Rheumatoid Arthritis -An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Rheumatoid Arthritis
Rheumatic Diseases
It is a heterogenous group of disorders of connective tissue, joints and bones in which musculo-skeletal pain and stiffness are prominent.
Classification of rheumatic diseases
A) Inflammatory joint diseases:
1) Rehumatoid arthritis.
2) Ankylosing spondylitis,
3) Reiters arthritis.
4) Psoriatic arthritis.
5) Enteropathic arthropathy.
6) Whipples diseases.
B) Infective arthritis:
1) Bacterial.
2) Viral.
3) Fungal.
C) Connective tissue diseases:
1) Syestemic lupus erythematous.
2) Polyarthritis nodusa.
3) Polymyositis.
4) Giant cell arteritis.
D) Crystal deposition:
1) Gout.
2) Chondrocalcinosis.
E) Osteoarthritis.

Investigations done in rheumatic diseases:
1) Haematology
2) Serologic test:
a) Rheumatoid factor
b) Antinuclear antibody
c) Antiphospolipid antibodies.
3) Biochemical test
4) Synovial fluid analysis
5) Arthroscopy
6) Imaging: X-ray, CT scan, MRI
7) ESR, CRP, Hb% etc.
Some Rheumatological term:
- Monoarticular-One joint involved
- Polyarticular – Many joint involved
- Oligoarticular-2-4 joint involved
- Arthralgia – Joint pain without swelling.
- Migratory – Arthritis moving from join to join.
- Seropositive – Rheumatoid factor positive
- Sero negative – Rheumatoid factor negative.
Arthritis:
Inflammation of the joint causes pain and swelling called arthritis.
Types of arthritis:
1. Monoarthritis.
2. Oligoarthritis.
3. Polyarthritis.
- Monoarthritis: Inflammation of one joint.
- Causes of monoarthritis:
1. Traumatic sprained ankle
2. Septic arthritis
3. Tubercular arthritis
4. Gout or pseudogout
5. Haemophilia
- Polyarthritis: Inflammation of more than 4 joints.
- Causes of polyarthritis:
1) Rheumatoid arthritis.
2) Ankylosing spondylitis.
3) Juvenile arthritis.
4) Psoriatic arthritis.
5) Gout.
6) Rheumatic fever

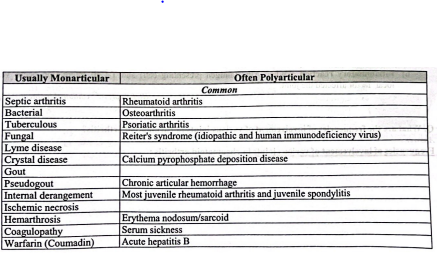
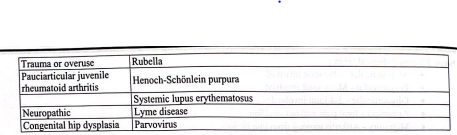
Differential diagnosis of monarticular arthritis:
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic systematic inflammatory diseases characterized by recurrent inflammations involving the synovial membrane or linings of the joints and leading to destructive changes in the joints.
Or
Rheumatoid arthritis is a systemic disease of young and middle aged adults characterized by proliferate and destructive changes in synovial membrane, particular structures, skeletal muscles and perineural sheaths. It is the most common inflammatory disease of the joints.

Etiology of rheumatoid arthritis:
1) Age: most common in 3 & 5th decade.
2) Sex: female male ratio 3:1
3) Genetic susceptibility: Rheumatoid arthritis (RA) is more common in 1″ degree relatives of pts than in large population. Again who has HLA-DR4 antigen are 70% risk for RA.
4) Rheumatoid factor.
5) Virus: Rubella virus, Epstein barr virus.
6) Inflammatory reaction: When APC (antigen presenting cell) and T-Cell interaction occur various local factor affected the joint.
[Ref-Applys- edition+Lippincott- 44 page]
Frequencies of involvement of various joints in rheumatoid arthritis:
- Temporomandibular: 30%
- Cervical spine: 40%
- Shoulder: 60%
- Sternoclavicular: 30%
- Acromio-clavicular: 50%
- Cricoarytenoid: 10
- Elbow: 50%
- Wrist: 80%
- MCP’sand IP’s: 90%
- Hip: 50%
- Knee: 80%
- Ankle: 80%
- MTP’s: 90%
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, 4 edition, P-584]
Clinical feature of rheumatoid arthritis:
A) Symptoms:
1) Joint pain:
a) Initially pain on movement but later pain on rest.
b) Pain occurs on small joint of fingers and toes.
2) Joint swelling:
a) Symmetrical swelling of small joints.
b) Swelling is not migratory.
3) Stiffness of the joint: Stiffness in early morning after awakeing from sleeping.
4) Systemic symptoms:
a) Fever
b) Fatigue.
c) Wt loss.
d) Muscle wasting.
B) Signs:
1) Joint become hot swollen and tender.
2) Limitation of movement.
3) Articular signs:
a) Swan neck deformity: hyperextension of the proximal interphalangeal joint with fixed flexion of the distal interphalangeal joint.
b) Z-deformity of the thumb.
c) Button hole deformity.
d) Sublaxation of MTP (meta terso phalangeus) with ulner deviation.
e) Rheumatoid nodule.
f) Clawing of the toes.

Extra-articular or non-articular features of rheumatoid arthritis:
1) Systemic:
i)Fever.
ii) Weight loss,
ⅲ) Fatigue,
iv) Susceptibility to infection.
2) Musculoskeletal:
i) Muscle wasting.
ii) Tenosynovitis.
ⅲ) Bursitis.
iv) Osteoporosis.
3) Hematological:
i) Anemia,
ii) Thrombocytosis.
ⅲ)Eosinophilia.
4) Lymphatic:
i) Felty’s syndrome,
ii) Splenomegaly.
5) Nodules:
i) Sinuses,
ⅱ) Fistulae.
6) Ocular:
i) Episcleritis.
ii) Scleritis.
ⅲ)Sclefomalacia.
iv) Keratoconjuntivitis sicca.
7) Vasculitis:
i) Digital arteritis.
ii) Ulcers.
ⅲ)Pyoderma gangrenosum.
iv) Mononeuritis mutiplexa.
v) Visceral arteritis.
8) Cardiac:
i) Pericarditis.
ii) Myocarditis.
ⅲ) Endocarditis.
iv) Conduction defects.
v) Coronary vasculitis.
vi) Granulomatous aortitis.
9) Pulmonary:
i) Nodules,
ii) Pleural effusions,
ⅲ)Fibrosing alveolitis.
iv) Bronchiolitis.
v) Caplan’s syndrome.
10) Neurological:
i) Cervical cord compression,
ii) Compression neuropathy.
ⅲ)Peripheral neuropathy,
iv) Mononeuritis multiplex.
11) Amyloidosis.
[Ref-Davidson’s, “Principles and Practice of Medicine”, 21″ edition, Page-1090]
Diagnostic criteria of RA:
According to the American college of rheumatology in 1987:at least 4 out of 7 criteria fulfill the diagnosis of Rheumatoid arthritis
1. Morning stiffness for minimum one hour everyday, at least for six weeks
2. Arthritis or swelling of 3 or more joints for greater than 6 weeks.
3. Arthritis or swelling of hand joints(wrist, metacarpal) for more than 6 weeks.
4. Symmetrical of swelling more than 6 weeks
5. Serum rheumatoid factor present.
6. Rheumatoid nodules.
7. Radoigraphics features of RA.
[Ref-John Ebnezar, edition.p-583]

Investigations for rheumatoid arthritis:
1. Blood: Hb%- normochromic normocytic anaemia
- ESR-increased
- CRP-increased
- Lymphocytosis
2. Serological test:
a) a) Rose waler test +ve in 70% cases
b) b) Anti nuclear factor(ANA) +ve in 30% cases
c) c) Rheumatoid factor +ve
d) Latex test
e) Inhibition test
3. X-ray findings
a) Soft tissue swelling
b) Joint spaces are decreased
4. Synovial fluid analysis: typically yellow, watery and turbid due to high WBC and has a longer sugar contents.
5. Arthroscopy
6. MRI
Radiological features of rheumatoid arthritis:
1. Soft tissue swelling.
2. Juxta-articular osteoporosis.
3. Erosion of joint margins.
4. Joint spaces are decreased.
5. Deformities.
6. Atlantoaxial subluxation.
7. Subchondral erosions and cyst formation.
8. Fibrous and bony ankylosis develops in the late stages.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, 4 edition, Page-586]
The following deformities are very common seen in the hand:
1. Symmetrical peripheral joint swelling of metacarpophalangeal (MCP) joints.
2. Ulnar deviation of the hand.
3. Boutonniere’s deformity.
4. Swan neck deformity.
5. Trigger fingers and trigger thumb.
6. Subluxation and dislocation of metacarpophalangeal joints.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, edition, Page-584-385]
Common foot deformities in rheumatoid arthritis:
1. Callosity under PIP joint
2. Planter callosity
3. Atrophy of the planter metatarsal fat pad.
4. Prominent metatarsal head.
5. Claw toes
6. Hammer toes.
7. Rehumatoid nodules.
8. Achilles tendinitis
9. Flattening of longitudinal arch.
10. Bunion.
11. Hallux valgus.
12. Over-riding of second and third toes. 13. Splaying of forefoot due to divergent metatarsals.
[Ref-John Ebnezar’s, “Textbook of Orthopedics”, edition, Page-585]

Management of rheumatoid arthritis;
i. Using western toilets, Bath aids and railings,
ii. Mop to clean the floors,
iii. Use of walking sticks while walking, climbing etc.
[Ref-John Ehnezar’s, “Textbook of Orthopedics”, edition, Page-587-589]
Prognoses of RA
1. 25% will have complete remission of symptoms regain fit for all normal activities. 2. 40% will have only moderate function despite exacerbation remission of diseases
3. 25% will be more severely disable.
4. 10% will be severely crippled.
[Ref-Davidsons, principales and practice of medicine, 21 th editionPage 862]
Surgical treatment of rheumatoid arthritis:
The following are some of commonly performed surgical methods in rheumatoid arthritis:
1) Synovectomy for inflamed joints.
2) Tenosynovectomy for inflamed tendon sheaths.
3) Osteotomy.
4) Arhtrodesis (Fusion) finger joints (IPIs), Wrist, spine, ankle and hindfoot.
5) Joint replacement (hip, knee, elbow, shoulder and metacarpophalangeal joints).
[Ref-John Ebnezar’s, “Orthopedics for Nursex”, 1″ edition, P-391,392]
Anaemia occurs in Rheumatoid arthritis patients:
1) Fe defiency, blood loss due to:
✔NSAIDS
✔Glucocorticoids
2) Folic acid deficiency.
3) Defective Fe utilization.
4) Hypoplasia of bonemarrow.
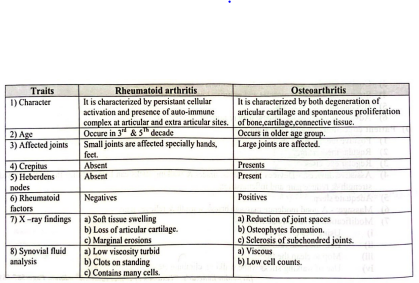
Difference between Rehumatoid arthritis and osteoarthritis:
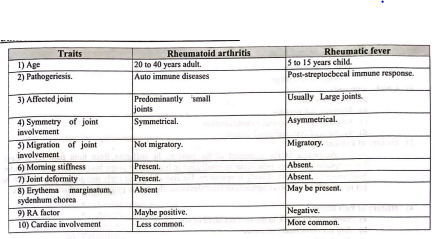
Difference between Rheumatic arthritis and Rheumatic fever :
Complications of rheumatoid arthritis:
A) General health deterioration:
1) Weight loss.
2) Anaemia.
3) Depression.
B) Articular complications:
1) Septic arthritis.
2) Deformity.
3) Sublaxation.
4) Synovial sac rupture(e.g.Barkers cysts).
5) Tendon rupture.
C) Extra articular complications
1) Osteoporosis & muscle atrophy
2) Pulmonary:
a) Pleural effusion
b) Pleurisy
c) Fibrosing alveolitis
3) Cardiac:
a) Pericarditis
b) Heart block.
a) Scleritis
b) Sjogren Syndrome
4) Ocular:
5) Arterial: Leg ulcer.
6) Lymphadenopathy.
7) Peripheral & autonomic neuropathy
Clinical assessment of a pts who suffering from Rheumatoid arthritis:
1) Particulars of the pts: as usual
- Age:
- Sex:
- Address:
- Date of admission:
- Date of discharge:
2) Chief complaints:
a) Joint pain (for..
b) Morning stiffness(for.
c) Features of extra articular manifestation
d) Features of systemic involvement.
3) History of Present illness:
According to the statement of the patients, he suffering from joint pain for 8 days. He complaints that joint pain occur in small joint in hands. later joints become hot swollen tender, Sometimes he fells rise of body temperature. He also added that early morning stiffness when he get up from his bed. No complaints of breathlessness, chest pain, palpitation, redness of eyes etc.
4) History of Past illness:
a) Same type of attack in the past occurred or not.
b) Any previous injury of joints
c) Any heart diseases.
5) Family history: same type of illness in his family is present or not.
6) Personal history:
✔ Occupations-
✔Dietary history
✔Habit-smoking alcohol drinking
✔History of immunization-
7) Drug history: H/o of taking NSAIDs, steroids etc
8) Systemic questioning:
- General-wt,sleep.energy
- GIT-pain, vomiting.constipation
- CVS-Dyspnoea,chest poin palpitation, ankle oedema
- Respiratory system-breathlessness.cough,sputum
9) General examinations:
✔Appearance-ill looking
✔Anaemia- present
✔Jaundice present
✔Cyanosis-absent
✔Clubbing-absent
✔Koilonychea- absent
✔Pulse-normal
✔blood pressure- normal Temperature-increased
✔Respiration -normal
✔Lymphnode- enlarged
✔Weight – decrease
✔Deformities hand deformity present.
✔Tremor-absent.
10) Systemic examinations:
A) Locomotor system:
a) Knee joint:
- Inspection:
- Swollen
- Red skin
- Scar
- Muscle wasting
- Deformity
Palpation:
✔Raise local temperature
✔Tenderness
✔Restriction of movement
✔Patellar tap
✔Bony crepitus
b) Interphalangeal joint:
- Swan neck deformity
- Button neck deformity
- Z- deformity of thumb
B) Cardi ovascular system:
a) Inspection:
- Visible apical impulse
- Any visible swelling
- Any scar mark of chest
b) Palpation:
✔ Apex beat
✔Lt parasternal heave
✔Thrill
C) Respiratory system: usually normal
D) Alimentery system usually normal
E) Dermatological system: Rheumatoid nodule
F) Ocular system:
✔ Seleritis
✔Episcleritis
✔Iritis
11) Provisional diagnosis: A case of polyarthritis due to rheumatoid arthritis
12) Confirm diagnosis: Done by laboratory investigations
Nursing management of Rheumatoid arthritis:
A) Nursing assessment:
1) Assess pain using pain measuring scale.
2) Assess sign symptoms of inflammations: tenderness, swelling.redness
3) Presence of joint deformity:
✔Swan neck deformity
✔Ulnar neck deformity
✔Rheumatoid nodule
✔ Carpal tunnel syndrome
4) Measuring body temperature
B) Nursing diagnosis:
1) Pain due to inflammation of the joint
2) Impaired physical mobility related to limited joint movement joint pain
3) Knowledge deficit related to lack of information about management.
4) Ineffective coping related to pain in the joints.
5) Altered body temperature related to inflammation of the joints.
C) Nursing interventions:
1) Controlling pain:
a) Apply local heat or cold to affected joints for 15 to 20 minutes 3 times daily
b) Encourage pain controls measures:
✔ Progressive muscle relaxation.
✔Biofeedback
✔Meditation
✔ Acupuncture or same therapies
c) Give medications according to doctor order c
d) Monitor pain remedy procedure.
e) Encourage exercise consistent with degree of diseases activity.
2) Optimizing mobility:
a) Encourage warm bath or shower in the morning to decrease morning stiffness.
b) Encourage measures to protect affected joints
i) Perform gentle ROM exercise.
ii) Use splints
ⅲ) Assist with ADLs if necessary.
c) Refer to physical therapy and occupational therapy.
3) Providing knowledge of diseases processes and management
a) Positive mental attitude
b) Regular medication
c) Regular exercise: pts should follow aregular and appropriate exercise programme.
d) Use of joints The patients is told the value of correct posture and the methods of using the joint
e) Energy conservation: patients are instructed to listen to the bodys inner signals for rest.
f) Assistive device: Devices likes splints, braces and walking sticks can help the stabilize the joints. And reduce pain.
g) Adequate sleep: a good sleep provides rest to the alling joints and reduce pain and swelling.
h) Massage: A good moderate massage brings warmth and relief pain due to arthritis.
i) Relaxation technique: yoga, meditation etc helps to relax the muscle.
j) Modification in the daily activities:
✔Using western toilet
✔Bath aids and railings
✔Use walking sticks while walking.climbing
✔High chair
✔Use of dining table and chairs
✔ To sleep in hard surface.
4) Strengthening coping skills:
a) Encourage patient vocalize problem and feelings.
b) Assist with problem solving approach to explore options and controls of problem.
c) Reinforce effective coping mechanisms.
d) Tell that diseases will cure quickly.
e) Deep breathing when more tensions.
5) Reduce body temperature:
✔ Assess body temperature.
✔Rapid sponging.
✔Plenty of fluid.
✔Give anti pyretics.
✔Monitor body temperature.