potential problem of constipation; these measures help maintain regular fecal elimination.
17) Encourage consumption of a well-balanced diet with adequate protein. Adequate nutrition promotes tissue healing.
18) Teach or reinforce postdischarge exercises and activity restrictions. Emphasize the importance of scheduled follow up physician visits. Clients are discharged from the acute care facility before healing is complete. Exercises are prescribed and activities are resumed gradually to protect the integrity of the joint replacement and prevent contractures.
19) For those clients needing additional direct care after discharge, arrange placement in a long-term care or rehabilitation facility. Activity restrictions may preclude discharge to home for some clients.
20) Make referrals as needed to home health agencies and physical therapy. Clients often require home health care for both nursing care needs and continued physical therapy following discharge from acute or long-term care.