Classifications of Anaemia – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric nursing.
Pediatric nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Classifications of Anaemia
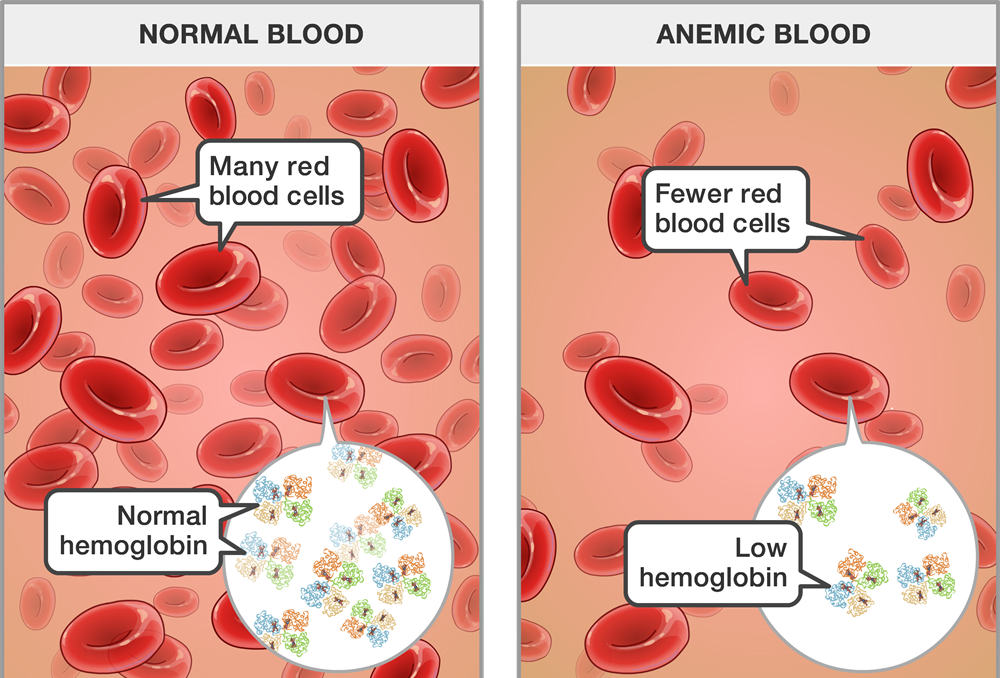
Anemia is when the level of healthy red blood cells (RBCs) in the body becomes too low. This can lead to health problems because RBCs contain hemoglobin, which carries oxygen to the body’s tissues. Anemia can cause a variety of complications, including fatigue (tiredness) and stress on the body’s organs.
Having fewer red blood cells than normal can happen because:
- The body is destroying red blood cells.
- Red blood cells are being lost.
- The body is producing red blood cells too slowly.
Anemia a fairly common blood disorder with many causes. They include inherited disorders, nutritional problems (such as an iron or vitamin deficiency), infections, some kinds of cancer. and exposure to a drug or toxin.
Definition of Anaemia:
It is a clinical condition characterized by the pale colouration of the skin & mucous membrane due to decrease concentration of Hb in the peripheral blood below the normal range for the age & sex of the person.
Or,
Anaemia is a clinical condition characterized by pale coloration of the skin and mucous membrane due to qualitative and quantitative deficiency of haemoglobin below the lower limit in the peripheral blood in respect of age and sex.
Or
Anaemia refers to a state in which the level of haemoglobin in the blood is below the normal range appropriate for age and sex.
Normal Hb level:
- Male: 13-18 gm/dl
- Female: 11.5-16.5gm/dl
- Children: 16-19 gm/dl
- At birth: 18-20 gm/dl
Site Where Anaemia is seen:
- Lower palpebral conjunctiva
- Dorsum of the tongue
- Buccal mucous membrane
- Palm of the hand
- Nail bed
- Sole of the feet
- Whole skin
Classifications of Anaemia:
A. Morphological classification: (On the basis of absolute values – MCV, MCH, MCHC)
a) Microcytic hypochromic anaemia: (MCV, MCH & MCHC)
- Iron deficiency anaemia.
- Thalassaemias.
- Sideroblastic anaemia.
- Anaemia of chronic disease.
b) Normocytic normochromic anaemia: (MCV, MCH & MCHC normal, but RBC & Hb)
- Aplastic anaemia.
- Haemolytic anaemia.
- Acute haemorrhagic anaemia.
c) Macrocytic anaemia: (↑MCV, MCHC normal)
- Megaloblasic anemia due to vtamin B12 deficiency.
- Megaloblastic anaemia due to folic acid deficiency.
B. Aetiological classification:
a) Haemorrhagic anaemia:
Acute haemorrhage: Trauma, surgical operation.
Chronic haemorrhage:
✓GIT lesion: PUD, hookworm infestation, haemorrhoids etc.
✓ Gynaecological disturbance: Menorrhagia.
b) Haemolytic anaemia: (Due to excess RBC destruction)
Intra-corpuscular defect: Thalassaemia.
Extra-corpuscular defect: Haemolytic disease of newborn.
c) Dyshaemopoietic anaemia:
- Due- to deficiency of essential elements of erythropoiesis:
✓ Iron deficiency anaemia.
✓Megaloblastic anaemia (due to deficiency of vitamin B12 & folic acid.
✓Nutritional anaemia in PEM (protein-energy malnutrition).
✓ Anaemia with scurvy (due to deficiency of vitamin C).
- Due to bone marrow disturbance:
✓ Aplastic anaemia.
✓Sideroblastic anaemia.
✓ Anaemia with renal failure (due to reduced erythropoietin secretion).
C. Clinical classification:
✓Anaemia with endocrine disorders.
a) Mild anaemia: When Hb
b) Moderate anaemia: When 12 to 9 gm /dl. (‘+’) Hb-9 to 6 gm/dl. (++)
c) Severe anaemia: When Hb Less than 6 gm/dl. (+++)
Common Causes of Anaemia of Children:
| Increased destruction of RBCs (Hemolytic anemia): | Thalassemia. Sickle cell disease. |
| Decreased RBC production (Bone marrow depression): | Primary: Hypoplasia or aplasia. Secondary: Irradiation, infections, chronic illness etc. |
| Impaired of RBC production: | Iron deficiency anemia. Folic acid deficiency anemia. Vitamin B12 deficiency anemia. |
| Increased blood loss (Hemorrhagic anemia): | Acute: Trauma, epistaxis, hemorrhagic disease of newborn and scurvy. Chronic: Hookworm infestation, bleeding piles, chronic dysentery. |
C/F of Anaemia:
| A. Symptoms of Anaemia |
|
| B. Signs of Anaemia |
|
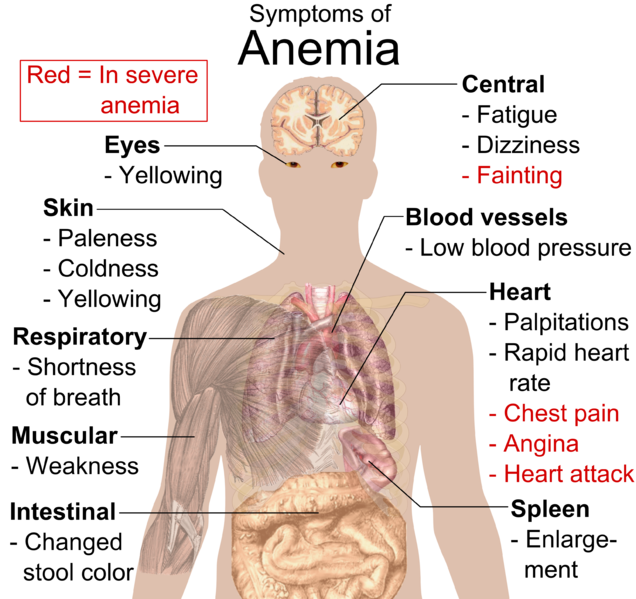
Complications of Anemia;
- Circulatory collapse and shock
- CCF
- Cardiac enlargement
- Systemic or local infections
- Rob stre
- Growth retardation
- Mental retardation or sluggishness with decreased attention span and intelligence
- Delayed puberty
(Ref: Paediatric Nursing, Parul Datta/34/320)
World Health Organization (WHO) proposed the cut-off points of Hb level for different age groups for the diagnosis of anemia –
1. Children 6 months to 6 years-11 g/dl
2. Children 6ycars to 14ycars- 12 g/dl
3. Above 14 years
- Male-13 g/dl
- Female-12 g/dl
Management of Anemia:
Medical Management of anemia depends upon the specifie cause of the condition.
Anemia due to excessive blood loss:
- Acute blood loss needs immediate control of bleeding
- Restore blood volume by IV infusion
- Blood transfusion along with treatment of shock
- Treat the cause of bleeding.
- Chronic blood loss usually produces iron deficiency anemia.
- The exact cause should be detected
- Treatment should be planned according to the specific cause.
Anemia due to excessive blood cell destruction:
- Requires the identification and treatment of specific hemolytic disorder.
Anemia due to depressed blood cell formation:
- Specific deficiency of iron, folic acid, vitamin B12, etc, should be detected and treatment to be done with replacement therapy of specific nutrients.
- In case of bone marrow depressions, the specific cause (like drugs, toxins) to be identified and treatment to be performed by removal of offending agents.
(Ref: Paediatric Nursing, Parul Datta/34/320)
Nursing Management of Anemia:
1. Nursing assessment is the comer stone of nursing interventions. It is done by obtaining details history to detect potential causes of the condition. Important aspects of assessment are-
History of present complaints
- Past illness
- Chronic diseases
- Presence of infections
- Worm infestations
- Exposure to medications
- Poisons
- Dietary habits
- Behavioral problems like pica and
- History of familial diseases
2. Physical examination to be done to exclude the presence of clinical features like pallor of skin and mucous membrane with other signs and symptoms related to anemia.
3. Assessment of anthropometric data (height, weight, MUAC, skin fold thickness, head and chest circumference)
4. Assessment of vital signs
5. Review of laboratory investigations are important to identify the problems and to implement the care.
(Ref by: Paediatric Nursing, Parul Datta/34/320)
Causes of Iron Deficiency Anemia in Children:
| Decreased iron stores: | Preterm, small for dates, twins. Repeated venous sampling Feto-maternal hemorrhage |
| Decreased intake: | Delayed weaning. Iron poor diet. |
| Decreased absorption: | PEM. Mal-absorption syndromes. Chronic diarrhea |
| Increased losses: | GI bleeding. Hookworm infestation. Peptic ulcer. Bleeding diathesis |
| Increased demand: | Prematurity.izu LBW. Recovery from PEM. |
Clinical Features of Iron Deficiency Anemia:
Symptoms:
- Pallor
- Irritability
- Fatigue
- Tiredness
- Listless
- Weakness
- Anorexia and
- Failure to thrive.
- There is usually vomiting, diarrhea and respiratory infections
Signs:
- Excessive pallor of the skin; conjunctiva and mucous membrane is found.
- Nails become thin, brittle and flat
- The child may have pica and atrophy of tongue papillae.
- Older children may present with koilonychia.
- In severe anemia spleen may enlarge.
- Cardiac enlargement with soft systolic (hemic) murmur may be detected.
- The child may be manifested by unhappiness, lack of co-operation and short attention span with poor school performance.
(Ref: Paediatric Nursing, Parul Datta/34/320)

Prevention of Iron Deficiency Anemia;
- Adequate antenatal care for prevention of maternal anemia and iron-folic acid supplementation to all antenatal mother.
- Prevention of preterm delivery or low-birth weight, and control of infections in prenatal, natal and neonatal period.
- Introduction of semi-solid and solid foods from 4 to 6 months of age as complementary feeding.
- Universal immunization to all children to prevent chronic illness.
- Iron-folic acid supplementation to the children and adolescent girls.
- Adequate treatment of parasitic infestations, chronic illnesses and IDA
- Improvement of living condition by avoidance of open-air defecation, practicing environmental sanitation, hygienic measures, wearing of shoes, balanced diet and preventive measures of nutritional deficiencies.
Prevention/Intervention of Anaemia:
An estimation of haemoglobin should be done to assess the degree of anaemia. If the anemia is severe (Hb 10 gm/dl), high dose of iron or blood transfusion may be necessary. If Hb between 10 to 12 gm/dl, the other interventions are –
Iron and folic acid supplementation:
➤ Mothers: 1 tab of iron & folic containing 60 mg of elemental iron (180 mg of ferrous sulfate) 0.5 mg of folic acid should be given daily up to 2-3 months.
➤ Children: 1 tab of iron and folic acid containing 20 mg of elemental iron (60 mg of ferrous sulfate) & 0.1 mg of folic acid should be given daily.
Iron fortification: Iron fortification with salt by adding ferric ortho-phosphate or ferrous sulfate with Na bisulfate. Iron fortification has many advantages over implementation a salt is a universally consumed dietary item.
Other strategies: (Long term measures)
- Changing dietary habits
- Control of parasites
- Nutrition education.
Detrimental Effects of Nutritional Anaemia:
The detrimental effects of anaemia can be seen in 3 important areas:
1. Pregnancy: Anaemia increases the risk of maternal and foetal mortality and morbidity. Conditions such as abortions, premature births, post-partum haemorrhage and low birth weight were especially associated with low haemoglobin levels in pregnancy.
2. Infection: Anaemia can be caused or aggravated by parasitic diseases, e.g., malaria, intestinal parasites. Further, iron deficiency may impair cellular responses and immune functions and increase susceptibility to infection.
3. Work capacity: Anaemia (even when mild) causes a significant impairment of maximal work capacity.
Risk of Nutritional Anaemia:
Some groups of people are more likely to be iron or folate deficient than others. They are ‘at risk’ of anaemia.
High-risk groups are:
- Women, especially during pregnancy or soon after delivery,
- Babies who are low birth weight or not breastfed,
- Young children- especially if they are malnourished,
- Adolescents, who are growing fast, especially girls,
- Older men and women, especially if they are poor.
Consequences of Anaemia:
| All individuals: |
|
| Infant, pre-school and school children: |
|
| Pregnant women and their fetuses: |
|
| In summary consequences of anaemia: |
|
Benefits of Anaemia Prevention and Control:
All individuals:
- Increased immunity and low morbidity from infectious diseases.
- Improved cognition.
- Improved quality of life.
In-case of pregnant women (PW) and foetus:
- Decreased risk of complications during delivery, preterm delivery, LBW, maternal and neonatal death.
- Increased iron stores in infants and lower risk of anaemia in infancy and children.
In case of infants and children:
- Improved growth.
- Improved BCD.
- Risk of IDD.
- Improved child survival.
- Better iron store for future pregnancies (adolescent).
Read more: