Cushing syndrome – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Cushing syndrome
Definition of Cushing syndrome
It is a clinical condition in which free circulating glucocorticoids level is increased. Most common cause is iatrogenic due to prolonged administration of synthetic glucocorticoid such as prednisolone.
Classification/Cause of Cushing syndrome
A. ACTH dependent
- Pituitary adenoma secreting ACTH (e.g. Cushing’s disease)
- Ectopic ACTH syndrome
- (e.g. bronchial carcinoid, small cell lung carcinoma, pancreatic -endocrine carcinoma)
- Iatrogenic (ACTH therapy).
B. Non-ACTH dependent
- Latrogenic (chronic glucocorticoid therapy, e.g. For asthma)
- Adrenal adenoma
- Adrenal carcinoma.
C. Pseudo-Cushing’s syndrome: (i.e. cortisol excess as a part of another illness)
- Alcohol excess
- Major depressive illness
- Primary obesity.
(Ref by-Davidson-770/21″)
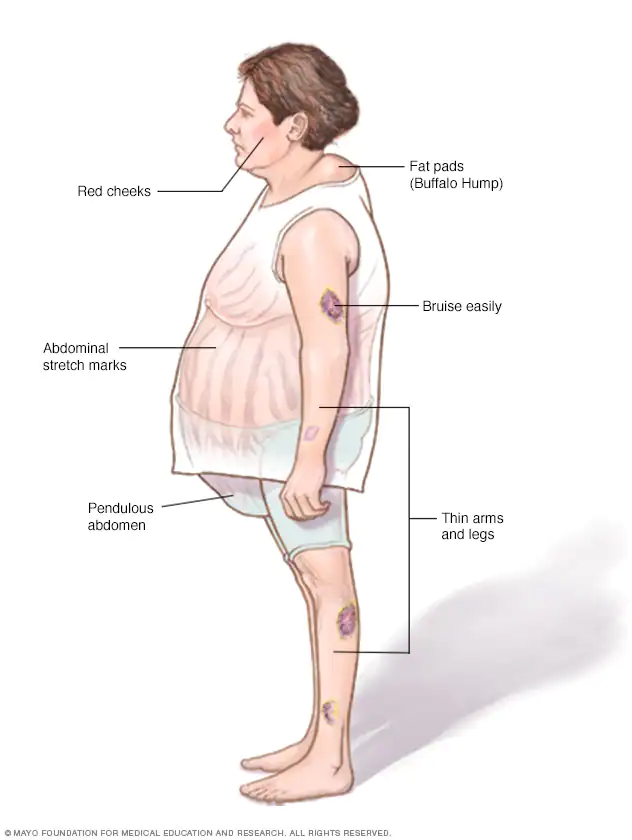
Clinical Features of Cushing Syndrome
A. General appearance
- Moon face (due to deposition of fat in the face).
- Buffalo neck (due to deposition of fat in the subscapular region)
- Hair thinning.
- Hirsutism.
- Acne
- Mild exophthalmos.
- Cataract.
- Plethora.
B. Skin
- Bruising.
- Striae
- Decreased skin thickness.
C. Musculoskeletal system
- Wasting & weakness of proximal thigh muscle.
- Loss of height and back pain from compression fracture
- May have exuberant callus with fractures
- Osteoporosis
D. Abdominal
- Centripetal obesity or pendulous abdomen (due to deposition of fat in the abdomen & buttock
- Peptic ulcer
E. Tendency to infections with poor wound healing and little inflammatory respone
F. Hypertension
G. Genitourinary
- In male- impotence (due to atrophy of testes)
- In female- amenorrhoea (due to atrophy of ovary)
H. Hyperglycaemia
I. Psychosis.
Investigation of Cushing syndrome
To confirm the Dx
- 24 Urinary free cortisol level – raised.
- Overnight dexamethasone suppression test: Fail to suppress.
- Diurnal rhythm of plasma cortisol: evening level >75% of morning level in Cushing’s
To detect the cause
- Plasma ACTH level.
- Excess cortisol + undetectable ACTH-Adrenal tumor.
- Detectable ACTH-Pituitary adenoma secreting ACTH (e.g. Cushing’s disease) or
- Ectopic ACTH syndrome.
- Plasma CRH test & High dose dexamethasone suppression test
- Adrenal USG, CT scan or MRI.
- MRI for Cushing’s disease.
- Inferior petrosal sinus sampling for Cushing’s disease (>200% of ACTH conc.)
Treatment
1. Medical therapy: Metyrapone, Ketoconazole-inhibit cortisol synthesis.
2. Cushing’s disease:
- Trans-sphenoidal surgical removal of pituitary adenoma pell
- If no tumor is found & Dx is Cushing’s disease – radical hypophysectomy may be required.
- Bilateral adrenalectomy with pituitary irradiation to prevent Nelson’s syndrome.
3. Adrenal tumors:
- Adenoma: Removed via laparoscopy or loin incision.
- Carcinoma: Resected if possible or Irradiation & adrenolytic drug is given to the pt.
4. Ectopic ACTH syndrome:
- Bronchial carcinoid is removed.
- Malignancies – Radiotherapy, chemotherapy according to choice.
5. Iatrogenic cushing’s syndrome:
- Gradually tapering the receiving steroid & ultimately stop if possible

differentiate Cushing’s syndrome from myxedema clinically
| Points | Myxodema | Cushing’s syndrome |
| Voice | Hoarseness of voice | Normal voice |
| Reaction to hot | Cold intolerance | Not such |
| Thyroid swelling | Goitre usually present | Not present |
| Appearance | Puffy face with baggy eyelid | Moon face with Buffalo neck |
| Weight gain | Periorbital oedema present & genelralized | Central obesity is more common |
| Easy bruising & striae | Not present | Present |
| Skin condition | Increased thickness & dry with rough | Decreased skin thickness. |
