Drug Receptors – This book covers the entire syllabus of “Pharmacology” prescribed by BNMC- for diploma in nursing science & midwifery students. We tried to accommodate the latest information and topics. This book is an examination set up according to the teachers’ lectures and examination questions.
At the end of the book, previous questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourish. The unique way of presentation may make your reading of the book a pleasurable experience.

Pharmacodynamics
Pharmacodynamics (Gr. Pharmacon: drug; dynamis; power). Pharmacodynamics is the study of drug effects.
In other words, “Pharmacodynamics is what drugs do to the body”.
Definition
Pharmacodynamics describes the actions of a drug on the body and the influence of drug concentrations on the magnitude of the response.
Or,
It covers all the aspects relating to what the drug does to the body’. It is the study of drugs-their mechanism of action, pharmacological actions and adverse effects.
It starts with describing what the drugs do, and goes on to explain how they do it. Thus, it attempts to elucidate the complete action-effect sequence and the dose-effect relationship. Modification of the action of one drug by another drug is also an aspect of pharmacodynamics.
Principles of Drug Action
Drugs (except those gene based) do not impart new functions to any system, organ or cell; they only alter the pace of ongoing activity. However, this alone can have profound medicinal as well as toxicological impact. The basic types of drug action can be broadly classed as:
➤ Stimulation: Some drugs act by increasing the activity of specialised cells, e.g. adrenaline stimulates the heart resulting in an increase in heart rate and force of contraction.
➤ Depression: Some drugs act by decreasing the activity of specialized cells, e.g. alcohol, barbiturates, general anaesthetics, etc. depress the central nervous system.
➤ Irritation: Certain agents on topical application can cause irritation of the skin and adjacent tissues. When an agent on application to the skin relieves deep seated pain, it is known as counterirritant, e.g.
- eucaliptus oil, methyl salirylate, etc. They are useful in sprains, joint pain and myalgia. They exert their action by:
- Reflexly increasing local circulation in deeper structures. Blocking impulse conduction in the spinal cord.
➤ Replacement: When there is a deficiency of endogenous substances, they can be replaced by drugs, e.g. insulin in diabetes mellitus, thyroxine in cretinism and myxedema, etc.
➤ Cytotoxic: Drugs are selectively toxic for the infecting organism/cancer cells, e.g. antibiotics/anticancer drugs.
Drug Receptors
Receptor are macromolecular structure protein in nature situated in the cell surface or inside the cell which are chemo recognition properties for specific drug, which are reversibly or irreversibly bind
Classification of Receptor
1. According to location:
- Membrane receptor – Alpha and beta adrenoceptors, cholinergic receptors
- Cytoplasmic receptor-steroid hormone receptors
- Nuclear receptor – thyroid hormone receptor
2. According to activity:
- Active receptor – adrenoceptors,cholinergic receptor
- Spare or receptor
- Silent receptor – plasma protein
3. According to both molecular structure and the nature of the transduction mechanism:
Type 1: Direct Ligand-gated channel type a)Nicotinic acetylcholine receptor,
b)GABA receptor
Type 2: G-protein coupled type.
b) Neuropeptide receptor
a) muscarinic acetylcholine receptor,
Type 3:- Tyrosine kinase type a) Insulin receptor, b) Various growth factors receptors.
Type 4:- Intracellular receptors – a)Steroid receptors, b)Thyroid receptors,
Drug Receptors Binding
Drugs bind with receptor by any of the following two types of bonds:
A. Weak bond (reversible binding):
- Hydrogen bonds.
- Vander-waals bonds
- Hydrophobic bonds
Characteristics of weak bond
1. Weak and reversible bond between drug & receptor: Acetylcholine → Muscarinic receptor
Morphine Opioid receptor Propranolol → ẞ adrenoceptor
2. Bond energy is low (0.5 Kcal/mole)
3. Action of drug is of short duration.
4. Higher concentration of agonist can displace antagonist from receptor binding (as binding is reversible).
5. Non-covalent interactions of high affinity may also appear to be essentially irreversible.

B. Strong bond (irreversible binding): Covalent bonds
Characteristics of covalent bonds
1. Binding between drug and receptor is firm and irreversible- Phenoxybenzamine → a adrenoceptor
2. Bond energy is high (100 Kcal/mole)
3. Duration of drug action is frequently but not necessary prolonged.
4. Higher concentration of agonist cannot modify the action of antagonist
Regulation of Receptors:
Receptor super-sensitization
Hyperactivity or super-sensitivity to receptor agonist is also frequently observed to follow reduction in the chronic level of receptor stimulation.
Super-sensitivity can results from –
- Long term administration of antagonists
- Synthesis of additional receptors
Receptor desensitization
Continued stimulation of receptors with agonist generally results in a state that the effect that follows continued or subsequent exposure to the same concentration of drug is diminished
Receptor desensitisation is due to:
- Phosphorylation of the receptor.
- Destruction of the receptor, or
- Its relocalisation within the cell.
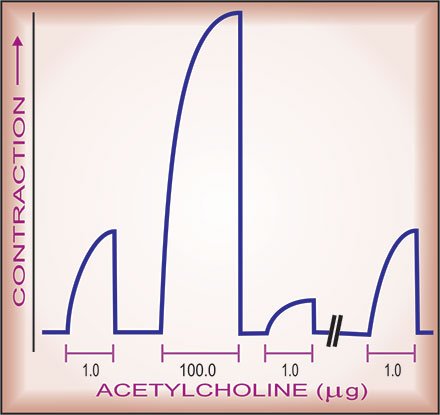
[Contractile responses of frog’s rectus abdominis muscle to acetylcholine. Note that shortly after exposure to a high
(100 fold) dose of the agonist, the response is markedly attenuated, but is regained if sufficient time is allowed to elapse).
Receptor Families
1. Ligand-gated ion channels (inotropic receptors)
2. G-protein-coupled receptors (metabotropic receptors)
3. Enzymatic receptors
4. Receptor-regulating gene expression (transcription factors) or the nuclear receptor.
Functions of Receptors
These can be summarized as:
1. To propagate regulatory signals from outside to inside the effector cell when the molecular species carrying the signal cannot itself penetrate the cell membrane.
2. To amplify the signal.
3. To integrate various extracellular and intracellular regulatory signals.
4. To adapt to short term and long term changes in the regulatory melieu and maintain homeostasis.
Terms Related With Pharmacodynamics
➤ Affinity: The ability of the drug to get bound to the receptor is known as affinity
➤ Intrinsic activity: The ability of the drug to produce pharmacological action after combining with the receptor is known as intrinsic activity of the drug.
➤ Agonist: A drug that is capable of producing pharmacological action after binding to the receptor is called an agonist.
➤ Agonist has high affinity + high intrinsic activity (e.g. morphine and adrenaline).
➤ Antagonist: A drug that prevents binding of agonist to its receptor or blocks its effect is called an antagonist. It does not produce any effect itself.
➤ Competitive antagonist has high affinity without intrinsic activity (e.g. naloxone and atropine). It produces receptor blockade.
➤ Partial agonist: A drug that binds to the receptor but produces an effect less than that of an agonist is called partial agonist. It blocks the effect of agonist.
➤ Partial agonist has affinity + less intrinsic activity (e.g. pindolol and buprenorphine).
➤ Inverse agonist: It has full affinity towards the receptor but produces effect opposite to that of an agonist, e.g. benzodiazepines produce antianxiety and anticonvulsant effects by interacting with benzodiazepine (BZD) receptors, but p-carbolines act as inverse agonist at BZD receptor and produce anxiety and convulsions.
Inverse agonist has affinity + intrinsic activity between 0 and-1

Factors Modifying Drug Action
There are a number of factors which can influence drug response. Individuals may often show quantitative variations in drug response but rarely show qualitative variations.
A. Non genetic factors:
1. Age
2. Disease
3. Pregnancy
4. Lactation
5. Circadian rhythm
6. Body temperature
7. Nutritional status
8. Occupational exposures
9. Drug factors
10. Food
B. Genetic factors:
Inherited factors causing different responses (increase, decrease) to drugs are commonly biochemical because single genes govern the production of enzymes.
1. Genetic pleomorphism includes –
- Low hepatic acetyl transferees activity
- Fast/slow acetylators (isoniazide, hydrallazine, procainamide),
- Enzyme involved: Acetyltransferase (acetylation).
- Slow acetylator (isoniazide); Peripheral neuropathy.vide
- Fast acetylator (isoniazide): Hepatotoxic.
2 Genetically determined defect in plasma cholinesterase
- Enzyme involved: Pseudocholinesterase (hydrolysis)
- Suxamethonium: Less metabolised by the defective enzyme.
- So, prolong neuromuscular blocking action leading to apnoea.
3. Genetically determined defect in oxidative metabolism of drug
- Enzyme involved: Cytochrome P450 oxidase (Oxidation)
- Beta-blockers (slow oxidation): Toxic action.
- Debrisoquine (slow oxidation): Orhostatic hypotension.
4. Glucose-6, phosphate dehydrogenase deficiency
- Acute haemolysis occurs when exposed to some drugs
5. Racial differences
6. Heritable condition
- Resistant to coumarin anticoagulants
- Resistant to suxamethonium (increase pseudocholinesterase activity)
- Resistant to vitamin D.
- Bacterial resistant to drug is genetically determined.
Non Genetic Factors
Sex
Male: Drugs rapidly metabolises because of testosteronc predominance. So less duration of action.
Female: Less rapidly metabolism occurs; so relatively longer duration of action. Lipid soluble drugs are largely accumulated in females due to more fat in their body.
Age
Drugs tend to produce greater and more prolonged effects al the extremes of age (with some exceptions). The main reason that affects drug action is that drug metabolism and renal function are less efficient, in babies and old peoples.
Pharmacodynamic variation with age
1. Receptor mediated drug action
- Neonates, adult: Average
- Old age: Number of receptors reduced, so less action.
2. Baroreceptor reflex: reduced in old age, so hypotensive drugs tend to cause orthostatic hypotension.
3. CNS action: (sedation, respiratory depression)
- Neonates: More
- Young adult: Average
- Old age: Less
Pharmacokinetic variation with age
| Absorption (GIT,rectum, IM) | Neonates Young age Old age | Less More Less |
| Metabolism | Neonates Young age Old age | Less Sufficient Decreased |
| Distribution | Neonates Young age Old age | Consume less drug Average Consume more drug |
| Excretion | Neonates Young age Old age | Less Average Decreased noudisieib al |
Food
- Food (especially fatty food) delays gastric empty so less absorption ( ampicillin, rifampicin)
- Calcium (in milk) interferes absorption of tetracycline by chelation.
- Specific dietary factors induce drug metabolising enzymes, e.g. Alcohol,

Methy-xanthines (Coffee, Cola, drinks, chocolate). Beef, Cabbage.
Drug Factors
1. Nature of drug
2. Routes of administration:
- Oral: onset of action and Bioavailability is variable.
- Parenteral: Immediate onset (IV), Bioavailability 100% (IV).
3. Time and frequency of doses:
- Before meal: Absorption of some drugs is better; so more action is obtained (e.g Captopril, Ampicillin).
- After meal: Amoxacillin is better absorbed
4. First pass metabolism:
- Some drugs undergo first pass metabolism (metabolism of drug before entering into the systemic circulation); therefore less bioavailability and so less duration of action.
5. Drug formulations:
- Slow and sustained release preparation (long action with less frequent dose)
- Prodrug.
- Drug with double strength (os), e.g. Cotrimoxazole-DS, Antacid-DS.
Pathological Condition
Diseases can cause altered handling of drugs by the body (pharmacokinetic variation) and/or altered sensitivity to drugs (pharmacodynamic variations).
Pharmacodynamic alterations
1. Disease that influence receptors:
- Myasthenia gravis.
- Nephrogenic diabetes mellitus.
- Familialhypercholesterolaemia.
2. Disease that influence signal transduction mechanism:
- Pseudohypo-parathyroidism
- Hypothyroidism (life of Digoxin, Antipyrine, Methimazole
Pharmacokinetic alterations
1. In absorption:
- Gastric stasis (e.g. migraine)
- Malabsorptionsyndrome
- Oedema of ileal mucosa (e.g. Heart failure. Nephrotic syndrome)
2. In distribution:
- Chronic renal failure: Altered plasma protein binding (phenytoin).
- Meningitis: Impaired blood brain barrier to penicillins.
3. In metabolism:
- Hepatic cirrhosis: reduced metabolism of drugs,
- Porphyria: increased hepatic drug metabolism
4. In excretion: acute/chronic renal failure.
Read more: