Chromosomal abnormalities – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric- nursing.
Pediatric-nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric-nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Chromosomal abnormalities

Chromosomal abnormalities occur either in the form of numerical or structural alterations and found time to time in human beings. They arise in various ways, i. e. non-disjunction, translocation, deletion, duplication, inversion, iso-chromosomes and mosaicism. The most common chromosomal abnormality related to autosomes is Down’s syndrome or Trisomy 21.
Some Chromosomal Abnormalities in Children:
- Down’s syndrome.
- Turner’s syndrome.
- Klinefelter’s syndrome.
Spina Bifida
Definition of Spina Bifida:
It is the congenital defect of the spinal column due to failure of the fusion of vertebral arches with or without protrusion of the meninges and dysplasia of the spinal cord.
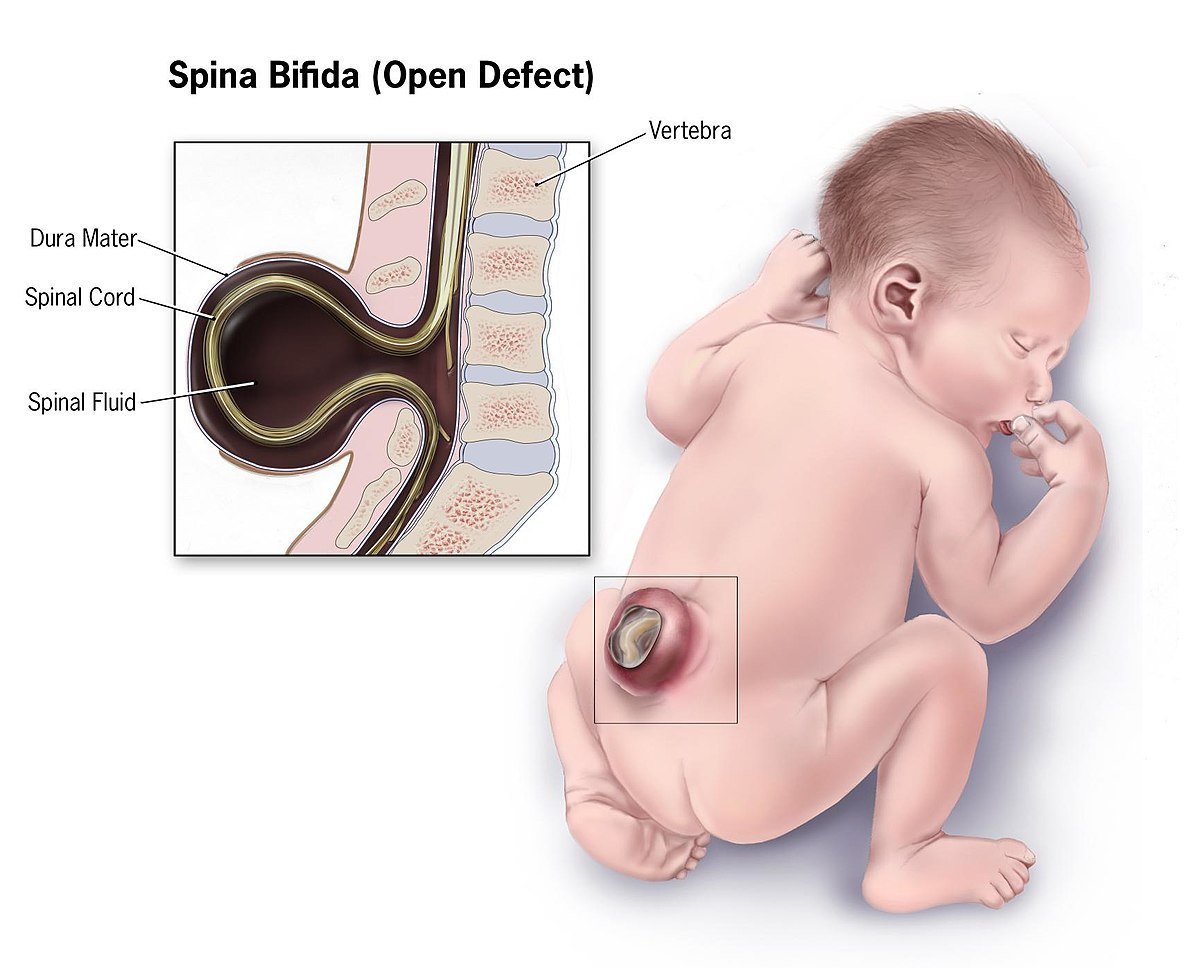
Spina bifida is a major birth defect and a type of neural tube defect that involves an opening in the vertebral column caused by the failure of the neural tube to close properly during embryonic development.
Or
Spina bifida is a birth defect that occurs when the spine and spinal cord don’t form properly. It falls under the broader category of neural tube defects. The neural tube is the embryonic structure that eventually develops into the baby’s brain and spinal cord and the tissues that enclose them.
(Ref: Paediatric Nursing, Parul Datta/3rd/380)
Types of Spina Bifida:
Spina bifida can occur in different forms:
1. Spina bifida occulta,
2. Meningocele
3. Myelomeningocele.
A. Spina bifida occulta: “Occulta” means hidden. The mildest form, spina bifida occulta results in a small separation or gap in one or more of the bones of the spine (vertebrae). Many people who have spina bifida occulta don’t even know it, unless the condition is discovered during an imaging test done for unrelated reasons.
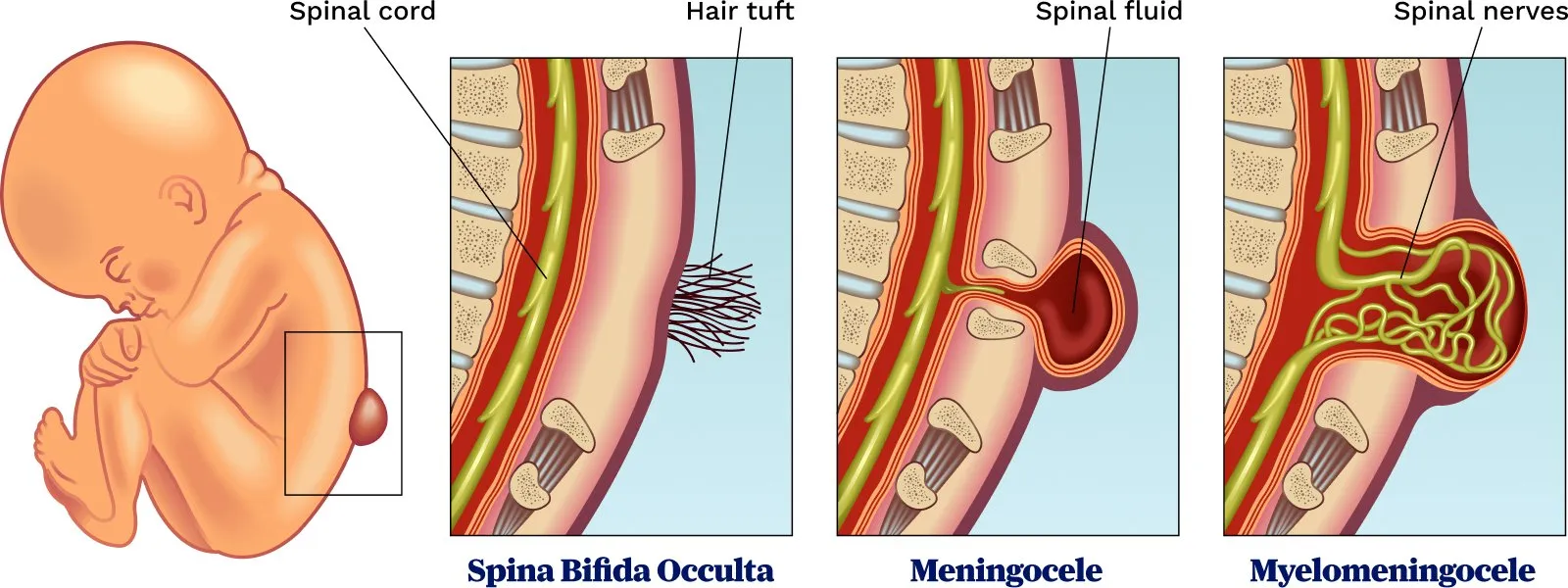
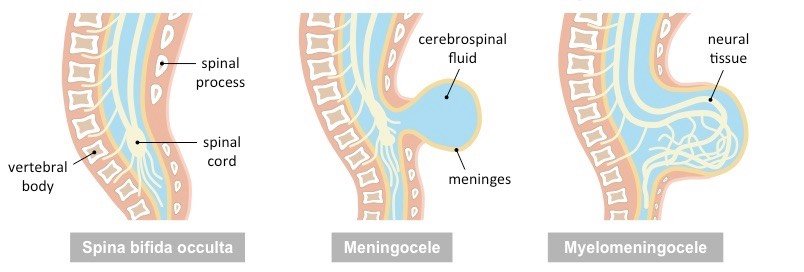
B. Meningocele: In a form of spina bifida called meningocele, the protective membranes around the spinal cord (meninges) push out through the opening in the vertebrae, forming a sac filled with fluid. But this sac doesn’t include the spinal cord, so nerve damage is less likely, though later complications are possible.
C. Myelomeningocele: Also known as open spina bifida, myelomeningocele is the most severe form. The spinal canal is open along several vertebrae in the lower or middle back. The membranes and spinal nerves push through this opening at birth, forming a sac on the baby’s back, typically exposing tissues and nerves. This makes the baby prone to life-threatening infections.
Another Answer:
1. Spina bifida occulta:
The defect is only in the vertebrae. The spinal cord and meninges are normal.
2. Meningocele:
The meninges protrude through the opening in the spinal canal. This forms a cyst filled with CSF and covered with skin.

3. Myelomeningocele (or meningomyelocele):
The spinal cord and cord membranes protrude through the defect in the laminae of the vertebral column. Myelomeningoceles are covered by a thin membrane.
4. Myeloschisis:
Spina bifida with myeloschisis is the most severe form of myelomeningocele. In this type, the involved area is represented by a flattened, plate-like mass of nervous tissue with no overlying membrane. The exposure of these nerves and tissues make the baby more prone to life-threatening infections such as meningitis.
Causes/Risk Factors of Spina Bifida:
The actual cause is still unknown. However, the likely causes are:
1. Poor economic status
2. Alcohol use
3. Vitamin A deficiency
4. Folic acid deficiency
5. Family history
6. Maternal use of valproic acid.
7. Genetic conditions
8. Other risk factors for spina bifida include: obesity, diabetes
Clinical Features of Spina Bifida:
Most of the cases are asymptomatic. Some children present with –
- Cutaneous lesions over the defect
- Tuft of hairs, nevus, lipoma, hemangioma, dermal sinus or as dimple in the skin
- There may be intraspinal lesions like dermoid cyst, intramedullary lipoma, etc.
Symptomatic children present with –
- Progressive deformity of the foot
- Changes in micturition pattern
- Alteration in the gait
- Trophic ulcers on the toes and feet.
- Other significant anomalies of the spinal cord (syringomyelia, diastematomyelia, tethered cord, etc.)
(Ref: Paediatric Nursing, Parul Datta/34/380)
Risk Factors of Spina Bifida:
Spina bifida is more common among whites and Hispanics, and females are affected more often than males. Although doctors and researchers don’t know for sure why spina bifida occurs, they have identified some risk factors:
1. Folate deficiency. Folate (vitamin B-9) is important to the healthy development of a baby. Folate is the natural form of vitamin B-9. The synthetic form, found in supplements and fortified foods, is called folic acid. A folate deficiency increases the risk of spina bifida and other neural tube defects.
2. Family history of neural tube defects. Couples who’ve had one child with a neural tube defect have a slightly higher chance of having another baby with the same defect. That risk increases if two previous children have been affected by the condition. In addition, a woman who was born with a neural tube defect has a greater chance of giving birth to a child with spina bifida. However, most babies with spina bifida are born to parents with no known family history of the condition.
3. Some medications. For example, anti-seizure medications, such as valproic acid (Depakene), seem to cause neural tube defects when taken during pregnancy, possibly because they interfere with the body’s ability to use folate and folic acid.
4. Diabetes. Women with diabetes who don’t control their blood sugar well have a higher
risk of having a baby with spina bifida.
5. Obesity. Pre-pregnancy obesity is associated with an increased risk of neural tube birth defects, including spina bifida.
6. Increased body temperature. Some evidence suggests that increased body temperature (hyperthermia) in the early weeks of pregnancy may increase the risk of spina bifida. Elevating your core body temperature, due to fever or the use of saunas or hot tubs, has been associated with a possible slight increased risk of spina bifida.
Treatment/Management of Spina Bifida:aanM
- Progressive neurological deficits require surgical correction of the defect.
- Laminectomy is done and the intraspinal lesion is excised.
- Operation can be done even before neurological deficit appears in selected cases.
- Myelo-CT scan and MRI help to confirm the diagnosis before operation.
(Ref: Paediatric Nursing, Pariil Datta/34/380)
Nursing Interventions of Spina Bifida:
A. Nursing Assessment
- Assess sensory and motor response of lower extremities.
- Assess ability to void spontaneously, retention of urine, symptoms of UTI.
- Assess usual stooling patterns, need for medications to facilitate elimination.
- Assess mobility and use of braces, casts, and other special equipment.
B. Nursing Diagnosis
- Neonates (Preoperative)
- Risk for impaired skin integrity related to impaired motor and sensory function.
- Risk for infection related to contamination of the myelomeningocele site.
- Impaired urinary elimination related to neurologic deficits.
- Ineffective tissue perfusion: cerebral related to potential hydrocephalus.
- Fear (parents) related to neonate with neurologic disorder and to surgery.
Infants and Children
- Ineffective thermoregulation following surgery
- Impaired urinary elimination related to sacral denervation
- Bowel incontinence or constipation related to impaired innervation of anal sphincter and bowel musculature.
- Disturbed body image related to the child’s appearance, difficulties with locomotion, and lack of control over excretory functions.
C. Nursing Interventions
- Protect against infection (breakdown of sac exposes spinal cord to environment)
✓ Provide meticulous skin care; keep area clean of urine and feces.
✓ Apply sterile, moist, nonadherent dressing over sac to prevent drying; use sterile normal saline for moistening; change dressing every 2 to 4 hours to maintain moistness.
✓Inspect sac for leaks, abrasions, irritation, or signs of infection.
✓ Avoid pressure on sac; do not cover with diaper.
- Measure head circumference daily; measure at greatest circumference (usually slightly above eyebrows and pinna of ears and around occipital prominence at back of skull); place marks on both sides of head to facilitate accurate serial measurements.
- Maintain in prone position to prevent injury to sac.
- Perform passive range of motion exercises to extremities unless contraindicated.
- Promote elimination
✓ Observe for urinary retention or continuous leakage of urine; perform intermittent straight catheterization as ordered.
✓Observe for bowel sphincter weakness (e.g., Continual passage of stool that is not diarrhea)
- Provide postoperative care
✓Maintain side-lying or prone position to prevent tension on suture line and skin graft.
✓ Measure head circumference daily because increase may indicate developing hydrocephalus.
✓ Monitor for signs of increased intracranial pressure.
✓ Use pain rating scale and medicate appropriately.
D. Family Education and Health Maintenance
- Prepare the parents to feed, hold, and stimulate their infant as naturally as possible.
- Teach the parents the special techniques that may be required for holding and positioning, feeding, caring for incision, emptying the bladder, and exercising muscles.
- Alert the parents to safety needs of the child with decreased sensation, such as protection from prolonged pressure, the risk of burns due to bath water that is too warm, and avoidance of trauma from contact with sharp objects.
- Urge continued follow-up and health maintenance, including immunizations and evaluation of growth and development.
- Advise parents that children with paralysis are at risk for becoming overweight due to inactivity, so they should provide a low fat, balanced diet, control snacking, and encourage as much activity as possible.
E. Evaluation/Outcomes
- Remains free of infection
- Maintains skin integrity
- Family demonstrates ability to care for infant
- Family continues follow-up care and habilitation.
[A Short Textbook of Traumatology and Orthopedic Nursing/Kibria/3rd/271-3]
