Umbilical cord – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Umbilical cord
The umbilical cord is a tube-like structure that connects a fetus to the mother’s placenta, providing oxygen and nutrient-rich blood and removing waste.
or
A cord arising from the navel that connects the fetus with the placenta and through which respiratory gases, nutrients, and wastes pass.

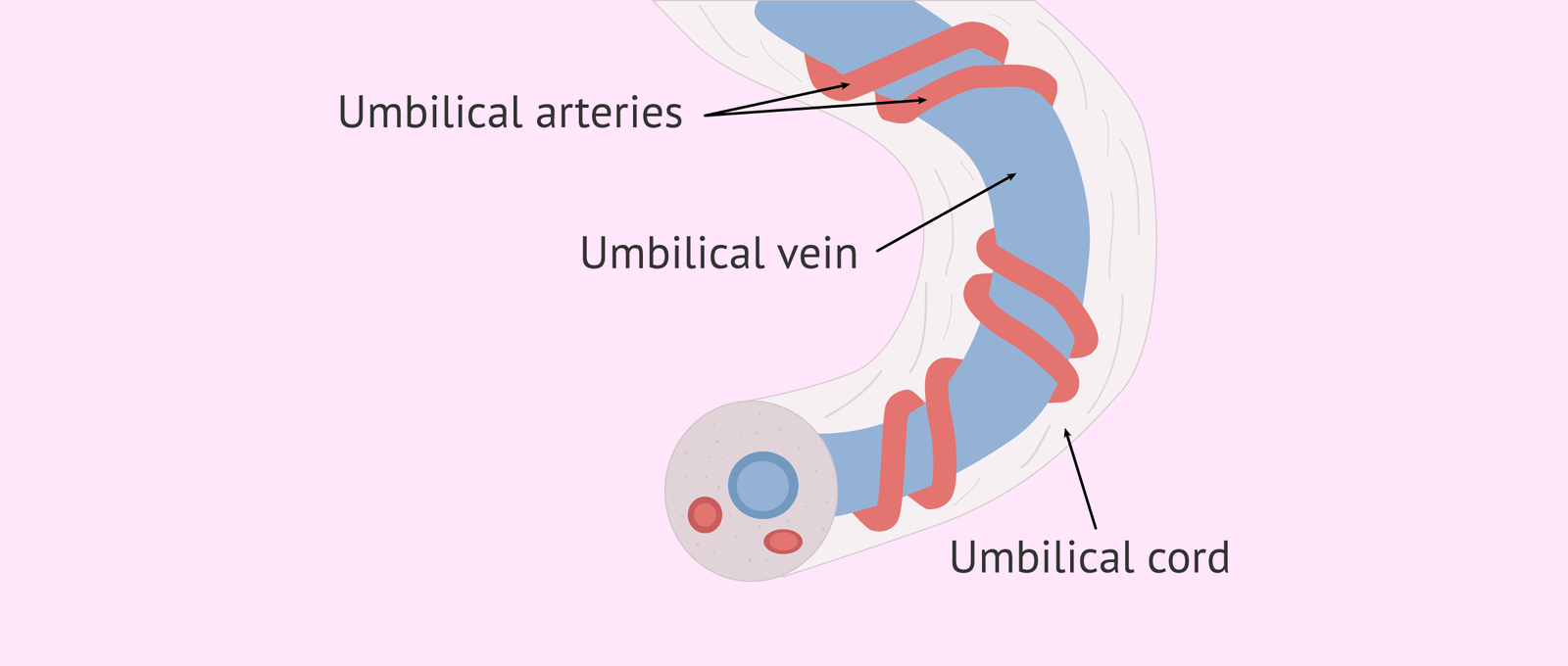
Figure: umbilical cord
Structure/content of umbilical cord:
A. Covering epithelium: It is lined by a single layer of epithelium.
B. Wharton’s jelly: It consists of elongated cells in a gelatinous fluid and rich in mucopolysaccharides and has got protective function to the umbilical vessels.
C. Blood vessels: Initially there are four vessels (2 arteries and 2 veins). But after 4 months the right umbilical vein disappears and two umbilical arteries and one umbilical vein remains.
D. Remnant of the umbilical vesicle (yolk sac) and its vitelline duct.
E. Allantosis.
F. Obliterated extraembryonic coelom.
Criteria/characteristics of umbilical cord:
1. Length: 30-100 cm (average 40 cm).
2. Diameter: 1-2.5 cm (average 1.5 cm)
3. False knots may be present due to dilatation of the umbilical veins or local collection of Wharton’s jelly.
4. It shows a spiral twist from left to right as early as 12tb week.
5. The umbilical arteries do not possess an intimal elastic lamina but have got well developed muscular coat.
6. Both the arteries & the vein does not possess vasavasorum
Development:
Form the connective stalk or body stalk which is a band of mesoblastic tissue stretching between the embryonic disc & the chorion.
[D.C. Dutta’s Obs/9th/35-36]
Cord abnormalities:
1. According to length:
➤ Long cord (>100 cm)
➤ Short cord (<20 cm)
2. According to presence of knot:
➤ True knot
➤ False Knot
3. According to attachment with placenta:
➤ Velamentous placenta
➤ Battledore placenta
4. Abnormalities in umbilical vessels:
➤ Single umbilical artery
Dangers/disadvantages of an abnormally long cord:
➤ Cord prolapse
➤ Cord entanglement round the neck or the body which may cause fetal distress or fetal death.
Umbilical cord prolapse:
Umbilical cord prolapse:
Umbilical cord prolapse occurs when the cord slips into the vagina after the membranes (bag of waters) have ruptured, before the baby descends into the birth canal. This complication affects about 1 in 300 births. Pressure on the cord reduces or cuts off blood flow from the placenta to the baby, decreasing the baby’s oxygen supply. Umbilical cord prolapse can result in stillbirth unless the baby is delivered promptly, usually by cesarean section.
The risk of umbilical cord prolapse
The risk of umbilical cord prolapse increases if:
1. The baby is in a breech (foot-first) position.
2. The woman is in preterm labor.
3. The umbilical cord is too long.
4. There is too much amniotic fluid.
5. The provider ruptures the membranes to start or speed up labor.
6. The woman is delivering twins vaginally. The second twin is more commonly affected.
Other risk factors for umbilical cord prolapse include:
➤ Low birth weight
➤ Prematurity
➤ Transverse lie (baby’s spine perpendicular to mother’s) with back-up presentation, or breech presentation
➤ Premature labor with premature rupture of the membranes
➤ Abnormally long umbilical cord
➤ Polyhydramnios (an excessive amount of fluid in the amniotic sac)
➤ Artificial rupture of the membranes by a healthcare provider can lead to iatrogenic W (caused by the doctor) cord prolapse if the water bag is intentionally broken during early labor and the baby’s head is not engaged.