Congenital anomalies – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric- nursing.
Pediatric-nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric-nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Congenital anomalies
Congenital anomalies are also known as birth defects, congenital disorders or congenital malformations. Congenital anomalies can be defined as structural or functional anomalies (for example, metabolic disorders) that occur during intrauterine life and can be identified prenatally, at birth, or sometimes may only be detected later in infancy, such as hearing defects. In simple terms, congenital refers to the existence at or before birth.
Congenital anomalies are important causes of infant and childhood deaths, chronic illness and disability.
Definition of Congenital Anomalies:
According to WHO (World Health Organization): Congenital anomalies are also known as birth defects, congenital disorders or congenital malformations. Congenital anomalies can be defined as structural or functional anomalies (for example, metabolic disorders) that occur during intrauterine life and can be identified prenatally, at birth, or sometimes may only be detected later in infancy, such as hearing defects.
(Ref by- http://www.who.int)
Risk Factors of Congenital Anomalies:
| Socioeconomic and demographic factors: |
|
| Genetic factors: |
|
| Infections: | Some Maternal infections during pregnancy can increase the risk of birth defects such as:
|
| Maternal nutritional status and medical conditions: |
|
| Environmental factors: |
|

Etiology/Causes of Congenital Anomalies;
Genetic factors -25%
A. Chromosomal defect:
a) Trisomy 21 or Down syndrome
B. Gene defect:
a) Single gene defect or unifactorial;
- Sickle cell anemia
- Polycystic kidney disease
b) Multifactorial:
- Diabetes mellitus
- Cleft lip/cleft palate
Environmental factors:
a) Intrauterine infections especially by STORCH (Syphilis, Toxoplasmosis, Rubella, Cytomegalovirus and Herpes Virus).
b) Drugs intake by the mother during pregnancy like steroid hormones, stilbestrol, anticonvulsants, folate antagonists, cocaine, lithium, thalidomide, etc.
c) X-ray exposure during pregnancy.
d) Maternal diseases like diabetes, cardiac failure, malnutrition, folic acid deficiency, iodine deficiency disorders, endocrine abnormalities, etc.
e) Abnormal intrauterine environment like bicornuate uterus, septed uterus, polyhydromnios, oligohydromnios, fetal hypoxia, etc.
f) Maternal addiction with alcohol, tobacco or smoking (active or passive).
g) Environmental pollution, especially air pollution.
(Ref: Paediatric Nursing, Parul Datta/3/187)
Common Congenital Anomalies in Children:
| Congenital Heart Diseases: |
|
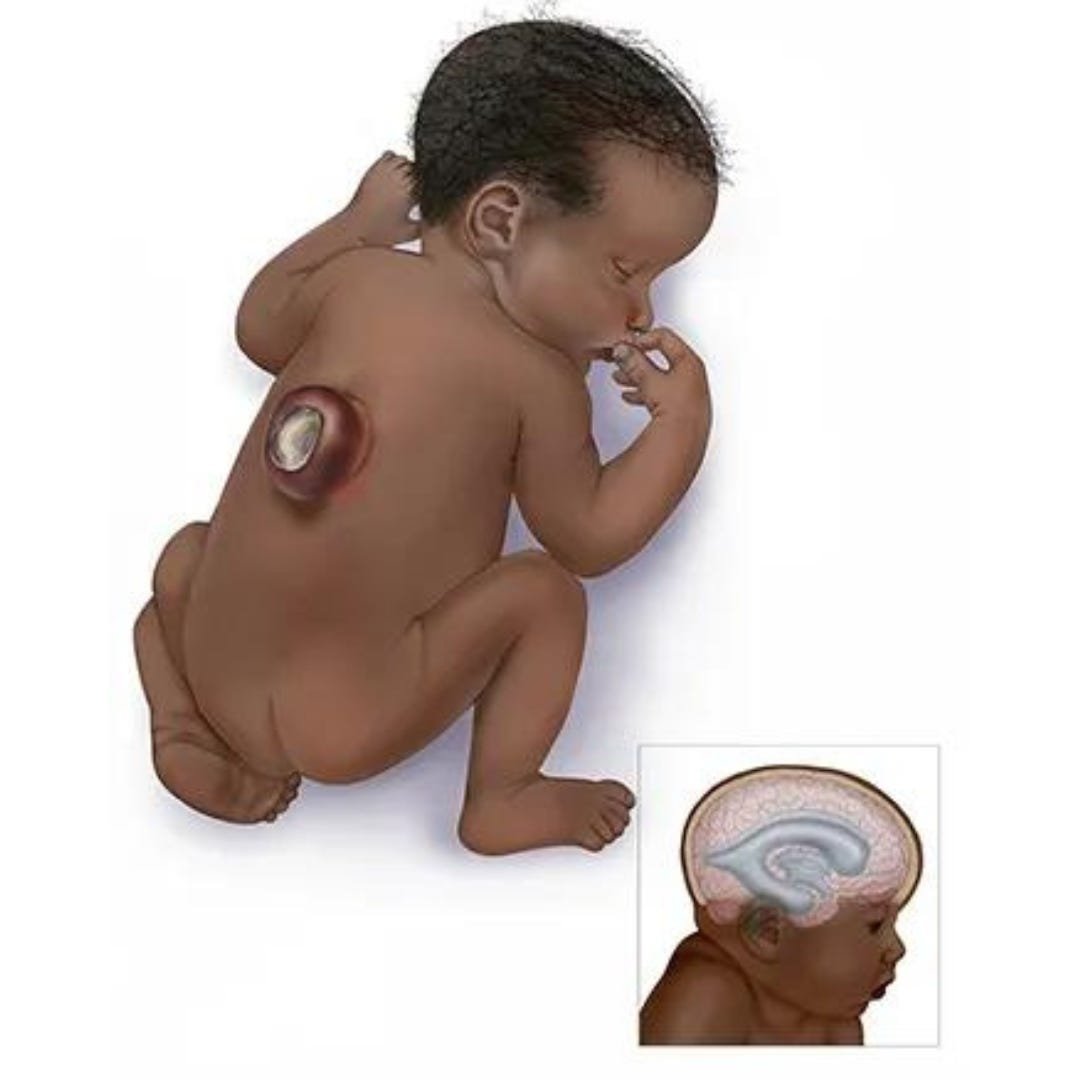
| Central Nervous System Defects: |
|
| GI System Abnormalities: |
|
| Respiratory System Abnormalities: |
|
| Abnormalities of Genitourinary System: |
|
| Musculoskeletal Abnormalities: |
|
| Blood Disorders: |
|
| Metabolic Disorders: |
|
| Endocrinal Abnormalities; |
|
| Chromosomal Abnormalities: |
|
| Miscellaneous: |
|
Preventive Measure of Congenital Anomalies:
According to World Health Organization:
Preventive public health measures work to decrease the frequency of certain congenital anomalies through the removal of risk factors or the reinforcement of protective factors. Important interventions and efforts include:
1. Ensuring adolescent girls and mothers have a healthy diet including a wide variety of
vegetables and fruit, and maintain a healthy weight;
2. Ensuring an adequate dietary intake of vitamins and minerals, and particularly folic acid in adolescent girls and mothers;
3. Ensuring mothers avoid harmful substances, particularly alcohol and tobacco; 3
4. Avoidance of travel by pregnant women (and sometimes women of child-bearing age) to regions experiencing outbreaks of infections known to be associated with congenital anomalies;
5. Reducing or eliminating environmental exposure to hazardous substances (such as heavy
metals or pesticides) during pregnancy;
6. Controlling diabetes prior to and during pregnancy through counselling, weight management, diet and administration of insulin when required;
7. Ensuring that any exposure of pregnant women to medications or medical radiation (such as imaging rays) is justified and based on careful health risk-benefit analysis;
8. Vaccination, especially against the rubella virus, for children and women;
9. Increasing and strengthening education of health staff and others involved in promoting prevention of congenital anomalies;
10. Screening for infections, especially rubella, varicella, and syphilis, and consideration of treatment

(Ref by- http://www.who.int)
Responsibility of a Nurse towards a Congenitally Abnormal Child:
The nurse is usually the first person with whom the family has contact. The nurse can help the family by the following ways –
1. Collection of detail history of prenatal, natal and postnatal period.
2. Preparation of pedigree chart by interview and home visit
3. Identification of present problems, its nature and severity, for necessary interventions.
4. Participation in diagnostic investigations, treatment, follow-up and research project.
5. Provide necessary information to the parents and family members.
6. Motivate the family members for genetic counseling and referring to the genetic clinic
7. Participating in genetic counseling process with special training, personal experience, knowledge and competency.
8. Provide emotional support and answer questions asked by the counselee
9. Guide the family for rehabilitation, of the child and for available, social and economical support.
10. Promote public awareness about the prevention of Congenital anomalies by individual or group health education or by mass media information.
(Ref: Paediatric Nursing, Parul Datta/34/192-193)
