Initial Antenatal Visit – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Antenatal Assessment of Woman and baby
Initial Antenatal Visit
At every antenatal visit, the midwife should use the same framework to guide her care:
A. Information gathering (including taking history);
B. Examination and assessment;
C. Tests and screening:
D. Decision making;
E. Health promotion/information and education.
A. Information gathering:
- At this initial AN visit, the midwife will gather basic social/personal data and socio- economic information (name, birth date, living circumstances, etc.);
- Gather information on the woman’s environmental issues;
- Symptoms of discomforts related to pregnancy; The lesson has already discussed that the midwife calculate EDD and current gestation;
- The remainder of the comprehensive history which is taken at the initial AN visit is addressed in the next section.
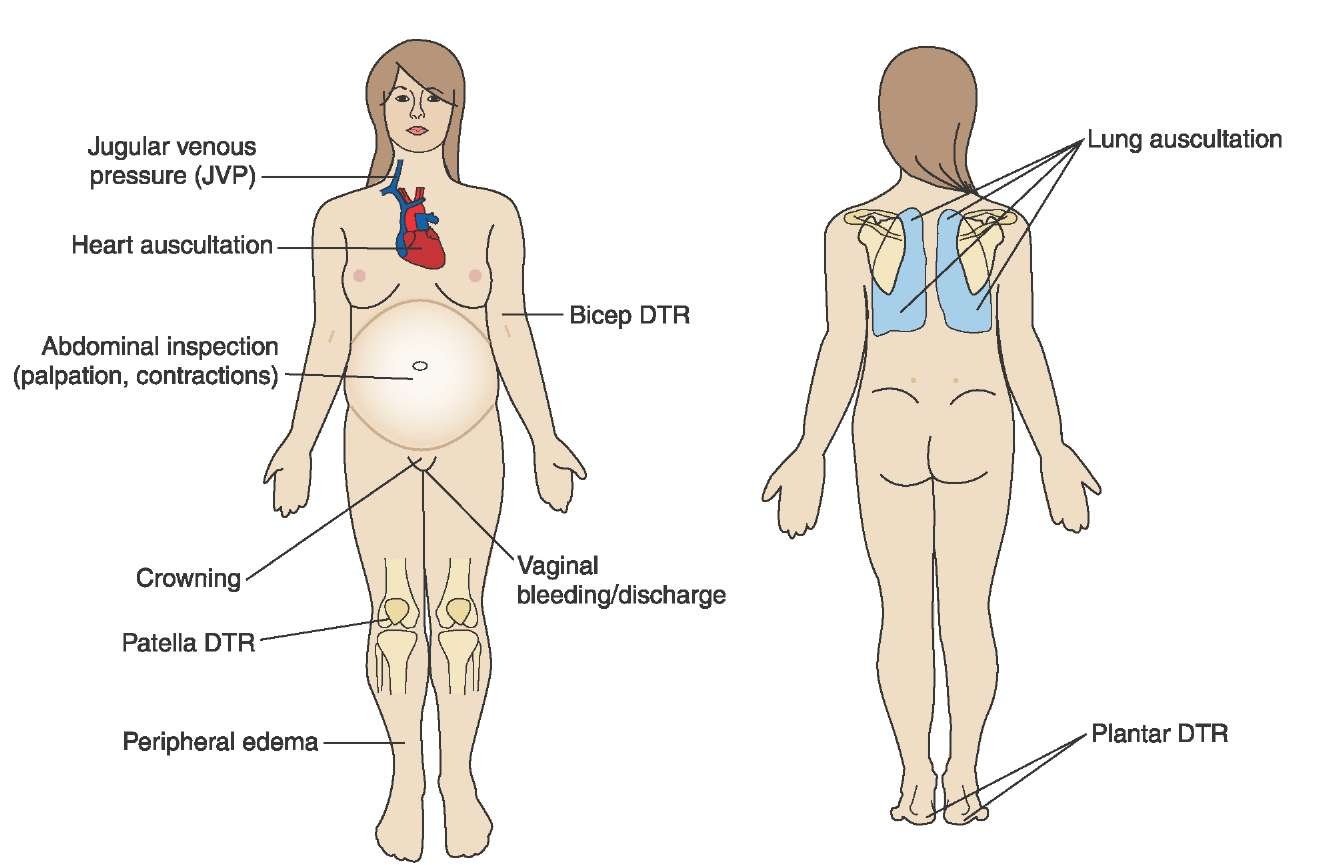
B. Examination and assessment:
- At this initial AN visit, it is important to obtain baseline data, so later changes can be measured against this initial baseline;
- height and weight;
- blood pressure check;
- general appearance;
- physical health status is reviewed to identify any health issues;
- nutritional status and examine for pallor (anaemia);
- breast examination;
- vaginal discharge/bleeding;
- legs examined for oedema or varicosities;
- abdominal palpation;
- assessment of uterine size;
C. Tests and screening:
- Blood tests
- Urine tests
- Other possible tests
⚫ for sexually transmitted infections
⚫ Ultrasound scanning
⚫ Nuchal translucency
⚫ Chorionic villus sampling (CVS)
⚫ Amniocentesis (Amnio)
D. Decision making:
- Antenatal care:
- Place of birth: advocate for birth in a health facility;
- Birth preparedness;
- Emergency readiness;
- Antenatal risk assessment.
At this first visit, one of the important decisions to make is that the woman will attend for future antenatal care. She, and importantly her husband and older members of the family, have to understand the advantage of good quality antenatal care in preventing, or detecting early, any potential complications which could endanger mother or baby. So using the information in schedule of AN care, inform her of the reasons for attending in future, and when to attend.
For information on counseling for other issues, so women can make decisions, see resources in health education and information section below.
One of the decisions that the midwife is continually assessing throughout Antenatal care, is whether all is well with the woman, the baby, and the pregnancy; or whether risks are present which means the woman should be referred to a higher level. This is an ongoing process, as the level of risk can change.
E. Health promotion/information and education.
Antenatal visits are an important time to share and discuss information which will improve the health and wellbeing of mother and fetus now, and for a healthy mother and baby after birth. At the first visit, the subject of place of birth should be discussed. The midwife is an advocate for safe birth in a health facility; but if the woman or family still insists on birth at home, the midwife must educate them regarding the importance of a skilled birth attendant and a clean delivery.
Other health promotion/information subjects to discuss include:
- Immunizations for the woman, particularly tetanus toxoid
- Other interventions such as iron, folic acid, malaria prophylaxis
- Self-care and nutrition
- Discomforts of pregnancy and offer advice for them
- Cleanliness and safe water
- Importance of breastfeeding for infant health and survival
- Ask the woman about her feelings about past pregnancy, labour and postnatal experiences
- Any other issues appropriate for that woman.

History taking history of a pregnant woman during first antenatal visit:
Content:
Taking a comprehensive history at the first antenatal visit is an important role of the midwife, there are many areas of information to find out, as per these headings:
A. Family history
- Ask regarding family history of illnesses, conditions, or congenital issues which may be relevant to this woman’s health, or to her baby: e.g. Diabetes, TB, Multiple pregnancy. Cardiac disease. Hypertension, Pre-eclampsia, Congenital defects. Partner’s health/previous paternity. Allergies, Asthma.
B. Medical history
- Ask about medical or health conditions which may affect the mother the baby or the pregnancy: e.g. Cardiac, Respiratory, Renal, Hepatitis, Thyroid, Allergies, Hypertension, Thromboembolic disease. Childhood illnesses, Epilepsy, Diabetes, Tuberculosis, Mental illness
- History of any systemic illness(es): Rule out any personal history of systemic illnesses like: High BP (Hypertension), Diabetes, Breathlessness on exertion, palpitations (Heart disease). Chronic cough, blood in sputum, prolonged fever (Tuberculosis), Renal disease. Convulsions (Epilepsy), Attacks of breathlessness or “Dama” (Asthma), Rashes, Jaundice.
C. Surgical history
- Any relevant previous surgery including anaesthetic; Spinal, hip or back deformity. Accidents, broken bones, pelvic injury.
- Any surgery on the reproductive tract (e.g. uterine surgery, cone biopsy, uterine perforation during an MR/MTP etc.).

D. Medications and drugs
- Ask if the woman is taking any prescribed medications; or any other medications or drugs including herbal. This is important to find out if the woman is allergic to any drug, or if she is taking any drug that might be harmful to the foetus.
- History of drug allergies: This is important to find out if the woman is allergic to any drug.
- Also ask the woman for any history of treatment or drugs taken for infertility. If yes, these women have a higher chance of having twins and other multiple pregnancies.
E. Menstrual and Gynaecological history
- Menstrual history, Age at menarche. Regularity of menstrual cycle, Duration of menses.
- History of her menses; for example excessive or long bleeding may be a risk for anaemia;
- Painful menses may affect the advice for post natal contraception choices.
- First day of her last period; was it a normal period; Contraception, Smear history. Vaginal
- infections, STIs, Surgery or laser treatment to cervix, cervical suturing; fistula history, or surgery to repair fistula.
- History of infertility or treatment for it.
F. History of previous pregnancies
- Ask the woman about her history of being pregnant, and how each pregnancy ended. This may be a distressing or private subject, particularly if the woman has had abortion, miscarriage, or a stillbirth; so the midwife should be kind and sensitive in her communication.
G. Ask questions about each pregnancy:
- For each pregnancy, and each loss of pregnancy or birth, ask regarding: Surgery, Complications, Transfusions, Breast feeding. Postnatal health (physical and emotional). Feelings about previous pregnancies and births.
- Any surgery on the reproductive tract (e.g. uterine surgery, cone biopsy, uterine perforation during an MR/MTP etc.)
- In particular ask for a history of high blood pressure or convulsions in previous pregnancy;
- For each birth, ask regarding prolonged labour, obstructed labour, mal-presentation like breech delivery, ante-partum haemorrhage, post-partum haemorrhage, assisted delivery (forceps or vacuum extraction), delivery by caesarean section
- Ask regarding possible isoimmunisation (Rh-ve) in previous pregnancy (ask her for the history of any costly injection given to her within 72 hours of her previous delivery).
- Ask specially for notes on last pregnancy, if available
- Identify any complications during previous pregnancies that may have a bearing on the
present pregnancy. - For each baby, ask about that child’s health and wellbeing; check for neonatal death, infant death, congenital concerns, illnesses or outcomes which you may need to provide health education regarding (e.g. jaundice, immunizations, tetanus, ORS, etc.).
H. Assess for risks:
- Assess for some of the researched risks, to help develop plan of care. For example:
- Age of the woman: women aged less than 16 or more than 40 years have greater chances of having pregnancy related complications.
- Primigravidas (women having their first baby) and those who have had 4 or more pregnancies are at higher risk of developing complications during pregnancy and during labour.
- Birth Interval: research has shown that women who have spaced their children less than 36 months apart, have greater chances of delivering a premature and low birth weight baby, with consequently increased mortality.
- An interval of less than 2 years from last pregnancy, or 3 months from the last abortion, increases the chance of the mother developing anemia.
- Having gathered a full obstetric history helps the midwife carry out a risk assessment, and is necessary to develop an appropriate plan for the remainder of the pregnancy/AN care, and for the birth.
I. History of current pregnancy
- As per the menstrual history above, ask the questions necessary to determine the LMP and so calculate the HDD, and current gestation.
- You will know from other questions her: Age, Parity, When last baby born.
- Ask about how she feels about this pregnancy (happy or reluctant).
- What signs of pregnancy she has had, if she has felt fetal movements, and if so when she first felt them;
- General wellbeing in the pregnancy so far, and if she has any symptoms during present pregnancy. Some symptoms might be causing the woman discomfort, and the midwife could offer support or advice. These include: Nausea and vomiting. Heartburn, Constipation, Increased frequency of urination.
- Some symptoms are indications of a complication arising. Ask the woman for the following symptoms in the present pregnancy: Fever, Vaginal discharge. Palpitations, easy fatigability and breathlessness at rest. Generalized swelling of the body; puffiness of face. Passing less amount of urine. Vaginal bleeding. Decreased or absent foetal movements. Leaking of watery fluid per vaginum (PV).
- Ask if the woman or family have any questions, or concerns. Advice should be offered as per various resources given.
J. Nutritional status
- Ask questions regarding: Appetite, Weight, Type of diet, Folic acid supplement.
- History of intake of habit forming or harmful substances: Ask the woman if anyone in the household smokes (risk of passive smoking) or if she takes tobacco (chewing or smoking) and/or alcohol. If yes, she needs to be counselled to discontinue them during pregnancy, as it harms the developing foetus.
- Even after the delivery, the woman should be advised to continue to abstain from taking alcohol and tobacco because it may cause other complications such as addiction and / or the development of cancer etc.

Determine fetal Well-being during Pregnancy:
The information gathered during the antenatal visits will help the midwife assess fetal wellbeing. It has some indicators including –
1. Increasing maternal weight and increasing uterine size.
2. Uterine size being equivalent to gestational age and remaining correct for gestational age.
3. Fetal movements that follow a regular pattern (once fetal movements can be felt). Fetal heart rate is within normal range of 110-160 beats per minute (bpm) when it is auscultated.
Some of this information can be gained when the midwife does an antenatal assessment including carrying out a systematic abdominal palpation.
At antenatal visits the midwife should ask the mother about fetal movements; and also educate her about normal fetal movements that can reassure her about her baby’s wellbeing. At least 10 movements a day is considered usual, but the mother should get used to her baby’s pattern of movement.
Some babies have most of their movements early in the day, some later in the day – and some all day. Mother should get used to her baby’s pattern; and if her baby’s movement pattern is reduced or changed, she should have an urgent antenatal check.
Normal fundal growth patterns:
During pregnancy the uterus is expected to grow at a predicted rate. The level of the top of the uterus the fundus is assessed during abdominal palpation, and can be measured to assess growth against the expected rate.
Especially in early pregnancy, it is possible to assess the size of the uterus and estimate gestation quite accurately; later in pregnancy what becomes more important to assess fetal wellbeing is the regular growth of the fundus since it was last checked. That is one of the reasons why it is important to have more than one antenatal visit in pregnancy.
Stages of fundal height:
- At about Three months (12-wks): The top of the uterus is usually just above the mother’s pubic bone.
- At about five months (20-22 wks): The top of the uterus is usually right at the mother’s umbilicus.
- At about eight to nine months (36-40 weeks): The top of the uterus is almost up to the bottom of xiphisternum or ribs.
As a general rule, a woman’s fundal height should be within 1 to3 Centimeters in weeks.

Measurement of fundal height:
1. The mother lie on her back with some support under her head and knees.
2. Explain to her about your procedure before you begin touching her abdomen.
3. Touch her abdomen firmly but gently.
4. Walk your fingers up the side of her abdomen until you feel the top of her pregnant uterus under the skin. It will feel like a hard ball.
5. Lay a soft plastic measuring tape on the mother’s abdomen, holding the zero on the tape at the top of the pubic bone (symphysis pubis)
6. Follow the curve of her abdomen and hold the tape at the top of her uterus.
7. Write down the number of centimeters (cm) from the tap of the public bone to the top of the uterus.
8. Fundal height should increase by 6 finger widths (two finger widths every month) in the second trimester.
9. Wash your hands.
Fandalhight is not consistent with gestation may mean:
1. Unreliable landmarks / long abdomen.
2. Inaccurate dates.
3. Fetus larger or smaller.
4. Less or more amount of amniotic fluid.
5. Multiple pregnancy.
6. Abnormal lie of the uterus. Eg. transverse lie.
7. Uterine mass or tumor.
8. Poor technique of measuring.
9. Intrautenrine fetal death.
Principles of abdominal examination
1. First see the woman as a whole person.
2. Obtain consent for abdominal examination and palpation.
3. Ensure her comfort and privacy.
4. Clean hands.
5. Avoid supine hypotension or venacaval compression, do not have woman lying flat.
A. Inspection
- Check size, shape and contours of the uterus consider in relation to gestation , presentation and position.
- Match visible scars with health history obtained.
- Observe for bruising, signs of physical violence.
B. Fundal palpation
- Identifies uppermost part of the uterus & baby.
- Indicates where to place tape measure for measuring fundus to symphysis height.
- Identify size, lie and initial info re-presentation.
C. Auscultation
- Place Pinards, Stethoscope or Doppler sonicaid over anterior shoulder to auscultate fetal heart sound.
- Identifies, whether baby is alive.,
- Allows assessment of fetal heart rate.
D. Amniotic Fluid estimation
Midwifery skill of assessing amniotic fluid (Liquor) volume whether it is Less than normal, normal, & excessive.
1. Oligohydramnios- It is reduced liquor volume. The uterus may feel small and compact and the fetal parts may be easily palpated. It may indicate growth and development restriction.
2. Polyhydramnios- It is increased liquor, The uterus may be larger than expected and the uterus may feel tense to palpate. The fetal parts may not be easily palpated
Leopold’s Maneuvers of abdominal palpation:
Leopold’s Maneuvers are difficult to perform on obese women and women who have polyhydramnios. The palpation can, sometimes be uncomfortable for the woman if care is not taken to ensure she is relaxed and adequately positioned. To help in this, the midwife should first ensure that the woman has recently emptied her bladder. The woman should be semi- recumbent, with her shoulders raised on a pillow, and her knees drawn up a little to relax the abdominal muscles.
Avoid having the woman lie flat, to prevent supine hypotension. Her abdomen should be uncovered, and most women appreciate it if the individual performing the maneuver warms their hands prior to palpation.
First maneuver:
Fundal palpation.
While facing the woman, palpate the woman’s upper abdomen with both hands. A midwife can often determine the size, consistency, shape, and mobility of the form that is felt. The fetal head is hard, firm, round, and moves independently of the tank while the buttocks feel softer, are symmetric, and the shoulders and limbs have small bony processes: unlike the head, they move with the trunk.
Second maneuver:
Umbilical or lateral palpation.
After the upper abdomen has been palpated and the form that is found there is identified as either head or breech, the individual performing the maneuver attempts to determine the location of the fetal back. Still facing the woman, the midwife palpates the abdomen with gentle but also deep pressure using the palm of the hands. First the right hand remains steady on one side of the abdomen while the left hand explores the right side of the woman’s uterus.
This is then repeated using the opposite side and hands. The fetal back will feel firm and smooth while fetal extremities (arms, legs, etc.) should feel like small irregularities and protmsions. The fetal back, once determined, should connect with the form found in the upper abdomen and also a mass in the maternal inlet, lower abdomen.
Third maneuver:
Pelvic palpation, assessing descent of fetal head.
In the third maneuver the midwife attempts to determine what fetal part is lying above the pelvic inlet, or in the lower abdomen. The individual performing the maneuver can gently grasp the lower portion of the abdomen just above the pubic svmphysis with the thumb and fingers of the right hand. This maneuver should yield the opposite information and validate the findings of the first, fundal, maneuver. If the woman enters labor, this is the part which will most likely come first in a vaginal birth.
If it is the head, it may be gently moved balloted or ‘nodded’. This Pawlick’s grip, although still used by some obstetricians, is not recommended as it is more uncomfortable for the woman. Instead, a two-handed approach is favored by placing the fingers of both hands laterally on either side of the presenting part, and assessing for the same information.
Fourth maneuver:
Deep pelvic palpation, assessing attitude of fetal head; sometimes termed Pelvic grip. The last maneuver requires that the midwife face the woman’s feet, as she will attempt to locate
the fetus’ brow. The fingers of both hands are moved gently down the sides of the uterus toward the pubis.
The side where there is resistance to the descent of the fingers toward the pubis is greatest is where the brow is located. If the head of the fetus is well-flexed, it should be on the opposite side from the fetal back. If the fetal head is extended though, the occiput is instead felt and is located on the same side as the back.
Cautions
Leopold’s maneuvers are intended to be performed gently; care must be taken not to hurt the woman; observe for her non-verbal cues if it is painful. Also, do not roughly or excessively disturb the fetus. It is important to note that all findings are not truly diagnostic.