Skeletal Traction – An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
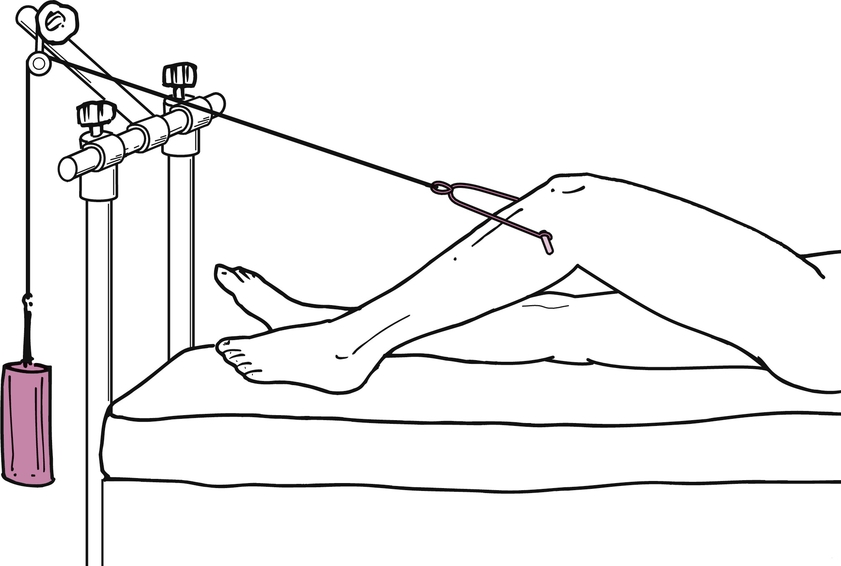
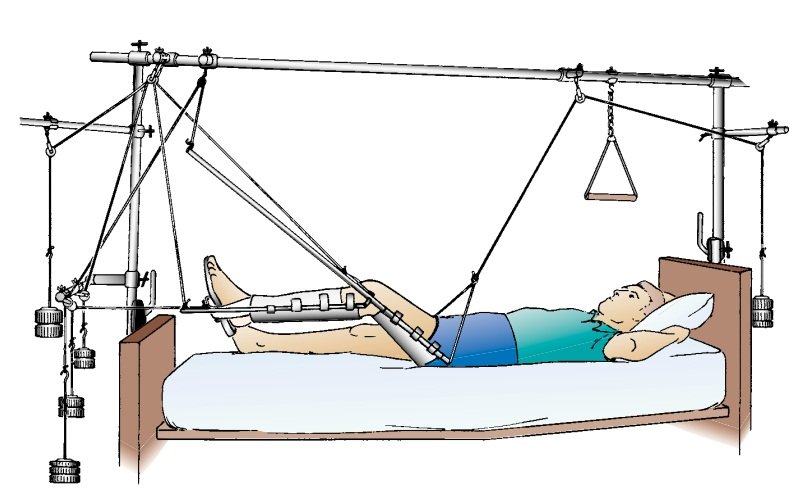
Skeletal Traction
Skeletal traction:
Skeleton is the bony frame work of the body in which Steinmann pin or K-wire is applied to re-align the bone fragments or repositioning of displaced part of the body is known as skeletal tractions.
Sites of skeletal tractions:
1) Upper and lower end of the tibia.
2) Lower end of the radius.
3) Lower end of the humerus.
4) Caslcenium.
5) Below the olicranon.
6) Distal end of the radius and ulna. 7) Through the middle metacarpals.
8) Supracondylar area of femur.
9) Throughthe distal phalanx of toes..
10) Skull traction.
(Ref- Luckmann and Sorensen, Medical-Surgical Nursing, 2 P-1669)
Weight required for skeletal traction:
1) Initially 1/7th of the body weight.
2) Then after radiological findings 1/10th of body weight.
Equipment of skeletal traction:
1) A Steinmann’s pin.
2) A Bohler’s Stirrup.
3) A Pulleys.
4) Appropriate length of ropes.
5) Appropriate weight for traction.
6) A rod to hang the pulleys in the bed.
Common pins used in skeletal traction:
1) Steinmann’s pin: It is a rigid stainless steel pin 4-6 mm in diameter. Bohler s stirrup allows the direction of the traction to be varied without turning the pin in the bone.

2) Denham pin : This pin is threaded in the center and engage the bony cortex. It reduces the risk of pin sliding and is useful in cancellous bone like calcaneum and osteoporotic bones

3) K-wire: It is a small diameter and commonly used in upper limbs
[Ref-John Ebnezar’s “Text book of Orthopaedics” 4″ edition, page-67]
Observation of patients with traction:
Learn to make routine observation each time nursing care time nursing care is given until such observation become habitual that they are no longer conscious. Learn to ask yourself these questions.
1. Are the circulations and nerve status of the extremity adequate?
2. Is the condition of the skin around the tape and strape are satisfactory?
3. Are you using your nose as well as your eyes to detect signs of trouble, are there any distinctive odors of macerating soft tissue and infection?
4. Are the tapes slipping or is the wrapping coming loose? 5. Is there any pressure on the popliteal region?
6. Is the heel free of pressure?
7. Is there any pressure over the outer aspect of the head of the fibula?
8. Is there sufficient counter traction?
9. I the angle of elevation of the heel enough or too much?
10. In balanced skeletal traction, hip flexion 20 degree or less?
11. Is there any deformity in fracture site?
12. Is the patient comfortable and warm?
13. Is the patient having an undue amount pain? 14. Is the patients body is correctly positioned.
15. Are there complications due to prolonged bed rest and reduced activity?
(Ref-Lippincott, Adult Orthopedic Nursing, I” edition,P-157)
General principles on the care of traction equipment:
The following are the general principles that apply to the care of all traction equipment to provide a safe environment for the patient traction:
1. Check the weakness of the traction cord never reuse a cord.
2. Tie knots properly and then secure knots with adhesive tape.
3. Check for correct poundage, apply weights in a slow manner, avoid any bumping or jerking of weights and make sure weights hang free of any obstruction.
4. Make sure all parts of the traction equipments are working correctly,
a. Never oil any pulley without notifying the patients physian first.
b. Apply manual traction if any piece of the equipment needs to be readjusted or replaced.
5. Check counter traction and ensure that the patient does not slide into the headboard, footboard, or side of the bed.
6. Check for obstructions that may interfere with the pull of the traction, such as knots pressing against the pulleys, traction pieces such as spreader bars, the footplate, or splints coming in contact with the bed frame, or bed linen on top of traction straps and ropes.
7. Check the line of pull and be certain that fracture fragments are3 ion correct alignment.
8. In continuous traction, make sure the pull is maintained 24 hours a day.
9. Check the position of the patients for correct body alignment, comfort, support for all body’s parts and undue stress or the pull
(Ref-Lippincott, Adult Orthopedic Nursing, I” edition, P-157)
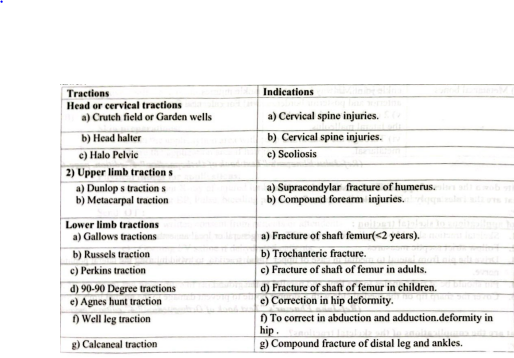
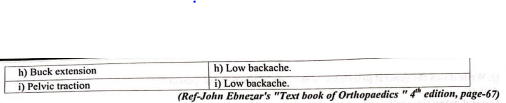
Exact point and indications of skeletal tractions:
Rules of applications of skeletal traction:
1. Skeletal traction should be applied in a major OT under general or local anaesthesia
2. Follow strict aseptic measures.
3. Drive the pin from lateral to medial in case of upper tibial traction, to avoid injuring the lateral popliteal nerve.
4. Pin should be at right angles to the limb and parallel to the ground.
5. Cover the sharp tip on the medial side with a stopper bottle to prevent damage to the normal limb.
(Ref-John Ebnezar’s “Text book of Orthopaedics” edition, page-67)
Complications of skeletal tractions:
A) At the time of application:
1) Anaesthetic problem.
2) Vasovagal shock.
3) Very rarely death due to vasovagal shock.
B) During application:
1) Injury to nerves (Lateral poplietal nerve)
2) Injury to the vessels.
3) Injury to the muscles ligaments, and tendons
4) Injury to the epiphysis in children(Upper tibial epiphysis)
5) Pain due to intraosseus pressure and atmospheric pressure due to the hole made in the bone.
C) When pin in situ:
1) Infection due to improper aseptic measures
2) Migration-due to loosening
3) Breakage: Thin pin or more weight.
4) Bending-same reasons as above.
5) Loosening- due to osteoporosis infection etc.
6) Distraction of fracture fragements due to excessive weight.
D) Late effects:
1) Pin tract infections.
2) Chronic osteomyelitis with ring sequestra at the site.
3) Genu recurvatum due to damage to the anterior epiphysis of the tibia in children
4) Depressed scar.
(Ref-John Ebnezar’s “Text book of Orthopaedics” edition, page-68)
Prepare the patients before applications of Skeletal tractions:
A) Mental preparation:
- Explain the benefits of traction.
- Give assurance that it has less adverse effect.
- Improve confidence for himself that doctor and nurse will do the best.
- Encourage to maintain relaxation techniques.
B) Physical preprations:
Skin preparations:
- Clean the applicaytion area with soap and water.
- Shave the application area if hair is present.
- Throughly scrub the area with an antiseptic solution.
Physical fitness for applications:
a) Take out X-ray of injured lumb and blood for Te, ESR,HB% etc
b) Monitor BP, Pulse, bleeding points, deformity of the limb and pain and swellings.
Send OT:
a) Take written consent from patients or attendents. b) Remove jwellary, nail polish (To see the cyanosis).
c) Opening IV saline if dehydrated patients
d) Send the Ortho-OT in timely.
Procedure of skeletal traction:
Nursing care management of the patients with skeletal tractions:
A) Assessment:
1) Assessment of correct position of the tractioned limb
2) Assess and monitor correct weight is applied.
3) Assess the pin sites for any infections or discharge.
4) Assess the mental condition of the patients.
5) Frequently monitoring of skin integrity.
6) Observe any signs of pain
7) Assess the function of nerve on the applied limbs.
B) Nursing diagnosis:
1) Impaired physical mobility related to traction therapy and underlying pathology.
2) Risk for impaired skin integrity related to pressure on soft tissues.
3) Pain and discomfort related to trauma and traction.
4) Risk of development of infections at the site of insertion of the skeletal pin.
5) Knowledge deficit about care of traction patients.
6) Risk of injury related to skeletal pin.
7) Self care deficit ( bathing/hygiene) related to immobilization of device.
8) Cutting out of skeletal pin from the bone with displacement of fracture site.
C) Nursing intervention:
1) Minimizing the effects of immobility:
a) Keep the patients in complete bed rest.
b) Keep the affected limb in comfortable position.
c) Encourage the patients to exercise in all body parts.
d) Patients can lying on supine position.
e) Weight of traction frequently monitoring.
f) To help reduce stress on back use pillows under the knee.
2) Maintaining skin integrity:
a) Assess the skin condition at bony prominence.
b) Observe any skin breakdown.
e) Apply message on the area to improve circulation.
d) Prevent pressure on the calf muscle and elevate twice daily for development of DVT.
e) Change position 2 Hourly.
f) Avoid wrinkle bed under the leg.
g) Provide backrubs on the bony prominence of the body.
3) Relieving Pain:
a) Maintain appropriate weight and position of the limb reducing pain and swellings.
b) Keep the injured limb elevated.
e) Purcuss on the pin if patients complaints pain at pin site that evidence of pain
d) Assess the level of pain with severity.
e) Give analgesics according to doctors order.
4) Improve self care:
a) Assist the patients in bowel and bladder elimination
b) Keep the bed pen/urinal in the bed.
c) Take a rope where he can raise from the bed.
d) Helps the patients in dressings and hygiene.
e) Helps him to feeding
f) Exercise of all body parts to regain all the function of the muscle and joint.
5) Avoiding infection at pin site:
a) Care of pin site:
a) Inspect pin site everyday.
b) Note skin tension in pin site.
c) Note loosen of pin.
d) Note placement of pins.
b) Pin site care:
a) Regular inspect the skin.
b) Clear the pin site with antiseptic solution.
c) Watch for signs of infections e.g. pus, swelling, redness etc.
d) Avoid touching in the pin site in open hand.
e) Care of appliance includes, keeping the frame clean adjusting the pulleys cord etc.
c) Pharmacological measures: Use of prophylactic (Prevent the development of complications) antibiotics according to doctors order.
6) Prevent cutting out of skeletal pin:
a) Regular inspect the pins area for-Loosening, bone cutting.
b) Check the area by X-ray for identifying the improvement bone fixing.
e) Observe and maintain the correct weight regarding the patient’s body weight.
7) Injury prevention in skeletal:
a) The sharp end of the Steinmann pin needs to be protected with an empty injection vial bottle to prevent injury to the normal limb.
b) You can cover the sharp end by adhesive tape.
(Ref-Lippincott, Adult Orthopedic Nursing, I edition, P-174+ BT. Basavanthappa, Orthopaedics for nurses, Page-132)

Prevention of skeletal pin site infections:
a) Care to pin sites:
i. Inspect the pin sites everyday.
ii. Note skin tension in pin sites.
iii. Note placement of pins.
iv. Report loosing pins. And loosing pin should be replaced.
v. Note any signs of infection if there is discharge.
b) Wound care:
i. Regular inspect of the skin.
ii. Change dressing everyday.
iii. Clean the wound with povisep solution.
iv. Avoid touching the wound in open hand.
v. Always use of sterile gauze, cotton, bandage.
vi. During dressing remove dead cells, if present.
vil. If infection or pus in the wound wash with 50% N/S +50% H2O2.
c) Sterile technique:
i. Use of sterile instrument, gauze.
ii. Encourage patients to maintain personal hygiene.
iii. Change bed cloths regularly.
iv. Keep area of external fixator clean and dry.
d) Pharmacological care:
i. Investigate Blood for TC, DC, ESR, RBS, Urine R/M/E etc.
ii. Give prophylactic antibiotic to prevent development of secondary infections.
iii. Use of topical antibiotic (If necessary).
iv. Control blood sugar if the pts is DM.
Daily checklist for above patients:
a) Daily checklist for above patients:
1) Check the peripheral pulse everyday. Check the function of the distal limb.
2) Check the pin sites for-infections, loosening of pin. 3) Everyday record-pulse BP, temperature, respiration.
4) Check the corerect alignment of the traction limb.
5) Check the traction weight-less/more/Adequqte.
6) Check the neurovascular status of the patients.
7) Check the weakness in the traction cord.
8) Check the pressure point of the body for bed sores.
b) Prevention of DVT:
1) Active exercise to the foot and ankle.
2) Massage of the calf muscle.
3) Elevation of the legs.
4) Performs Homans test for early detection of DVT.
5) Firm compression of the calf muscle by application of elastrocrepe bandage.
6) Measures to prevent chest complications like hypostatic pneumonia.

c) Complications due to long standing confinement in bed:
1) Chest problems-pneumonia
2) Bedsores
3) Renal stones.
4) DVT.
5) Joint stiffness.
6) Mental depression.
7) Development of osteoporosis.
(Ref- BT. Basavanthappa, Orthopaedics for nurses, Page-134)
Counter tractions:
Traction force will overcome muscle spasms only if another force is acting in the opposite direction as counter traction.
(Ref-John Ebnezar’s. “Text book of Orthopaedics”. 4 edition, page-69)
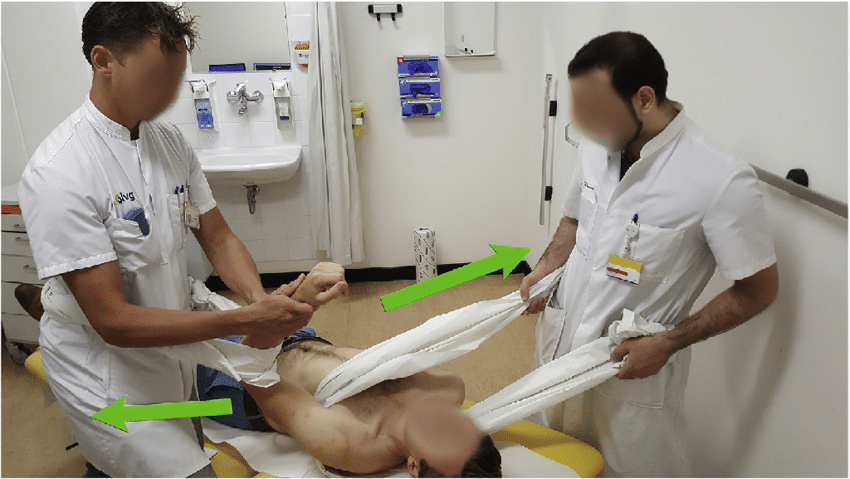
Types of counter tractions:
There are 2 types of counter tractions:
1) Fixed tractions: Here counter tractions is achieved through an appliance which obtains a firm purchase on a part of the body. This can maintain but can not obtain reduction. E.g. Fixed traction on a Thomas splint for a fracture shaft of femur,
2) Balanced tractions: here weight of all body part or part of the body nacting under the influence of gravity is utilized to provide counter traction. This can be achieved by raising the foot end of the bed. This can both maintenance and reduction ability.
(Ref-John Ebnezar’s, “Text book of Orthopaedics” edition, page-69)
Read more:
