Intrauterine contraceptive device- This book covers the entire syllabus of “Community Health Nursing” prescribed by the Universities of Bangladesh- for Basic and diploma nursing students. We tried to accommodate latest information and topics.
This book is examination friendly setup according to the teachers’ lectures and examination’s questions. At the end of the book previous university questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourished. The unique way of presentation may make your reading of the book a pleasurable experience.
Intrauterine contraceptive device
Definition of IUCD
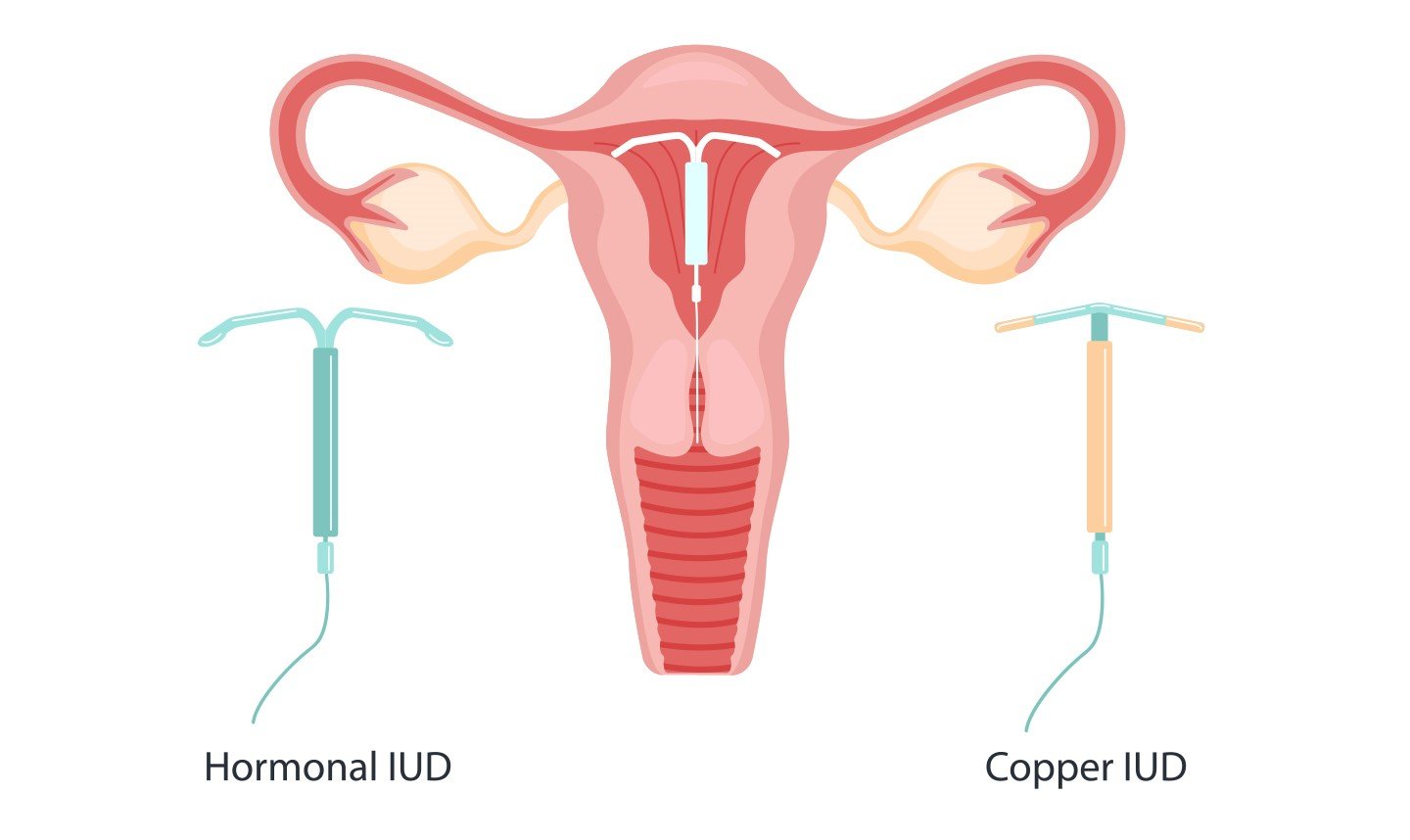
Intrauterine contraceptive device is a small plastic carrier, usually in the shape of a T or similar design on the vertical stem of which is wound some copper wire and may have copper bands on the transverse arms.
Or
An IUD is a small, T-shaped plastic device that is wrapped in copper or contains hormones. The IUD is inserted into the uterus by a doctor. A plastic string tied to the end of the IUD hangs down through the cervix into the vagina.
Mechanism of Action of IUCD
A. Foreign body inflammatory reaction on the endometrium cases:
- Increase PG secretion
- Inflammatory cells- Leucocytes and macrophages in the edometrium make a hostile environment for fertilized ovum and phagocytose the sperm and blastocyte.
- Increase tubal motility which result in quick migration of the fertilized ovum into the uterine cavity before the endometrium is receptive.
B. Cooper ion causes:
- Interferes with all the enzymatic activity of endometrium, particularly Zn containing carbonic anhydrase
Interferes with cellular DNA control - Increase inflammatory uptake by endometrium
- Toxic effect of Cu affects sperm motility, capacitating and survival by altering the biochemical composition of cervical mucus.
a. 1st generation-Lippes loop.
b. 2nd generation Cu impregnant CuT
c. 3rd generation->Hormone impregnant->Progestasent
d. Hospital supply-> Cu 1200
Definition of Copper – T
A small, “T” shaped plastic device inserted into the uterus by medical personnel to prevent pregnancy.
| A. Indication of Cu-T: |
|
| B. Contraindication of Cu-T: | a) Absolute:
b) Relative:
|
| C. Side effect: |
|
Complication of Copper-T:
1. Fainting and collapse of the patient
2. Mood changes
3. Acne
4. Headache
5. Breast tenderness
6. Nausea
7. Cramping and pain at insertion
8. Increased bleeding
9. Pelvic infection
10. Uterine perforation
11. Expulsion
12. Ectopic pregnancy

| A. Advantages of Cu – T/IUCD |
|
| B. Disadvantages of IUCD: | Not 100% effective (only 97%) 1. Increase menstrual bleeding:
2. Pregnancy- 60th intrauterine and ectopic pregnancy. 3. Pain & discomfort- low backache, lower abdominal cramp, pain in the thigh. 4. Perforation of uterus.
6. Syncopal attack. 7. Cramp like pain 8. Expulsion with risk or pregnancy. 9. Thread to infertility. 10. Infection-actinomycesisraeliae |
Best Time of Insertion
1. End of menstruation
2. 6 weeks after delivery or abortion
3. Just after MR.
4. Insertion by withdrawal method.
5. Follow up: After each mens.
Advice or Instructions for Cu-T Users
1. She should regularly check the threads or tails to be sure that the Cu-T is in the uterus, if she fails to locate the threads, she must consult the doctor.
2. She should visit the clinic whenever she experiences any side effects such as fever, pelvic pain and bleeding.
3. If she misses a period, she must consult the doctorale gele atte
4. She should be examined after her 1st menstrual period, for the chances of loop expulsion are high during this period, and again after the third menstrual period to evaluate the problems of pain and bleeding, and thereafter at six month or one year intervals depending upon the facilities and the convenience of the patient.
Selection of Patient for IUCD
A. Patient profile
- Age of the patient.
- She should have at least one child
B. History:
- History should be taken to exclude menstrual abnormality, PID, previous history of ectopic pregnancy and suspected pregaancy.
- Personal history
C. Pelvic examination:
- To determine-the size, shape position and mobility of the uterus.
- To exclude adnexal and cervical pathology
D. Investigation:
- Pregnancy test to exclude pregnancy Cervical smear may be taken if possible
E. Counseling:
It is essential to discuss the possible side effects of these preparations with each woman before administration & should be advised for follow up visits.
The threads of the IUCD sometime not palpable by the user. It may be
a. Device in uterus but
- Thread cut too short or caught up around the device
- Avulsed at a previous removal attempt
- Device itself mal-positioned or translocation inside the uterus
b. Translocation into the abdomen (by perforation of uterus) –
- In the broad ligament
- Peritoneal cavity
c. Expulsion

Diagnosis of the missing/displacement of IUCD
A. Examination:
- Abdominal palpation
- Speculum examination
- Introduction of uterine sound inside the uterus
B. Investigation:
- X-ray pelvis A/P and straight lateral view
- Ultrasonography
- Hysterosalphingography
- Hysteroscopy
- Laparoscopy
C. Management:
a) When IUCD is inside the uterus –
- Remove the IUCD by thread retrievers of by D & C
b) When IUCD is outside the uterus remove the IUCD by –
- Laparotomy
- Laparoscopy
See More: