Diabetes Mellitus – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.

Diabetes Mellitus
Definition of Diabetes Mellitus
Diabetes mellitus is a metabolic disorders characterized by hyperglycaemia with or without glycosuria due to absolute or relative deficiency of insulin.
(Ref-Davidson-798/22)
Classification of DM
A. Type I or insulin dependent diabetes mellitus (IDDM):
a) Immune mediated
b) Idiopathic
B. Type II or non-insulin dependent diabetes mellitus (NIDDM):
a) Insulin resistance.
b) Pancreatic beta-cell failure.
5 important 2ndary causes of DM:
|
C. Other specific types:
a) Genetic defects of beta cell function.
b) Genetic defect of insulin action.
c) Pancreatic disease:
- Pancreatitis.
- Pancreatectomy.
- Neoplastic disease
- Cystic fibrosis
- Haemochromatosis
- Fibrocalculous pancreatopathy
d) Excess endogenous production of hormonal antagonists to insulin:
GH hormone-Acromegaly
Glucocorticoid-Cushing’s syndrome.
Glucagon-Glucagonoma
Catecholamines-Phaeochromocytoma.
Thyroid hormone-Thyrotoxicosis.
e) Drug induced: Corticosteroid, thiazide diuretics, phenytoin
f) Viral infections: Congenital rubella, mumps, Coxackie virus B.
g) Uncommon forms of immune-mediated diabetes.
h) Associated with genetic syndromes:
- Down’s syndrome.
- Klinefelter’s syndrome
- Turner’s syndrome
- DIDMOAD/Wolfram’s syndrome:
- (Diabetes insipidus, DM, optic atrophy, nerve deafiaess, Friedreich ataxia, myotonic dystrophy)
D. Gestational diabetes mellitus.
(Ref-Davidson-807/22)

The Diagnostic Criteria for Diabetes Mellitus Recommended By
World Health Organization (WHO) in 2000 are shown in the following:
Diagnosis of diabetes mellitus
Patient complains of symptoms suggesting diabetes-
- Test urine for glucose and ketones
- Measure random or fasting blood glucose.
Diagnosis confirmed by biochemically –
- Fasting plasma glucose ≥ 7.0 mmol/L (126 mg/dl)
- Random plasma glucose ≥ 11.1 mmol/L(200 mg/dl)
In symptomatic patient: one abnormal fasting plasma glucose or Random plasma glucose value indicate Diabetes.
In asymptomatic patient: Two value are needed for diagnosis of Diabetes.
(Ref-Davidson-817/21 +ADA criteria-2011)
Clinical Feature of DM
Symptoms
A. Asymptomatic.
B. Symptomatic case
a) Polyuria.
b) Polydipsia.
c) Polyphagia.
d) Weight loss.
e) Fatigue
f) Pruritus vulvae or balanitis.
g) Dryness of the mouth & throat.
C. Pts. may come with features of complication
a) Diabetic retinopathy (visual blurring), nephropathy (with oedema).
b) Features of neuropathy: Pain, paraesthesia, muscle wasting, or loss of ankle reflexes, loss of vibration.
c) Ulcer with delayed healing.
d) Fungal infection (skin) & urinary tract infection.
e) Unconsciousness due to hypoglycaemia, ketoaci dosis, hyperosmolar non- ketotic coma, lactic acidosis.
f) Stroke
g) MI & peripheral gangrene
Sign’s
Following signs may present or associated,
A. Hand
- Dupuytren’s contracture
- Carpal tünnel syndrome
- Trigger finger/thumb
- Limited joint mobility
- Wasting of small muscles
- Sensory abnormality
B. Skin
- Bullosis
- Pigmentation
- Granuloma annulare
- Vitiligo
C. Blood pressure
- High blood pressure
D. Axilla
- Acanthosis nigricans.
E. Neck
- Carotid bruit
- Thyroid enlargement.
F. Eyes
- Ptosis
- Reduced visual acuity
- Lens opacity (cataract)
- Fundoscopy (diabetic retinopathy)
G. Insulin injection sites: Lipodystrophy
H. Abdomen
- Hepatomegaly (due to fatty change)
I. Legs
- Muscle wasting
- Sensory abnormality
- Hair loss
- Tendon reflexes – Diminished or exaggerated
J. Feet
- Sensory loss
- Ulcer
- Peripheral pulses – May be absent.
K. Others
- Low BMI (under-weight)
- Obesity in type-2 diabetes
- Mucosal candidiasis
- Dehydration
- Air hunger – Kussmaul breathing in ketoacidosis
(Ref-Davidson-809-10/22)
Clinical feature of IDDM (Type -I) & NIDDM (Type-II)
| Traits | IDDM (Type-1) | NIDDM (Type-II) |
| 1. Age of onset: | Usually < 40 years | > 50 yars |
| 2. Duration of symptoms: | Weeks | Months to years |
| 3. Body weight: | Normal or low | Obese. |
| 4. Ketonuria: | Yes | No |
| 5. Rapid death without treatment with insulin. | Yes | No |
| 6. Auto antibodies | Present(against pancreatic cells) | Absent |
| 7. Diabetic complication at diagnosis. | Absent | Present in 25% cases |
| 8. Family history of DM | Uncommon | Yes |
| 9. Acute complication | Diabetic ketoacidosis | Hyperosmolar nonketotic coma |
| 10. Other autoimmune disease | Yes | Uncommon |
(Ref by-Davidson-809/22)
Indications for oral Glucose tolerance test (OGTT)
- Fasting plasma glucose 6.1-7.0 mmol/L (110-126 mg/dl).
- Random plasma glucose 7.8-11.0 mmol/L (140-199 mg/dl
Procedure
- Unrestricted carbohydrate diet for 3 days before test.
- Fasted overnight (for at least 8 hrs).
- Rest before test (30 mins); No smoking; seated for duration of test.
- Plasma glucose measured before, and 2 hrs after 75 g glucose load.
Interpretation
Fasting hyperglycaemia
- Fasting plasma glucose 6.1-6..9 mmol/L (110-126 mg/dl).
- Random plasma glucose less than 7.8 mmol/L
Impaired glucose tolerance test
- Fasting plasma glucose 6.1-7.0 mmoVL (110-126 mg/dl).
- 2 hrs after glucose load 7.8-11.0 mmol/L (140-199 mg/dl).
DM:
- Fasting 7.0 mmol/L (126 mg/dl)
- 2 hrs after glucose load≥ 11.1 mmol/L(200 mg/dl)
(Ref-Davidson-806/21″)
Pathophysiological Condition of DM
Diabetes Mellitus has different courses of pathophysiology because of it has several types.
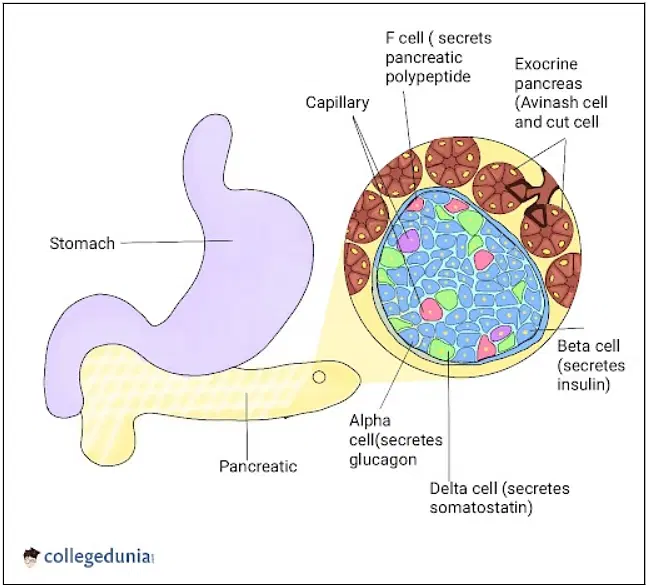
- Insulin is secreted by beta cells in the pancreas and it is an anabolic hormone.
- When we consume food, insulin moves glucose from blood to muscle, liver, and fat cells as insulin level increases.
- The functions of insulin include the transport and metabolism of glucose for energy, stimulation of storage of glucose in the liver and muscle, serves as the signal of the liver to stop releasing glucose, enhancement of the storage of dietary fat in adipose tissue, and acceleration of the transport of amino acid into cells.
- Insulin and glucagon maintain a constant level of glucose in the blood by stimulating the release of glucose from the liver.
Islet of Langerhans
Type 1 Diabetes Mellitus
Type 1 diabetes mellitus is characterized by destruction of the pancreatic beta cells.
- A common underlying factor in the development of type 1 diabetes is a genetic susceptibility.
- Destruction of beta cells leads to a decrease in insulin production, unchecked glucose production by the liver and fasting hyperglycemia.
- Glucose taken from food cannot be stored in the liver anymore but remains in the blood stream.
- The kidneys will not reabsorb the glucose once it has exceeded the renal threshold, so it will appear in the urine and be called glycosuria.
- Excessive loss of fluids is accompanied by excessive excretion of glucose in the urine leading to osmotic diuresis.
- There is fat breakdown which results in ketone production, the by-product of fat breakdown.
Type 2 Diabetes Mellitus
Pathophysiology of Diabetes Mellitus Type 2
|
Figure: Pathophysiology of Diabetes Mellitus Type 2
Type 2 diabetes mellitus has major problems of insulin resistance and impaired insulin secretion.
- Insulin could not bind with the special receptors so insulin becomes less effective at stimulating glucose uptake and at regulating the glucose release.
- There must be increased amounts of insulin to maintain glucose level at a normal or slightly elevated level.
- However, there is enough insulin to prevent the breakdown of fats and production of ketones.
- Uncontrolled type 2 diabetes could lead to hyperglycemic, hyperosmolar nonketotic syndrome.
- The usual symptoms that the patient may feel are polyuria, polydipsia, polyphagia, fatigue, irritability, poorly healing skin wounds, vaginal infections, or blurred vision
Gestational Diabetes Mellitus
- With gestational diabetes mellitus (GDM), the pregnant woman experiences any degree of glucose intolerance with the onset of pregnancy.
- The secretion of placental hormones causes insulin resistance, leading to hyperglycemia.
- After delivery, blood glucose levels in women with GDM usually return to normal or later on develop type 2 diabetes
Complication of DM
| Acute complications | a) Hypoglycemic coma. b) Diabetic ketoacidosis c) Non ketotic hyperosmolar diabetic coma d) Lactic acidosis e) Acute circulatory failure. |
| Chronic complications | Microvascular/ Neuropathic: a) Retinopathy, cataract
b) Nephropathy:
c) Peripheral neuropathy:
d) Autonomic neuropathy:
GIT problems
Macrovascular: a) Coronary circulation:
b) Cerebral circulation:
c) Peripheral circulation:
|
Management of DM:
Principle management of diabetes is “3D”
1. Discipline
2. Diet
3. Drugs
A. Discipline:
a) Patient motivation and education are central, idea about how to avoid complication (eg. Hypoglycemia, long term complication of hyperglycemia)
b) Lifestyle changes: Diet, exercise, ( insulin resistance)
c) Regular follow up
d) Tight BP control
B. Diet:
a) Restricted diet: Sweet, sugar, saturated fat
b) Measured diet: Carbohydrate 60%, Protein 20%, fat 20%
- Daily energy intake (calories):
- An obese middle aged or elderly person – 1000to 1600 kcal daily
- A young active person-1800 to 3000 Kcal daily (if overweight <1800 Kcal daily)
Carbohydrate:
- Daily intake from 100g to maximum 300g
- If 300g, 3 main meals = 180 mg, 3 snacks 90 g and 0.5 liters of milk = 30gm
- Consumption of both soluble fibre supplements and fibre rich foods (eg. barley, beans, peas)
- Protein – Moderate protein
- Fat – Total intake of fat should be reduced
- Alcohol-low intake but abstinence if obesity or hypertension
- Salt – Reduced intake (<6g daily)
- Diabetic foods and sweeteners
c) Unmeasured diet: Green vegetables, tomato or lemon, cucumber
d) Types of diabetic diets:
- Low energy, weight reducing diet: A diet of 1000 Kcal/day (1500Kcal in active person)
- Weight maintenance diet
- Nibbling
- Say weight 60 kg, so energy 1200 Kcal, Now it is given on the course of the day
Example
1. 3 main meals
- Morning: 2 slice bread + 1 egg + vegetables + dal
- Midday: 1.5 plate rice + vegetables + fish + meat + dal
- Night: 3 slice bread + vegetable + dal
2. In each of snacks (eg. at 11 am, 5 pm and 11 pm): 2 piece protein biscuit or 1 small banana + 1 biscuit
3. Milk without cheese, 0.5 litters in the course of the day
C. Drugs:
a) Oral hypoglycemic drugs:
- Sulphonylureas eg. chlorpropamide (indication: non obese patients with NIDDM who fails to respond dietary measure alone)
- Biguanides eg. metformin (indication: obese patients with NIDDM or in combination with sulfonylures)
b) Insulin:
- Unmodified (eg. actrapid): Short acting
- Modified (eg. monotard, isophane): Intermediate and long acting
(Ref-Davidson-820-22/22nd)
Diabetic Ketoacidosis
Definition of Diabetic ketoacidosis
Diabetic ketoacidosis is a medical emergency in which hyperglycaemia is associated with metabolic acidosis and hyperketonaemia principally in people with type 1 diabetes
Cardinal Feature of Diabetic Ketoacidosis
- Hyperglycaemia.
- Metabolic acidosis.
- Hyperketonaemia.
Pathogenesis of ketoacidosis
Diabetic pt.
↓
Lack of insulin.
↓
Increased catabolism
↓
Increased glycogenolysis.
Increased gluconeogenesis.
Increased lypolysis.
↓
Hyperketonaemia.
↓
Metabolic Acidosis.
↓
Diabetic ketacidosis
(Ref-Davidson-812/22nd)
Complication of DKA
- Cerebral edema – due to
✔ Rapid reduction of blood glucose &
✔ Use of hypotonic fluids &/or bicarbonate.
- ARDS
- Thromboembolism
- DIC
- Acute circulatory collapse
(Ref-Davidson-812/224)
Management of Diabetic ketoacidosis
Clinical features/Sign and Symptoms
Symptoms
- Polyuria, thirst
- Leg cramps.
- Weight loss
- Blurred vision
- Weakness
- Abdominal pain.
- Nausea, vomiting.
Sign’s
- Dehydration
- Smell of acetone.
- Hypotension
- Hypothermia. (Postural or Supine).
- Confusion, drowsiness, coma (10%)
- Cold extremities/ peripheral cyanosis.
- Tachycardia.
- Air hunger (Kussmaul breathing)
Diagnosis
History
1. H/O diabetes.
2. History of precipitating factor:
- Inter-current infection
- Loss of appetite.
- Either stop or reduce the dose of anti-diabetic drugs.
- Any form of stress.
Investigations
1. Urinalysis
- Ketonuria (Rothares test)
- Glycosuria. (Benedict’s test)
2. Blood glucose level:
- Very high.
3. Blood urea & serum creatinine.
4. Serum electrolytes & bicarbonate
5. Blood gases to assess the severity of acidosis..
a) Blood & urine C/S.
b) CBC-leukocytosis &CRP
c) X ray chest.
d) ECG
Treatment
Principle components of Rx
- Administration of short acting (soluble) insulin.
- Fluid replacement
- Potassium replacement
- Administration of antibiotics if infections is present.

Fluid replacement
0.9% saline (NaCI) I.V.
- 1 liter over 30 minutes
- 1 liter over 1 hr
- 1 liter over 2 hrs
- 1 liter over next 2-4 hrs
When blood glucose < 15 mmol/I (270 mg/dl)
- Switch to 5% dextrose, I liter 8-hourly
- If still dehydrated, continue 0.9% saline and add
- 5% dextrosel liter per 12 hr
- Typical requirement is 6 liters in first 24 hrs but avoid fluid overload in elderly patients
- Subsequent fluid requirement should be based on clinical response including urine output.
Insulin
50 units soluble insulin in 50 ml 0.9% saline i.v. via infusion pump
- 6 units/hr initially
- 3 units/hr when blood glucose < 15 mmol/l (270 mg/dl)
- 2 units/hr if blood glucose declines <10 mmol/l (180 mg/dl)
- Check blood glucose hourly initially if no reduction in first hour, rate of insulin infusion should be increased
- Aim for fall in blood glucose of 3-6 mmol/l (55-110 mg/dl) per hour.
Alternatively: If IV infusion is not possible:
- 10-20 units soluble insulin IM stat then 4-6 units hourly.
- If no response within 2 hrs. the dose of insulin should be doubled.
- If blood glucose 10-15 mmol/L, insulin 1-4 units hourly.
Potassium:
- None in first litre of i.v fluid unless < 3.0 mmol/l
- If plasma potassium <3.5 mmol/l, give 20 mmol/hr added potassium
- If plasma potassium is 3.5-5.0 mmol/l, give 10 mmol/hr
Antibiotic: Broad spectrum antibiotic if infection is present

Additional measures in Mx of DKA
- Catheterization if no urine passed after 3 hrs
- Nasogastric tube to keep stomach empty in unconscious or semiconscious patients, or if vomiting is protracted
- Central venous line if cardiovascular system compromised, to allow fluid replacement to be adjusted accurately
- Plasma expander if systolic BP is <90 mmHg or does not rise with i.v. saline.
- Antibiotic: Broad spectrum antibiotic if infection is present
- ECG monitoring in severe cases
Monitoring
- Blood glucose & electrolyte hourly for 3 hrs & every 2-4 hrs thereafter.
- Temp., pulse, respiration, BP hourly.
- Urine output & ketones.
- ECG, plasma osmolality
- Arterial PH in some cases.
(Ref-Davidson-809-11/21)

