Concept about Placenta – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Concept about Placenta
Definition of placenta:
The placenta (also known as afterbirth) is an organ that connects the developing fetus to the uterine wall to allow nutrient uptake, provide thermo-regulation to the fetus, waste elimination, and gas exchange via the mother’s blood supply, fight against internal infection and produce hormones to support pregnancy.
or
A temporary organ that joins the mother and fetus, transferring oxygen and nutrients from the mother to the fetus and permitting the release of carbon dioxide and waste products from the fetus.
or
The placenta is a flattened circular organ in the uterus of pregnant maminals that nourishes and maintains the fetus through the umbilical cord. This cord is the main link from the fetus to the placenta. Through it, the placenta provides oxygen and nutrients to the growing baby and removes waste products.
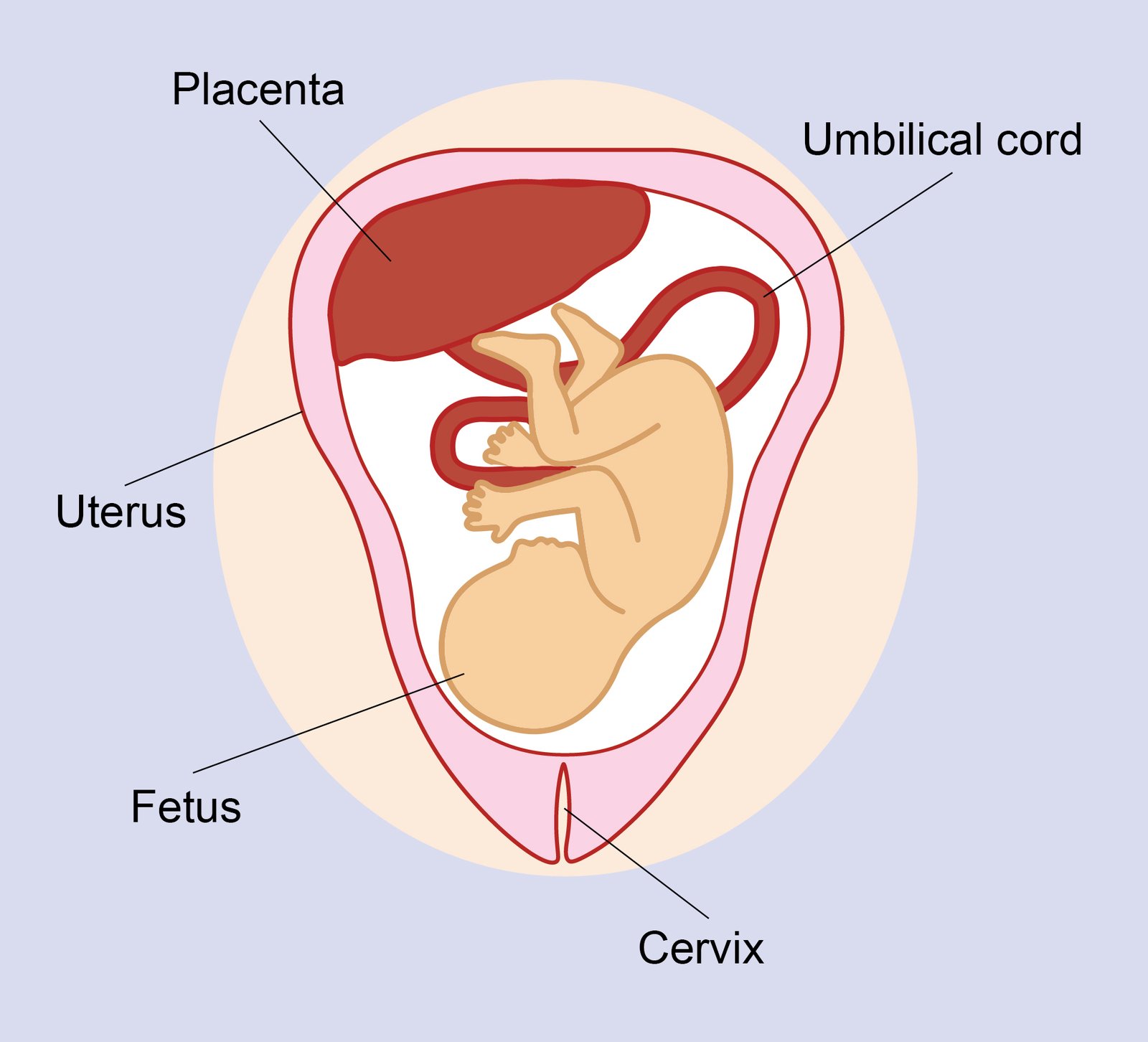
Figure: Placenta
Types of placenta:
1. Epithelio-chorial placenta (swine, horse).
2. Endothelio-chorial placenta (dog, cat).
3. Hemo-chorial placenta (human, rodents, primates).
Classification Based on Placental Shape and Contact Points:
| Type of Placenta | Common Examples |
| Diffuse, epitheliochorial | Horses and pigs |
| Cotyledonary, epitheliochorial | Ruminants (cattle, sheep, goats, deer) |
| Zonary, endotheliochorial | Carnivores (dog, cat, ferret) |
| Discoid, hemochorial | Humans, apes, monkeys and rodents |
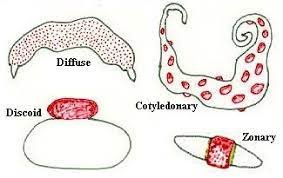
Figure: Types/classification of placenta
Structure of placenta:
1. In humans, the placenta averages 22 cm (9 inch) in length and 2-2.5 cm (0.8-1 inch) in thickness, with the center being the thickest, and the edges being the thinnest.
2. It typically weighs approximately 500 grams (just over 1 lb).
3. It has a dark reddish-blue or crimson color. It connects to the fetus by an umbilical cord of approximately 55-60 cm (22-24 inch) in length, which contains two umbilical arteries and one umbilical vein.
4. The umbilical cord inserts into the chorionic plate (has an eccentric attachment). Vessels branch out over the surface of the placenta and further divide to form a network covered by a thin layer of cells.
5. This results in the formation of villous tree structures. On the maternal side, these villous tree structures are grouped into lobules called cotyledons,
6. In humans, the placenta usually has a disc shape, but size varies vastly between different mammalian species.
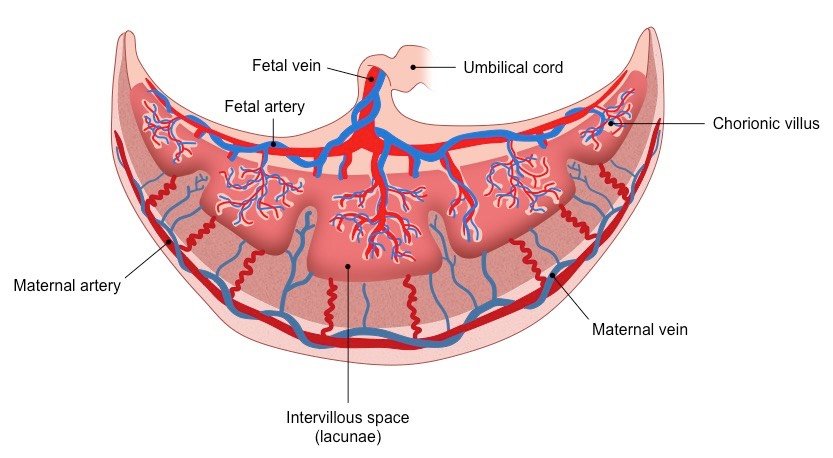
Figure: Structure of placenta
Placental barrier:
Separation of the maternal and fetal blood is referred to as the “placental barrier”
Formation of placental barrier:
The placental barrier is made up of a number of layers;
➤ Syncytiotrophoblast
➤ Discontinuous inner cytotrophoblast layer
➤ Basal lamina of the trophoblast
➤ Connective (mesenchymal) tissue of the villus
➤ Basal lamina of the endothelium
➤ Endothelium of the fetal placental capillary in the teriary villus
[D.C. Dutta’s Obs/9th & lecture]
Functions of placenta:
The placenta performs the following functions:
1. Nutrition: Food materials pass from the mother’s blood into the foetal blood through the placenta.
2. Digestion: The trophoblast of the placenta digest protein before passing them into foetal blood.
3. Respiration: Through the placenta oxygen passes from the maternal blood to the foetal blood, and carbon dioxide passes from foetal blood to maternal blood.
4. Excretion: Nitrogenous wastes such as urea pass from foetal blood into maternal blood through placenta and are filtered out by the kidneys of the mother.
5. Storage: The placenta stores glycogen, fat etc. for the foetus before liver is formed.
6. Barrier: Placenta functions as an efficient barrier (defensive wall) and allows useful: aerials to pass into the Social blood. Harmful substances such as nicotine from cigarette and addictive drugs such as heroin can pass through placenta. Therefore, pregnant women should avoid cigarette and drugs. Viruses and bacteria can pass through placenta.
7. Endocrine function: Placenta functions as an endocrine gland it secretes hormones such as oestrogen, progesterone and human chorionic gonadotropin (HCG).
8. Immunological function: Antibody from mother crosses the placenta and give passive immunity to the fetus.
9. Detoxification: Placenta detoxify some drugs.
Placental circulation:
Fetal blood: low in oxygen, this is pumped by the fetal heart towards the placenta along the two umbilical arteries and through their branches to the capillaries of the chorionic villi.
- Carbon dioxide is excreted, and oxygen taken up
- The blood then returns to the fetus along the one umbilical vein
Maternal blood: flows to the placenta to the decidua by spiral arterioles, and flows into the blood spaces surrounding the chorionic villi;
- It ‘bathes’ the villi as it circulates around the villi, so oxygen and nutrients can be absorbed, or wastes exchanged;
- The maternal blood then flows back into a branch of the maternal uterine vein.
Early placental development:
- The blastocyst reaches the uterus wall; the trophoblast layer has developed fine threadlike projections which later become the chorionic villi.
- These ‘sticky’ projections are what enable implantation into the endometrium; by day 10 post-fertilisation, the trophoblast is completely embedded in uterine lining:
- The blastocyst produces human chorionic gonadotrophin (HCG) to signal the corpus luteum to continue producing progesterone.
- More villi develop where there is most blood supply – that is, in the basal decidua of the endometrium (the decidua basalis); here the trophoblast is called the chorion frondosum which will later develop into the placenta.
- The villi under the capsular decidua (decidua capsularis) gradually degenerate and form the chorion laeve or ‘bald’ chorion, which eventually becomes the chorion membrane.
- Decidua parietalis is the remaining uterine lining.
- The villi erode the walls of maternal blood vessels in the decidua and this opens the blood vessels up to form a ‘lake’ of maternal blood, called a sinus, in which the villi float;
- These villi are known as the nutritive villi as they absorb nutrients and oxygen from the maternal blood and excrete waste
- A few villi are more deeply attached to the decidua and known as anchoring villi.
- Each of the villi is a branching structure with a centre of mesoderm with fetal blood vessels, and branches of the umbilical vein and artery. These are covered with a single layer of cytotrophoblast cells, and the external layer of the villi is the synctiotrophoblast;
- This means that there are 4 layers of tissue that separate the maternal blood from the fetal blood; it is impossible for the maternal and fetal circulation to mix unless any villi are damaged.
- Small spaces called lacunae appear in the synctiotrophoblast and become filled with blood from the sinusoids and secretions from the eroded endometrial glands.
- The lacunae fuse together to form the intervillous spaces of the placenta through which maternal blood flows.
The mature placenta is completely formed and functioning 10 weeks after fertilization.
- Between 12 and 20 weeks, the placenta weighs more than the fetus.
- As it matures the placenta becomes compact, and at term is a round flat organ that weighs about 1/6th the weight of the baby.
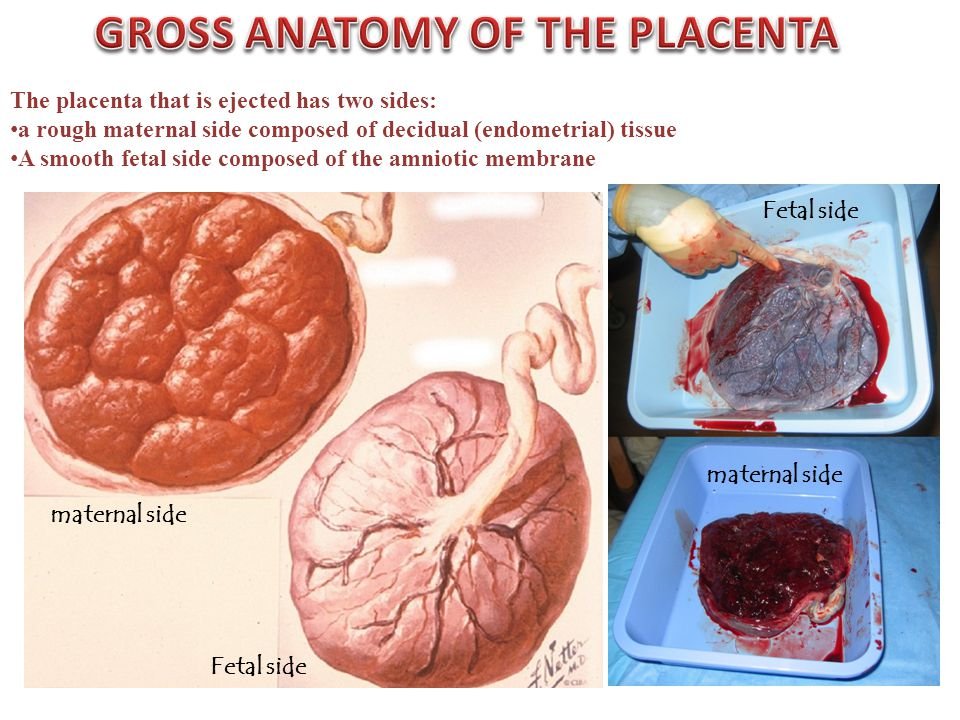
- The maternal surface of the placenta is arranged in about 20 lobes; each lobe is made up of lobules, each with a single chorionic villus and its branches. The maternal side is red and ‘meaty’ rich with maternal blood and decidua
- The fetal surface is white and shiny, as it is covered by the amnion membrane. Branches of the umbilical vein and artery can be seen spreading out from where the umbilical cord is inserted.
[Ref-DMW, Lesson plan volume 1/ page 20-21]
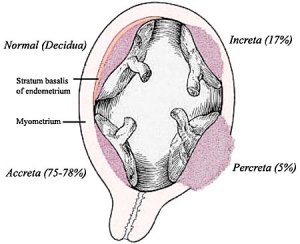
Placental abnormality:
1. Placenta Accreta – abnormal adherence, with absence of decidua basalis. The incidence of placenta accreta also significantly increases in women with previous cesarean section compared to those without a prior surgical delivery.
2. Placenta Increta occurs when the placenta attaches deep into the uterine wall and penetrates into the uterine muscle, but does not penetrate the uterine serosa. Placenta increta accounts for approximately 15-17% of all cases.
3. Placenta Percreta – placental villi penetrate myometrium and through to uterine serosa.
4. Placenta Previa – In this placenatal abnormality, the placenta overlies internal os of uterus, essentially covering the birth canal. This condition occurs in approximately 1 in 200 to 250 pregnancies.
5. Vasa Previa (vasa praevia) placental abnormality where the fetal vessels lie within the membranes close too or crossing the inner cervical os (opening). This occurs normally in 1:2500-5000 pregnancies and leads to complications similar too those for Placenta Previa.
6. Abruptio Placenta a retroplacental blood clot formation, abnormal hemorrhage prior to delivery.
7. Chronic Intervillositis (massive chronic intervillositis, chronic histiocytic intervillositis) Rare placental abnormality and pathology defined by inflammatory placental lesions, mainly in the intervillous space (IVS), with a maternal infiltrate of mononuclear cells (monocytes, lymphocytes, histiocytes) and intervillous fibrinoid deposition.
8. Hydatidiform mole placental tumor with no embryo development. Several forms of hydatidiform mole: partial mole, complete mole and persistent gestational trophoblastic tumor. Many of these tumours arise from a haploid sperm fertilizing an egg without a female pronucleus (the alternative form, an embryo without sperm contribution.
Pathology of placenta:
1. Chronic Villitis can occur following placental infection leading to maternal inflammation of the villous stroma, often with associated intervillositis. The inflammation can lead to disruption of blood flow and necrotic cell death.
2. Massive Chronic Intervillositis (MCI) – maternal blood-filled space is filled with CD68- positive histiocytes and an increase in fibrin, occuring more commonly in the first trimester.
3. Meconium: Myonecrosis prolonged meconium exposure leads to toxic death of myocytes of placental vessels (umbilical cord or chorionic plate).
4. Neuroblastoma a fetal malignancy that leads to an enlarged placenta, with tumor cells in the fetal circulation and rarely in the chorionic villi.
5. Thrombophilias (protein Cor S deficiency, factor V Leiden, sickle cell disease, antiphospholipid antibody) can generate an increased fibrin/fibrinoid deposition in the maternal or intervillous space, this can trap and kill villi.
Placenta examination:
Pathological examination of the placenta is performed for fetal, maternal, and placental indications. The purposes are to identify fetal or maternal disease, to provide prognosis for the current and future pregnancies, to evaluate the effect of maternal disease on the pregnancy, and for legal considerations.

Importance of placenta examination:
It is necessary to examine the placenta in two conditions at least: when the fetus is still born or dies in the neonatal period, and when there is a gestational or a neonatal pathology. Placental examination is essentially macroscopic.
1. It is recommended to practice it on fresh placenta, so that cytobacteriological investigation can be done.
2. Complete pathologic evaluation of the placenta provides valuable information for perinatal care for the obstetrician, neonatologist, pediatrician, and family.
3. The principal abnormalities or lesions are described, with their clinical significance: shape abnormalities, pathology of the cord and membranes, vascular lesions (decidual haematoma, infarcts, perivillous fibrin deposition), chorioangioma, abscess.
4. Some more “genetical” aspects of the placentology are also approached, for instance chromosomal aberrations, or multiple pregnancies.
5. placenta examination is essential for determine:
a. Stillbirth (antepartum or intrapartum); if baby is not going for a post mortem
b. Late miscarriage.
c.. Severe fetal distress requiring admission to NNU.
d. Prematurity (less than 30 weeks gestation).
e. Intrauterine growth.
f. Maternal pyrexia (>38°C)
6. Referral of placenta for examination may be desirable for identifying:
a. Prematurity (30-36 weeks)
b. Placental abruption
c. Fetal congenital malformation
d. Morbidly adherent placenta
e. Twins or other multiple pregnancy (uncomplicated)
f. Abnormal placental shape (if clinically relevant)
g. Two vessel cord, etc.
h. Prolonged rupture of the membranes (more than 36 hours)
i. Gestational diabetes
j. Maternal group B streptococcus
k. Pre-eclampsia/maternal hypertension
i. Maternal coagulopathy
m. Maternal substance abuse.
Examination of the placenta:
1. Explain the procedure to the parents and ask if they want to observe.
2. Wash hands; wear an apron and gloves.
3. The delivery trolley is a good surface to use.
4. Lay out the placenta with the fetal surface uppermost noting shape, size, colour and smell.
5. The cord is then examined noting the length, the point of insertion and the presence of any knots.
6. Count the vessels in the cut end of the cord; the absence of one of the arteries can be associated with renal agenesis.
7. Observe the fetal surface for irregularities.
8. By lifting the cord and holding the placenta up, you can then observe the membranes and inspect for completeness. There should be a single hole present.
9. The placenta is returned to the surface and the membranes are spread out in order to look for extra vessels, lobes, or holes in the surface.
10. The amnion is then pulled back towards the cord, thereby separating the membranes to ensure that they are both present.
11. The placenta is turned over to inspect the maternal side.
12. The cotyledons are examined to ensure that they are all present, noting any areas of infarction or blood clots.
13. Estimate blood loss.
14. Take cord blood samples.
15. Weigh or swab the placenta if indicated.
16. Dispose of the placenta as per trust guidelines.
17. Clean away equipment.
18. Wash hands.
19. Discuss the findings with the parents.
Read More….