Spina Bifida – An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Spina Bifida
Definition of spina bifida:
Spina bifida is a congenital disorder in which the two halves of the posterior vertebral arch fail to fuse at one or more levels.
This neural tube defect or spinal dysraphism, which occurs within the first month of foetal life usually, affects the lumbar or lumbosacral segments of the spine. In its most severe form, the condition is associated with major neurological problems in the lower limbs together with incontinence.
[Ref- Apley’s, “System of orthopedics and fractures”, 9 edition, P-24″]
Or
Spina bifida is one of the commonest anomaly of neural tube development seen in infants.
(Ref- Parul Datta’s, “Pediatric Nursing”, 2 edition, P-405)
Or
Spina bifida is the common congenital disorder of the spine; involve the defect in the spinal column characterized by failure of fusion between one or more vertebral arches.
Or
Spina bifida, also called spinal dysraphia, is a malformation of the spine in which the posterior portion of the laminae of the vertibra fails to close.
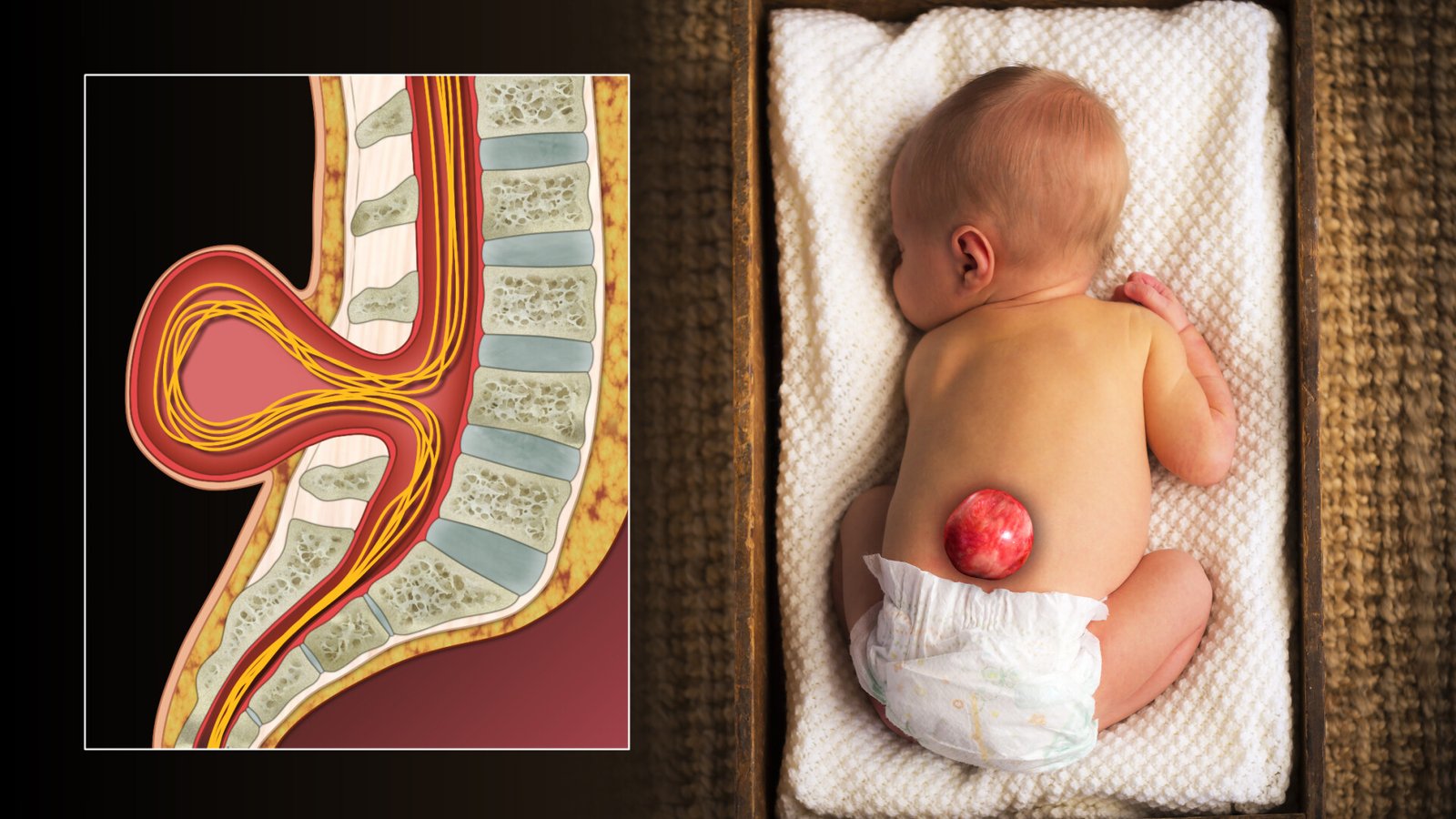
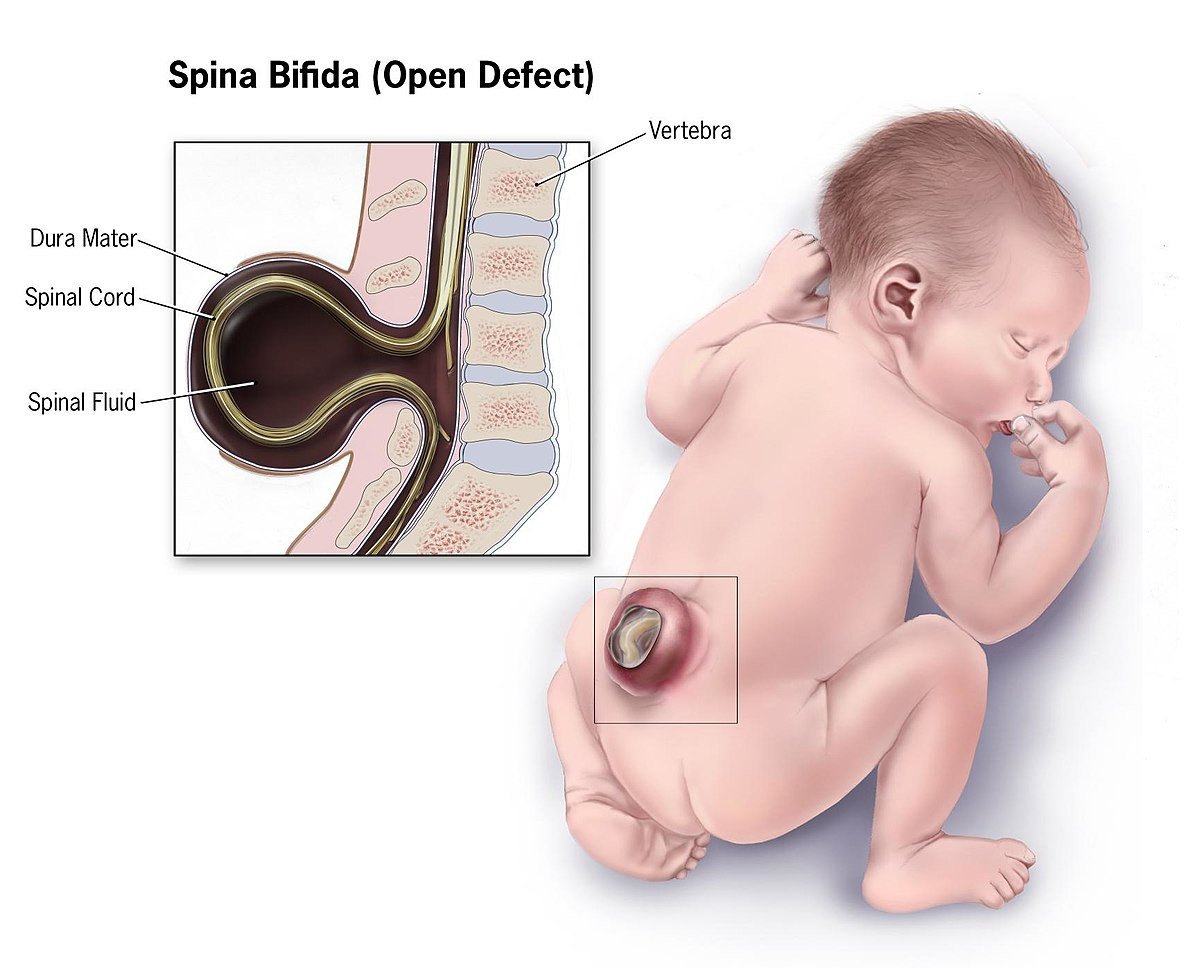
Classification of spina bifida:
1. Spina bifida occulta. The defect is only in the vertebrae. The spinal cord and meninges are normal.
2. Meningocele: The meninges protrude through the opening in the spinal canal. This forms a cyst fluid with Csf and covered with skin.
3. Meningomyelocele or myelomeningocele :
The spinal cord and cord membranes protrude through the defect in the laminal of the vertebral column. Myelomeningoceles are covered by a then membrane.
[Ref- Parul Datta’s, “Pediatric Nursing”, 2 edition, P-405]
Causes of spina bifida:
Multifactoral cause. These are:
1. Folic acid deficiency.
2. Chromosome.
3. Maternal risk factors- Certain drugs, including valporic acid, anticonvulsant drud etc.
4. Alcohol.
Clinical features of spina bifida:
A) Asymptomatic feature: Most of the cause are asymptomatic. Some children present with after birth-
1. Hydrocephalus
2. Apnea
3. Stridor
4. Club foot
5. Tuft of hair on the back
6. Swelling in the spine, may be –
- Lipoma.
- Hamangioma.
7. Impaired neurological function.
B) Symptomatic feature:Its usually present 6-8 years age with any of the following;
1. Progressive deformity of the foot.
2. Changes in the micturation pattern
3. Alteration in the gait
4. Topic ulcer on the toes and feet.
5. Absence of sensation and drop reflex.
6. Flaccid paralysis.
7. Paralysis of the lower limb.
8. Loss of bowel function, e.g: constipation
9. Growth retardation.
C) Diagnostic evaluation:
1. Ultrasound-Neural tube and kidney
2. X-ray head, lumber spine
3. CT scan
4. MRI-brain and spinal cord.
Treatment of spina bifida:
1. In case of spina bifida occulta conservative management to establish the patter of development as near normal as possible.
2. In case of meningocele and myelomeningocele, surgical removal of the sac is closure of the defect.
3. Physical and occupational therapy.
Complications of spina bifida:
1. Progressive deformity of the foot.
2. Changes in micturation pattern.
3. Alteration in the gait.
4. Trophic ulcers on the toes and feet.
5. Tethered cord.
6. Skin rupture.
7. Faecal
8. Hip dislocation
9. Kyphosis and Scolosis
10. infection of CNS.
11. Syringomyelia.
12. Diastematomyelia.
13. Tethered cord.
[Ref- Parul Datta’s, “Pediatric Nursing”, 2nd edition, page 405]
Nursing interventions and prevention of spina bifida:
1. Protecting skin integrity:
a.Position: Prone position with hips only slightly flexed to decrease pressure on the sac.
b. Avoid positioning on back.
c. Observe the sac for irritation or leakage of CSF every shift.
2. Preventing infection by:
a. Infants buttocks and genitalia must be kept clean.
b. Apply sterile gauze, moistened dressing over the sac.
e. Monitor and report immediately if:
- Oosing of fluid from the sac.
- Fever
3. Reducing fever by:
a. Encourage the patient to express feelings.
b. Include the parents with care plan.
4. Promoting urinary elimination by: 4
a. Regular monitoring the urine output.
5. Emotional and psychological support.
6. Preventing hip deformity.

Prevention of spina bifida:
1. General:
a. Genetic counseling is the true preventive measure of spina bifida.
b. Reducing and discouraging consanguineous marriages.
c. Avoiding late marriage of female and avoidance of pregnancy beyond the age of 35 years.
d. Promotion of health of girl child and pre-pregnant health status of the females by prevention of malnutrition, anaemia, folic acid deficiency iodine deficiency etc.
e. Encourage the immunization of all girl children by MMR (Measles. Mumps and Rubella). f. Elimination of active and passive smoking of tobacco by mothers.
g. Avoidance of drug intake without counseling by physician in the first trimester of pregnancy.
h. Avoidance of cytotoxic drugs.
i. Discouraging reproduction after birth of a baby with congenital anomalies without genetic counseling.
j. Encourage folic acid 400mg/day.
2. Specific:
a) The use of folic acid before conception and during pregnancy is associated to lower incidence of
spina bifida. b) AFP test (Alpha Feto Protein) from amniotic fluid.
c) Antenatal Screening during 15-18 th weeks of pregnancy.
d) Ultrasound Scanning.
e) Arrangement of termination of pregnancy when it is detected.
[Ref- Parul Datta’s, “Pediatric Nursing”, 2nd edition, page-199, 200]
