Some communicable diseases – This book covers the entire syllabus of ” Community Health Nursing” prescribed by the Universities of Bangladesh- for Basic and diploma nursing students. We tried to accommodate the latest information and topics.
This book is an examination-friendly setup according to the teachers’ lectures and examination questions. At the end of the book previous university questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourish. The unique way of presentation may make your reading of the book a pleasurable experience.
Some communicable diseases
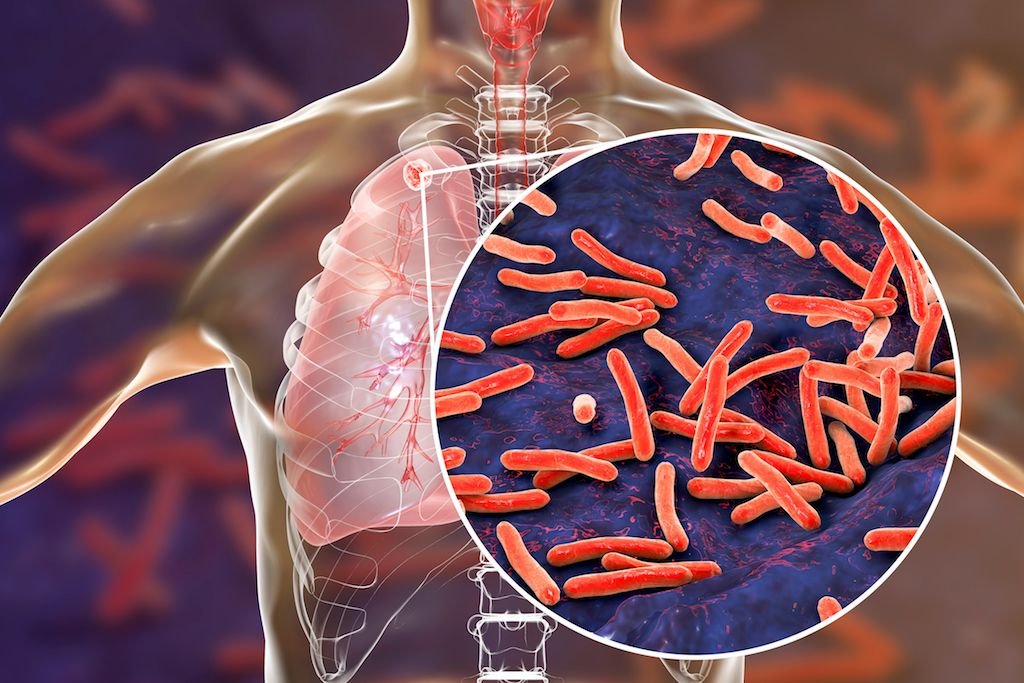
Pulmonary tuberculosis:
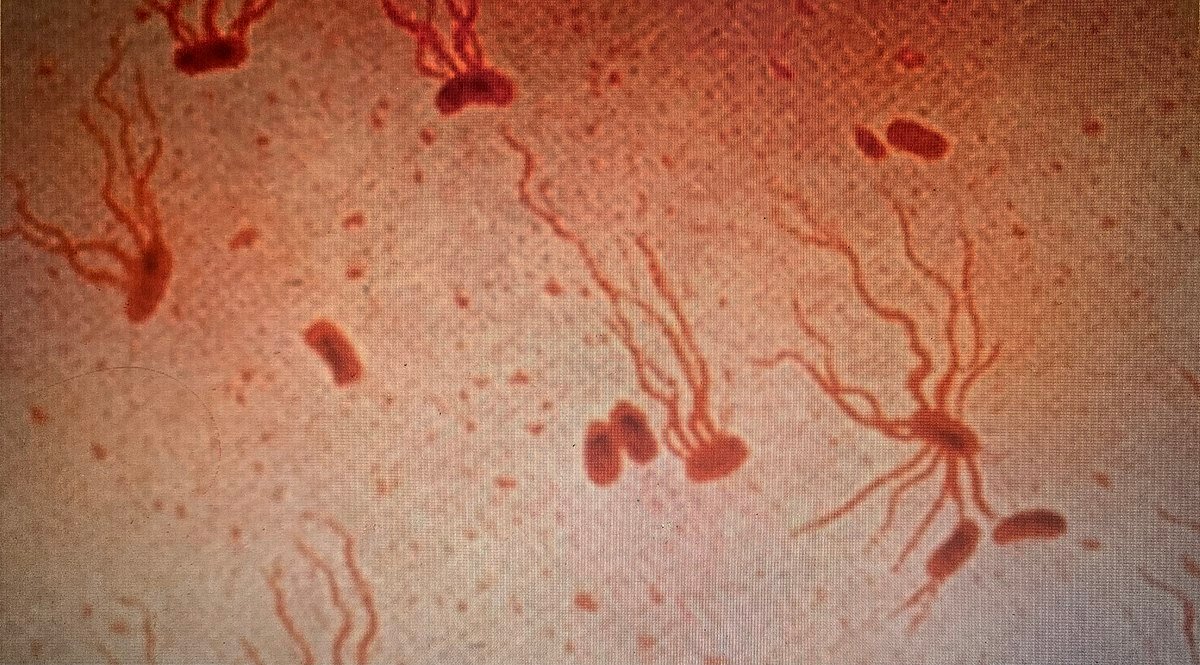
The bacterium Mycobacterium tuberculosis causes tuberculosis (TB), a contagious, airborne infection that destroys body tissue. Pulmonary TB occurs when M. tuberculosis primarily attacks the lungs. However, it can spread from there to other organs. Pulmonary TB is curable with an early diagnosis and antibiotic treatment.
Or,
Pulmonary TB is caused by the bacterium Mycobacterium tuberculosis (M tuberculosis). This means the bacteria is easily spread from an infected person to someone else.
(Ref: K Park 26 /204)
Pulmonary TB can be spread by
- shaking hands
- sharing food or drink
- sleeping in the same bed
- kissing
TB is airborne, which means someone can become infected with M. tuberculosis after breathing air exhaled by someone with tuberculosis. This can be air from:
- coughing
- sneezing
- laughing
- singing
The germs can stay in the air for several hours. It’s possible to inhale them even when the infected person isn’t in the room. But usually you have to be close to someone with TB for a long period of time to catch it.
Pulmonary TB can be diagnosed by:
- conduct a physical exam to check for fluid in your lungs
- ask about your medical history
- schedule a chest X-ray
- order a medical test to confirm pulmonary TB
To diagnose pulmonary TB specifically, a doctor will ask a person to perform a strong cough and produce sputum up to three separate times. The doctor will send the samples to a laboratory. At the lab, a technician will examine the sputum under a microscope to identify TB bacteria.
Risk factors for pulmonary TB:
The risk for getting pulmonary TB is highest for people who are in close contact with those who have TB. This includes being around family or friends with TB or working in places such as the following that often house people with TB:
- correctional facilities
- group homes
- nursing homes
- hospitals
- shelters
People also at risk for developing pulmonary TB disease are:
- older adults
- small children
- people who smoke
- people with an autoimmune disorder, such as lupus or rheumatoid arthritis people with lifelong conditions, such as diabetes or kidney disease
- people who inject drugs
- People who are immunocompromised, such as those living with HIV, undergoing chemotherapy, or taking chronic steroids.
[Ref: K. Park26th/210-12]
Sign and symptoms of pulmonary tuberculosis
Symptoms
a) Systemic effects: Anorexia, Weight loss, Lassitude, Sleep sweat, evening pyrexia.
b) Local effects:-
1. Lungs: Persistent cough, Sputum, Haemoptysis,
2. Pleura: Pleural pain, Pleural effusion, breathlessness
3. Pericardium/ heart: Pain, arrhythmias, constrictive pericarditis, cardiac failure.
4. Intestine: Diarrhea, Mal-absorption, obstruction
5. GIT: Renal failure, Hematuria, epididimis, salpingitis, erythema nodosum.
6. Skin: Lupus valgaris, iritis, phlyctennular kerato conjunctivitis.
7. Bones/joints: Osteomyelitis, arthritis
8. Lymphatic’s: cold abscesses, lymph adenopathy, sinuses.
Signs:
1. Early signs: Crepitations usually heard at one or other lung apex posteriorly.
2. Sign of consolidation, cavitations, fibrosis, pleural effusion, and spontaneous pneumothorax may be present.
[Ref: K. Park26th/210-12]
Treatment of pulmonary TB:
1. Rest-not required unless patient is very ill.
2. Diet normal
3. Isolation not required only very young children should be kept away from the patient
4. Anti TB drugs are the mainstay of therapy
Chemotherapy in the main treatment of T. Drugs that are used in TB –
A) Six month regimen
Initial phase: 2 month (four drugs): Patient will come daily to take the drugs (DOTS)
| Children | Adults | ||
| < 50kg | > 50kg | ||
| Rifampicin | 10 – 20mg / k * g | 450 mg | 600 mg |
| Isoniazid | 10 mg/kg | 225 mg | 300 mg |
| pyrazinamide | 20 – 35mg / k * g | 1200 mg | 1600 mg |
| Ethambutol | 25 mg/kg | 825 mg | 1100 mg |
Continuation phase 4 month: Patient will be given drugs for 30 days each visit. Thrice daily
| Children | Adults | ||
| <50 kg | > 50kg | ||
| Rifampicin | 10 – 20mg / k * g | 450 mg | 600 mg |
| Isoniazid | 10 mg/kg | 225 | 300 mg |
B) Nine month regimen:
Initial phase 2month (3 drugs): Patient will come daily to take the drugs (DOTS).
| Children | Adults | ||
| <50 kg | >50 kg | ||
| Rifampicin | 10 – 20mg / k * g | 450 mg | 600 mg |
| Isoniazid | 10 mg/kg | 225 mg | 300 mg |
| pyrazinamide or | 20 – 35mg / k * g | 1200 mg | 1600 mg |
Ethambutol or Steptomycin | 25 mg/kg | 825 mg | 1100 mg |
| 30 mg/kg | 750 mg | 1000 mg |
Continuation phage 7 month: Patient comes each alternative day to take the drugs (DOTs)
| Children | Adults | ||
| <50 kg | >50 kg | ||
| Rifampicin | 10-20 mg/kg | 450 mg | 600 mg |
| Isoniazid | 10 mg/kg | 225 | 300 mg |
[Ref: K. Park/26/214]
Name of anti-tubercular drugs with dose:
| Children | Adults | ||
| <50 kg | >50 kg | ||
| Rifampicin | 10-20 mg/kg | 450 mg | 600 mg |
| Isoniazid | 10 mg/kg | 225 mg | 300 mg |
| pyrazinamide or | 20-35 mg/kg | 1200 mg | 1600 mg |
Ethambutol or Steptomycin | 25 mg/kg | 825 mg | 1000 mg |
| 30 mg/kg | 750 mg | 1000 mg | |
Main complication of anti-tubercular drugs:
➤ Isoniazid
✓main complication: Peripheral neuropathy, Hepatitis, Rash
➤ Rifampicin
✓ main complication: Febrile reaction, Hepatitis, Rash, Gastrointestinal disturbance
➤ Pyrazinamide
✓ main complication: Hepatitis, Gastrointestinal disturbance, Hyperuricaemia
➤ Streptomycin
✓main complication: 8th nerve damage, Rash
➤ Ethambutol
✓ main complication: Retro bulbar neuritis, Arthralgia
[Ref: K. Park/26/216-17]
Investigate pulmonary tuberculosis (TB)
Investigation:
- Chest X-ray P/A view
- CBC (complete blood count) TC, DC, ESR, Hb%
- Sputum for AFB staining and C/S
- Tuberculin test (Mantoux test)
- Lymph node biopsy-mandatory for absolute diagnosis
- Pleural biopsy
- Others
-If pleural effusion – Pleural fluid study
-Closed case – Bronchial brushing
-PCR-highly sensitive and specific
Tuberculin test or Mantoux test
Definition of Tuberculin test/Mantoux test:
It is a screening of tuberculosis (TB) which can help in diagnosis of tuberculosis (TB) with other test
Purpose:
-To measure prevalence of infection
-Aid to diagnosis of suspected infection (not confirm diagnosis)
-For contact tracing of infectious cases. Indication of early clinical infection.
-Post vaccination check for the efficacy of BCG vaccination.
✓ Reagents
-PPD (Purified Protein Derivatives) -10 UT (Tuberculin unit) in 0.1 ml normal saline.
✓ Procedure
-10 TU of PPD contained in 0.1 ml is administered intra-dermal in the flexor surface of the forearm. After 72 hours the result is observed.
✓ Result
-Positive: An area of indurations > 10mm
-Negative: No indurations
✓ Interpretation
a) Positive test
✓ Causes
-Past infection or disease (TB)
-Present infection or disease (TB)
-BCG vaccination
b) False positive: It means skin test is positive, but the patient has no TB.
✓ Causes
-Infection by atypical mycobacterium
c) False negative: It means skin test negative but the patient has TB.
✓ causes
-Overwhelming TB
-Miliary TB
-Measles
-sarcoidosis
-Scarlet fever
-Brucellosis
-Hodgkin’s disease
-Leprosy
-Malnutrition
-Administration of immunosuppressive drugs
-Other immunosuppressive disease
✓ Importance of tuberculin test
-It become positive in active infection, past infection of TB and post BCG vaccination cases.
-It gives a clue in diagnosis of extra pulmonary TB.
-It has and impotent role in diagnosis of active TB among children below 5 years are not vaccinated before. (As adult is exposed).
[Ref: K. Park/26/212]
Factors increasing the risk of Tuberculosis
Patient related
- Age (Children >young adult<elder)
- First generation immigrants from high Prevalence countries
- Close contacts of patients with smear positive pulmonary TB
- Overcrowding (Prisons, collective dormitories): Homelessness (doss houses and hostels)
- Chest radiographic evidence of self-healed tuberculosis
- Primary infection < 1 year previously
- Smoking: cigarettes, and bidis
Associate disease:
- Type on diabetes mellitus (DM)
- Malignancy (especially, leukemia, Lymphoma)
- Immune-suppression: HIV, high dose corticosteroids, cytotoxic agents.
- Chronic renal failure
- Silicosis.
Prevent and controlled pulmonary TB.
A. Curative methods (early diagnosis and treatment): It consist of-
- Case finding/screening/early detection of cases by-
-Sputum examination: (a) Staining, (b) culture
-Chest X-ray
-Tuberculin test
- Isolation
- Chemotherapy (drug treatment) to suitable case
B. Preventive methods:
- BCG vaccination
- Chemoprophylaxis
- General health improvement:
-Adequate housing
-Good nutrition
-Health education
- Limitation of disability
- Rehabilitation
- Surveillance
[Ref: K. Park/26/230]
National TB control programme in BD (NTP):
Goal:
To reduce the incidence of TB until it is no longer a public health problem, by diagnosing and treating effectively as many TB patients as possible, especially those whose sputum is smear positive (infectious cases).
Objective of TB control:
1. To increase-the cure rate of sputum positive TB from 50% to 85% by the year 2005.
2. To increase the case detection from teh present 20% to over 70% of teh estimated incidence. by the year 2005.
Strategies of control therapy:
1. Ensure effective chemotherapy to all patients.
2. Promote early detecion of sputum positive TB
3. Organize treatment delivery up to union level.
4. Introduce standardized recording and reporting system.
5. Monitor results of treatment & evaluate progress of the programme by the means of quarterly cohort analysis.
6. Provide regular training & refresher courses for all staff involved.
7. Strengthening co-operation between Government and NGO involve in TB control.
8. Co-ordinate TB control activities with I. leprosy control activities integrating the to PHC through out the country.
Structure of the programme:
Central level: Honorable minister of the ministry of health and family welfare.
↓
DG health
↓
Project Director of Mycobacterial disease control programme.
↓
Divisional level: Divisional consultant
↓
District level: Civil surgeon
↓
Thana’ level: Thana health and family planning officer
↓
Medical officer designated for TB & leprosy
Dots strategy: 5 components
1. Government Commitment
2. Case Detection
3. Short-Course Chemotherapy
4. Supply System
5. Recording and Reporting.
a) Chemotherapy (drug treatment) to suitable case:
| TB Diagnosis Category | TB Patients | TB Treatment Regimen | |
| Initial phase (daily) | Continuation phase ( times weekly) | ||
| i. | New smear – positive patients New smear-negative PTB with extensive parenchyma in evolvement | 2 (HRZE) | 4 (HR) 3 |
| ii. | Previously treatment sputum smear positive PTB.
| 2 (HRZE)S 1 (HRZE) | 5 (HR) 3 E3 |
| iii. | New smear-negative PTB (other than in Category1): Less severe forms of EPTB | 2( HRZ) | 4 (HR) 3 |
HREZ:
H = INH
R = Rifampicin
E = Ethambutol
Z = Pyrazinamide
2 HRZE= The duration of the phase is 2 months
In category-II, initial phase in 3 months (2+1) a continuation phase is 5 months.
BCG vaccine to all new born babies.
[Ref: K. Park/26/214-218]
Multidrug-resistant:
Multi-drug-resistant tuberculosis (MDR-TB) is a form of tuberculosis (TB) infection caused by bacteria that are resistant to treatment with at least two of the most powerful first-line anti-TB medications (drugs), isoniazid and rifampin. Some forms of TB are also resistant to second-line medications, and are called extensively drug-resistant TB.
Or,
Multi-drug resistant TB (MDR-TB) is TB that is resistant to the typical antibiotics used to treat the condition, which are isoniazid and rifampin. Some of the factors that contribute to MDR-TB include:
- healthcare providers prescribing an incorrect drug to treat TB
- people stopping treatment early
- people taking poor-quality medications
Improper prescribing is the leading cause of MDR-TB, according to WHO, However, it’s possible a person who hasn’t ever taken TB medications can have a strain that is drug-resistant. People who develop MDR-TB also have fewer options for treatment. The second-line treatments can be expensive and take as long as two years. It’s also possible for MDR-TB to develop even further into extensively drug-resistant TB (XDR-TB).
Outlook for pulmonary TB:
Pulmonary TB is curable with treatment, but if left untreated or not fully treated, the disease often causes life-threatening concerns. Untreated pulmonary TB disease can lead to long-term damage to these parts of the body:
- lungs
- brain
- liver
- heart
- spine
New drugs and treatments are currently being developed to prevent latent TB and TB, especially as MDR-TB grows. In some countries, this involves a vaccine called Bacillus Calmette-Guérin (BCG). This vaccine is useful to prevent severe forms of TB outside the lungs in children, but it doesn’t prevent development of pulmonary TB.
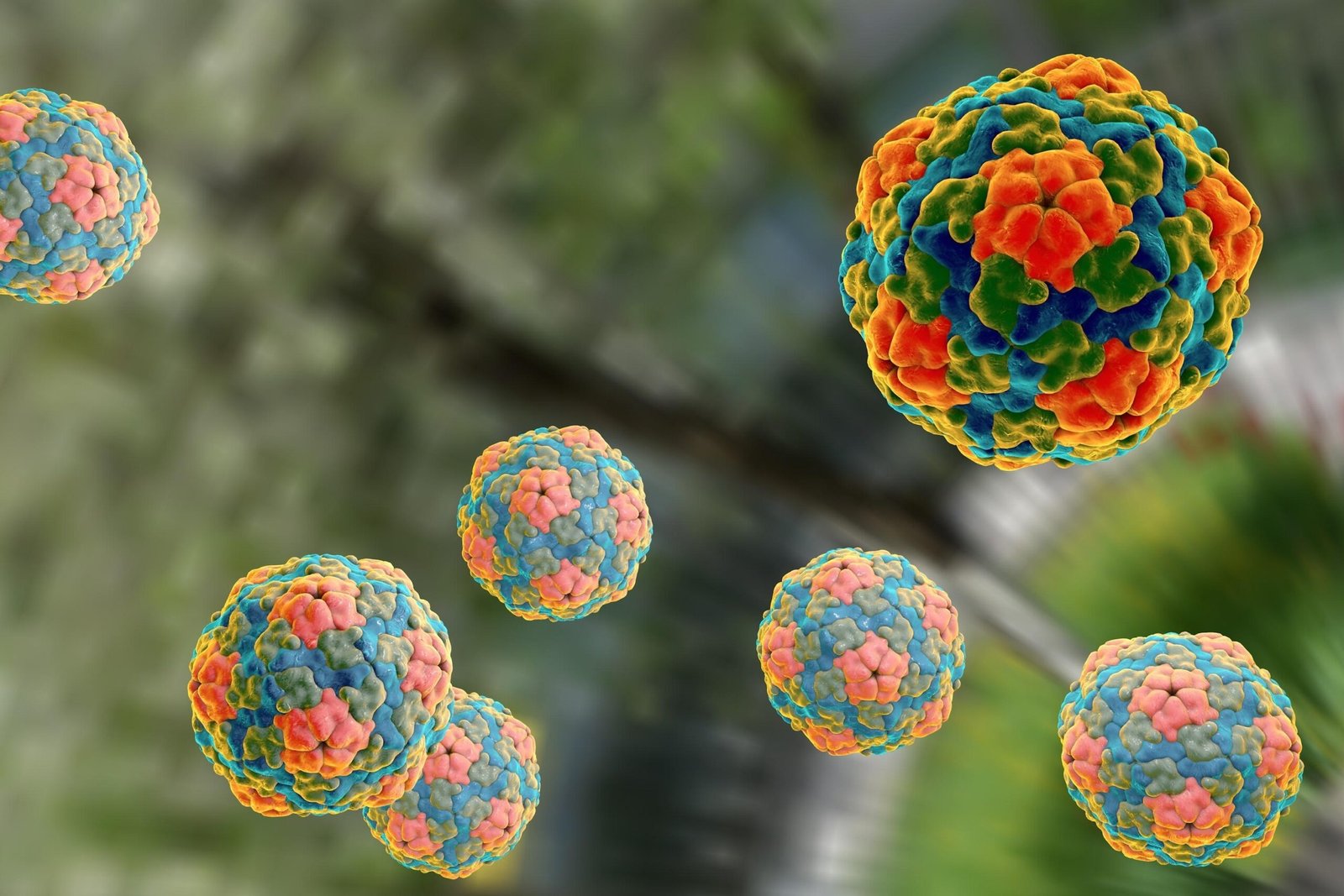
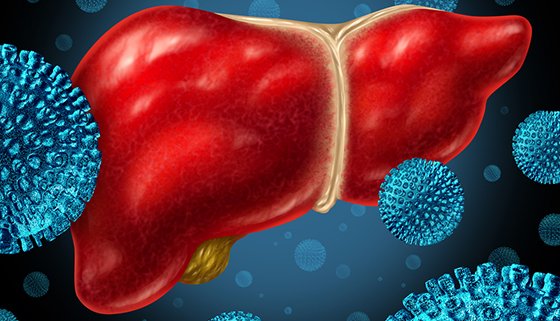
Viral hepatitis
Definition of Meningitis:
According to World Health Organization (WHO):
Hepatitis is an inflammation of the liver. The condition can be self-limiting or can progress to fibrosis (scarring), cirrhosis or liver cancer.
Or,
Inflammation of the liver which result in damage to hepatocytes with a subsequent cell death.
[Ref by-K. Park/26/244]
Types of viral hepatitis
Classification of Hepatitis:
A. According to duration:
a) Acutehepatitis
b) Chronichepatitis
B. According toetiology:
a) Viral infection:
- Hepatitis A virus (HAB)
- Hepatitis B virus (HBV)
- Hepatitis C virus (HCV)
- Hepatitis D virus (HDV)
- Hepatitis E virus (HEV)
- Herpes simplex virus (HDV)
- Cytomegalovirus (CMV)
- Epstein Barr virus(EBV)
- Yellow fever virus
b) Auto immune disorder: toxins alcohol drug
c) Miscellaneous: Wilson’s disease
[Ref by-K. Park/26/2441]
Preventive and Controlling Measures of HAV and HEV:
1. Proper sanitation:
- Improving water supply
- Proper excreta disposal
- Maintenance of hygiene (personal and environmental)
- Sanitary improvements of food stores and kitchen
2. Health education about:
- Use of safe drinking water and sanitary latrine
- Proper disposal of excreta
- Food handlers should be educated in matters of food hygiene
- Adequate breast feeding and improved weaning practices
3. Fly control: Controlling breeding of flies in association with faeces and dirty water.
4. Timely control of epidemics: By strengthening of epidemiological surveillance systems.
5. Vaccination: Vaccine for hepatitis A is available but not for hepatitis
6. Screening of blood donors for hepatitis A
Preventive and Controlling Measures of Hepatitis B, C, D:
1. Avoid risk factors:
- Shared needles
- Homosexuality and illiegimate heterosexuality
- Prostitute
- Professional blood donors
- Carriers: They should not share razors and tooth brushes, Use barrier methods of contraception and should not donate blood
2. Screening of blood donors and encouraging voluntary blood donation
3. Standard safety precautions in hospitals and other health care settings: To avoid accidental needle puncture and contact with infected body fluids.
4. Active immunization: HBV vaccine
5. Passive immunization: By hepatitis immunoglobulin for immediate protection to acutely exposed HBs Ag positive blood, preferably within 6hours
- Surgeons, nurses and laboratory workers
- Newborn infants of carrier mothers
- Sexual contacts of acute hepatitis B patients
6. Passive active immunization.
Hepatitis A and E
Definition of Hepatitis A:
Hepatitis E is an acute infectious disease caused by hepatitis HAV.
A) Agent’s factors:
- Agent: Causative agent is hepatitis A virus
- Resistance: The virus is resistance to heat and chemical
- Reservoir of infection: Human cases only
- Period of infectivity: 2 weeks before and I week after the onset of jaundice.
- Infective materials: Human faeces, Blood, Serum and body fluids.
B) Host factors:
- Age: All age groups can be affected. More frequent among children than adult.
- Sex: Both sexes can be equally affected
C) Mode of transmission:
- Faeco oral route
- Parenteral route (through blood or contaminated by needle
- Sexual route
D) Incubation period: 2-6weeks
E) Sign and symptoms: Symptoms may be mild or even no symptoms, but the person faeces are still infectious to others. The usual features are:
- A short, mild, flu-like illness: Fever, chills, malaise and fatigue
- Nausea, vomiting and diarrhea
- Loss of appetite
- Weight loss
- Dark urine and jaundice
- Itchy skin
- Abdominal pain
F) Investigation:
- Anti HAV
- Serum bilirubin
- SGPT andSGOT
G) Treatment: There is no specific treatment for HAV. The disease is self-limiting and returns to normal within a couple of months. Only severely affected patients need hospitalization. General plan of treatment are-
- Bedrest
- Diet
-Protein restricted and no spicy foods
-Light diet supplemented by fruits, plenty of fluids, ORS, dab water and glucose drinks.
- If severe vomiting: IV fluid and anti-emetic
- Drugs: Sedatives, hypnotics, and diuretics, are usually avoided. It diuretics are to be used potassium sparing diuretics should be used
- Clinical and biochemical follow up
[Ref by-K. Park/26/244]
short note on – Hepatitis E.
Definition: Hepatitis E is the viral hepatitis caused by hepatitis E virus
Answer:
Epidemiology: Hepatitis E should be suspected in outbreaks of waterborne hepatitis occurring in developing countries like Bangladesh, especially if the disease is more severe in pregnant women.
Incidence and risk factors: Symptomatic HEV infections is most common in young adults
Incubation period: 3-8 weeks
Mode of transmission: Facco oral and water borne
Signs and symptoms: May be asymptomatic or mild illness without jaundice that goes undiagnosed, particularly in children, typical sign and symptoms are –
-Jaundice
-Loss of appetite
-An enlarged, tender liver
-Abdominal pain and tenderness
-Nausea and vomiting
-Fever
Investigation:
-Anti HAV
-Serum bilirubin
-SGPT and SGOT
Treatment: There is no specific treatment for HAV. The disease is self-limiting and returns to normal within a couple of months. Only severely affected patients need hospitalization. General
plan of treatment are –
- Bedrest
- Diet
-Protein restricted and no spicy foods
-Light diet supplemented by fruits, plenty of fluids, ORS, dab water and glucose drinks.
- If severe vomiting: IV fluid and anti-emetic.
- Drugs: Sedatives, hypnotics, and diuretics, are usually avoided. It diuretics are be used potassium sparing diuretics should be used.
- to Clinical and biochemical follow up.
[Ref by-K. Park/26/255]
Preventive and controlling measures of HAV and HEV:
A. Proper sanitation:
- Improving water supply
- Proper excreta disposal
- Maintenance of hygiene (personal and environmental)
- Sanitary improvements of food stores and kitchen
B. Health education about:
- Use of safe drinking water and sanitary latrine
- Proper disposal of excreta
- Food handlers should be educated in matters of food hygiene
- Adequate breast feeding and improved weaning practices
C. Fly control: Controlling breeding of flies in association with faeces and dirty water.
D . Timely control of epidemics: By strengthening of epidemiological surveillance systems.
E. Vaccination: Vaccine for hepatitis A is available but not for hepatitis
F. Screening of blood donors for hepatitis.
[Ref by-K. Park/26/255]
Hepatitis B
Mode of Transmission of Hepatitis B Virus:
A. Parenteral transmission:
a) Infected unscreened blood and blood products.
b) Tattoos/acupuncture needles
e) A mode of spread most common among parenteral drug miss-users who share needles or other injecting paraphernalia.
d) Contaminated syringes and surgical instruments
B. Sexual route:
a) Close personal contact seems necessary for transmission
b) Sexual intercourse especially in male homo sexual and heterosexuals is an important route of transmission of infection.
C. Perinatal or Vertical transmission:
a) Before birth has not been documented
b) During birth has not been documented.
c) During birth, most of the transmission occur, when placenta is separated, leakage of blood infect the baby. d) Infection occur After birth, during HBV contaminated with breastmilk
D. Close living quarters or playground play as a toddler.
[Ref by-K. Park/26/246]
Clinical features:
A. Symptoms:
- Headache
- Myalgia
- Arthralgia
- Yellow coloration of eye and skin
- Dark urine and pale stool
- Nausea and anorexia
- Vomiting
- Diarrhea
- Abdominal discomfort
- Fever
B. Signs:
- Jaundice
- Enlarged tender liver
- Occasionally, mild splenomegaly and cervical lymphadenopathy are seen.
C. Investigation:
- Blood examination’s, DC, Hb%, ESR
- Liver function test: Serum bilirubin, Serum AST and ALT – raised, PT, Serum alkaline phosphatase level
- Viral markers:
-Ig Manti HAV (hepatitis A virus)
-HBs Ag (Hepatitis B surface antigen)
-Ig M – Anti HBc (Hepatitis B core antigen)
D. Management:
a) Acute hepatitis B: There is no specific treatment only severely affected patients required hospitalization so that developing fulminate hepatic failure can be detected early.
- Bed rest (3 to 5weeks)
- Diet: Normal diet with slight fat restriction)
-Nutritious diet containing 2000-3000 K Cal/d, good protein.
-If not tolerated light diet supplemented by fruit drink and glucose
-If severe vomiting give IV fluid and glucose
- Drug (Sedative, Hypnotic): Should be avoided especially in severe hepatitis.
- Clinical biochemical and imaging follow-up.
- Treatment of complication
b) Chronic hepatitis B: Treatments are still limited, with no drug able to eradicate hepatitis B infection completely. Supportive treatment plus
- Drugs
-Interferon -alpha.
-lamivudin, 100mg/dayorally
-Adefovir.
-Entecavir (more effective than lamivudin)
-Telbivudin.
-Tenofovir, 300mg/day.
- Liver transplantation with prophylactic lamivudine and hepatitis Immunoglobulin’s
[Ref by-K. Park/26/246-47]
Fate or Complication of Hepatitis B Virus Infection:
- Full recovery in 90-95% of adults/resolution(fate)
- Acute hepaticfailure.
- Relapsing hepatitis: Biochemical, Clinical
- Cholestatic hepatitis.
- Post hepatitis syndrome
- Hyperbilirubinemia.
- Aplasticanaemia
- connective tissuedisease
- Renal failure
- Henoch schonleinpurpura
- Papularacro dermatitis
- Chronichepatitis
- Cirrhosis (hepatitis B,C)
- Hepatocellular carcinoma.
[Ref by-K. Park/26/246-471]
Preventive and Controlling Measures of Hepatitis B:
A. Avoid risk factors
- Shared needles
- Homosexuality
- Prostitute
- Professional blood donors
- Carriers: They should not share razors and tooth brushes, Use barrier methods of contraception and should not donate blood
B. Screening of blood donors and encouraging voluntary blood donation
C. Standard safety precautions in hospitals and other health care settings: To avid accidental needle puncture and contact with infected body fluids.
D. Active immunization: HBVvaccine
E. Passive immunization: By hepatitis immunoglobulin for immediate protection to acutely exposed HBs Ag positive blood, preferably within 6hours
- Surgeons, nurses and laboratory workers
- Newborn infants of carrier mothers
- Sexual contacts of acute hepatitis B Patients
[Ref by-K. Park/26/246-47]
Tetanus
Definition of Tetanus:
Tetanus is a wound infection caused by Cl. tetani. Occurring usually in the deep, contused, soil contaminated injuries with pyogenic organism it containing foreign bodies.
Or,
Tetanus is wound, caused by exotoxin of clostridium tetani. Characterized by painful paroxysmal spasm of voluntary muscle and muscular rigidity.

A. Incubation period: 6-10 days
B. Agent factores:
- Agent: Clostridium tetani is a Gram positive, spore bearing and anaerobic bacteria.
- Reservoir of infection: Soil and dust, intestine of herbivorous animals (eg.cattle, goats, shipetc)
C. Patient factors:
- Occupation: Agricultural workers mostly affected
- Immunity: No age is immune unless protected by immunization
[Ref by-K. Park/26/353]
Route of Entry:
The organism gains access to the body via various wounds, including –
- Apparently trivial injuries (eg. Puncture wounds, including those caused by splinters and rose thorns)
- Animalbites
- Humanbites
- Openfractures
- Burns
- Gangrene
- Frostbite
- Chronic decubitusulcers
- Abscesses
- Parenteral drug abuse as a complication of intramuscular injection, especially ofquinine. In neonates, especially the infants of non-immune mothers, infection can occur via infected umbilical stumps. The risk is increased by unhygienic midwifery practices, such as applying animal dung to the umbilical stump.
[Ref by-K. Park/26/353-55]
Pathogenesis of Tetanus
Tetanospasmin
↓———————————————————-↓
CNS PNS
↓ ↓
Spinal cord (motor nuclei) Motor end plate
↓ ↓
Dysfunction of polysynaptic reflex neuromuscular transmission
↓ ↓
Spasm Spasticity
Clinical Features (C/F) of Tetanus:
A. Prodromalstage:
- Dysphagia
- Severe neck pain, back pain and pain inabdomen
- Wound pain
B. Stage of tonicrigidity:
- Trismus/lockjaw:
-Spasm of massetermuscle
-Earliestsign
- Musclespasticity
- Risussardonicus: Contraction of the muscles of angle of mouth and frontalis
- Opisthotonos: Spasm of muscle of back and limbs
C. Stage of clonicspasm:
- Laryngeal and pharyngeal spasm
-Respiratory fixation
[Ref by-K. Park/26/353-55]
Differential Diagnosis:
- Tetany-Characteristically affects the limbs producing carpopendal spasm.
- Strychnine poisoning – Flaccidity between convulsions whereas in tetanus spasm persists.
- Meningitis – Neck stiffness
- Epilepsy, Hysteria
- Masseter muscle spasm due to dental abscess or throat infection.
- Dystonic reaction to phenothiazines
- Rabies
Essential of diagnosis:
- Unimmunized or partially immunized patient
- History of tetanus prone injury
- Stiffness of muscle of mastication, facial expression, neck, respiration, abdominal and back.
- Tonic muscle spasm.
Management of Tetanus:
1. Isolation of patient in a quite (No. light, No sound) darkroom.
2. O2 inhalation, tracheostomy, if necessary
3. Maintenance of food and nutrition by NG tube or IV fluid.
4. Control of muscle spasm by-
- Injection Diazepam 0.1-02 mg/kg IM or IV 6hourly
- If failed, Injection Tubocurarine.
5. Neutralization of toxin by-
- Injection Tetanus immunoglobulin (TIG) 3000-6000 units IM single dose or
- Injection Tetanusantitoxin (ATS)50000-1lackunits IMafterskinsensitivitytest.
6. Anti-microbial therapy to eradicate vegetative tetani:
- Injection Benzyl penicillin 600 mg 6 hourly IV 10hourly
7. Local care of wound:
- Closed wound should be opened up
- Wash with fresh water H2 O2solution
- Debridement of all dead tissues
8. Nursing care-
- Clear the airway by adjusting the position of head extension.
- Physical examination by auscultation of breath sounds heard (there Ronchi) every 2-4hours.
- Clean the mouth and respiratory tract of mucus with a secret and do section.
- Oxygenation according to physician instructions.
- Observation of vital signs every 2hours.
- Observation of the onset of respiratory failure /apnea. Collaboration in a secret-thinning medication
[Ref by-K. Park/26/354-356]
Prevention of Tetanus:
Women of reproductive age (15-45 years)
| TT doses | Minimum interval between doses | Years protected |
| TT – 1 | 0 | 0 |
| TT – 2 | 4 weeks after TT – 1 | 3 years (from 15 days after the administration of TT – 2 ) |
| TT – 3 | 6 month after TT – 2 | 5 years (from 15 days after the administration of TT – 3 ) |
| TT – 4 | 1 years after TT – 3 | 10 years (from 15 days after the administration of TT-4) |
| TT – 5 | 1 years after TT-4 | lifelong protected |
Antenatal: Pregnant mother should be immunized with 2 doses of tetanus toxoid within 16-28 weeks of pregnancy.
Postnatal:
- Vaccine DPT at 6 ^ (th) 10 ^ (fh) * and 14th weeks of birth.
- Booster dose: After 1 year
Tetanus prophylaxis in an injured patient: It depends on immunization status of wound, eg.
A) Clean wound:
a) Without previous immunization –
- 1″dose Inj. TT 5 cc IM stat
- 2nddose 6-12 weeks later
- 3dose after 6-12months
- And booster dose every 5 years interval
b) Previously immunized but no booster dose within 5 years-
- Inj. TT 5 cc IM stat single dose
B) Tetanus prone wounds/Dirty wound:
a) Non-immunized
- Passive immunization with: Inj. TIG 250-unit IMstat
- Active immunization with: Inj. TT 5 cc IM state and repeat at 1, 2, 6month
b) Immunized:
- Inj. TIG 250-unit IM stat
[Ref by-K. Park/26/354-356]
Complication of tetanus:
1. Aspiration pneumonia
2. Atelectasis
3. Cyanosis
4. Asphyxia due to spasm of respiratory muscle and laryngospasm
5. Tongue bite
6. Intramuscular hematoma
7. Vertebral fracture
8. Peripheral neuropathy
9. Hyperhydrosis, cardiac arrhythmia
10. Dehydration and PEM in prolonged case.
[Ref by-h. Park/26/354-356]
Chicken pox and small pox

Definition of chickenpox:
Chickenpox or varicella is an acute, highly infectious disease caused by varicella-zoster virus. It is characterized by vesicular rash that may be accompanied by fever and malaise.
Or,
It is highly communicable and infectious disease caused by varicella virus, characterized by mild prodromal symptoms and a typical rash which passes through the stages of macule, papule, vesicle and crustation.
Epidemiological features of chickenpox:
i. Agent factors:
- Agent: Varicella zoster virus
- Source of infection:
-Oropharyngeal secretion
-Lesions of skin and mucosa and
-Rarely A patient with herpes zoster
- Infectivity: 1-2 days before appearance of rash and 4-5 days thereafter
- Secondary attack rate: The disease is highly contagious, so secondary attack rate in household contacts approximately 90%
ii. Host factors:
- Age: Primarily among children under 10 years. Few may escape until adulthood
- Immunity: One attack gives life ling immunity
-Pregnancy: Presents a risk for the foetus and the neonate
iii. Environmental factors: Overcrowding favors its transmission
iv. Transmission: Person to person by droplet infection and by droplet nuclei. Vertical transmission is possible and can infect the foetus.
V. Incubation period: Usually 14 to 16 days. The range may vary from 7 to 21 days.
[Ref by-K. Park/26/158]
Clinical features and controlling measures of chickenpox
Clinical features:
a) Pre-eruptive stage: Onset is sudden with mild to moderate fever, pain in the back, malaise. This stage is very brief in children. In adults these prodromal illnesses may be prominent lasting 2-3days.
b) Eruptive stage: In children the rash is often the first sign –
- Distribution is symmetrical. First appears on the trunk where it is abundant and then gradually spreads in the centripetal manner.
- Rapid evolution: the rash advances quickly through the stages of macule, papule, vesicle and scab.
- Pleomorphism: All stages of the rash appear simultaneously
- Fever: In children, low grade fever may be observed
Treatment and controlling measure:
- There is no specific treatment for chickenpox
- Aspiration should be avoided, especially in children. Paracetamol is usually sufficient.
- Notification and isolation of cases for about 6 days after onset of rash
- Disinfection of articles soiled by nose and throat discharges
[Ref by-K. Park/26/158]
Complication of chickenpox:
-Hemorrhage
-Pneumonia
-Encephalitis
-Acute cerebral ataxia
-Reyes syndrome
-congenital defect and malformation (low birth weight, atrophied limbs, microcephaly)
-Oncogenicity
[Ref by-K. Park/26/158/]
What Is Smallpox
Definition of small pox:
Smallpox is a disease caused by a poxvirus that is transmitted from person to person that causes high fever, characteristic rash, and may kill about one-third of those infected. Smallpox (also called variola) is the only disease that has been completely wiped out throughout the world. Smallpox is also potentially one of the most devastating biological weapons ever conceived.
Cause of Smallpox
Variola (the virus that causes smallpox) is a member of the orthopoxvirus genus, which also includes viruses that cause cowpox, monkeypox, and molluscum contagiosum. Poxviruses are the largest animal viruses, visible with a light microscope. They are larger than some bacteria and contain double-stranded DNA.
Poxviruses are the only viruses that do not need a cell’s nucleus to replicate inside the cell. The variola virus is the only known cause of smallpox. The disease affects only humans. No animal reservoirs or insect vectors (insects that spread a disease) exist, and no carrier state (period when the virus is in the body, but the person is not actively sick) occurs.
Before smallpox was wiped out, the disease survived through continual person-to-person transmission. Pregnant women and children had a heightened risk for the illness. Smallpox also affected them more severely than normal. The virus is only transmitted from human to human; there are no known animal infections.
The virus is acquired from inhalation (breathing into the lungs). Virus particles can remain on such items as clothing, bedding, and surfaces for up to one week.
[Ref by-K. Park/26/158]
Smallpox Risk Factors
Because smallpox has been eradicated, the only risk factor today for contracting the virus is working in a laboratory with the virus or in the event of a biological weapons attack. In the past, risk factors for smallpox included contact with a person with smallpox, contact with infected bodily fluids or contaminated surfaces, or exposure to aerosolized particles (such as from a cough or sneeze) from a person with smallpox.
Symptoms of Smallpox:
Historical accounts show that when someone was infected with the smallpox virus, they had no symptoms for between seven and 17 days. However, once the incubation period (or virus development phase) was over, the following flu-like symptoms occurred:
- high fever
- chills
- headache
- severe back pain
- abdominal pain
- vomiting
These symptoms would go away within two to three days. Then the patient would feel better. However, just as the patient started to feel better, a rash would appear. The rash started on the face and then spread to the hands, forearms, and the main part of the body. The person would be highly contagious until the rash disappeared.
Within two days of appearance, the rash would develop into abscesses that filled with fluid and pus. The abscesses would break open and scab over. The scabs would eventually fall off, leaving pit mark scars. Until the scabs fell off, the person remained contagious.
[Ref by-K. Park/26/158]
Contagious Period for Smallpox
Once the initial symptoms of smallpox appear (high fever, malaise, headache and body aches, and vomiting), people may start to be contagious. This is called the prodrome phase, and it can last from two to four days.
The most contagious period is once the rash develops, and this can last from seven to 10 days following the onset of the rash.
Treatments for Smallpox
In the hospital’s emergency department, a suspected smallpox victim is isolated. All emergency medical services and hospital personnel exposed to someone with smallpox require quarantine and vaccination if they have not been previously vaccinated against smallpox.
1. Isolation: The infected person is immediately placed into strict isolation (as opposed to quarantine, which is used for healthy, asymptomatic people who may have been exposed to the infected person).
2. Quarantine: Anyone who has come into contact with the infected person for up to 17 days prior to the onset of that infected person’s illness (including the treating doctor and nursing staff) may be required to remain in quarantine until a definite diagnosis is made. If the suspected case is indeed smallpox, these individuals will have to remain in quarantine for at least 17 days to ensure that they are not also infected with the virus.
a. If a person in quarantine develops the signs and symptoms of smallpox infection, they are immediately moved to strict isolation.
b. The most likely scenario of a smallpox outbreak is from a terrorist attack or a laboratory accident. Given the highly infectious nature of the organism, researchers estimate that one infected person can infect up to 20 new contacts during the infectious stage of the illness. If one infected person appears at a hospital, it is assumed that more people have been infected.
c. Because of the medical, legal, and social implications of quarantine and isolation, coordinated involvement at the federal, state, and local levels is mandatory. In reality, strict quarantine of a large segment of the population is probably not possible.
d. Infectious disease specialists are consulted, along with state, federal, and local health authorities.
3. Treatment: Medical treatment for smallpox eases its symptoms. This includes replacing fluid lost from fever and skin breakdown. Antibiotics may be needed for secondary skin infections. The infected person is kept in isolation for 17 days or until the scabs fall off.
a. Experiments testing new antiviral medications are in progress, but it will be some time before they produce results. Vaccinations and post exposure interventions are the mainstays of treatment.
(Ref by-K. Park/26/158)
Potential Complications of Smallpox:
Survivors of smallpox may experience severe complications, including
1. deeply scarred skin,
2. blindness,
3. arthritis,
4. Osteomyelitis (bone infection), and fetal infections during pregnancy resulting in additional severe complications or death of the fetus.
Typhoid fever
Definition of Typhoid Fever:
Typhoid fever is the result of systemic infection mainly caused by salmonella typhi.
Or,
It is characterized by a typical continuous fever for 3-4 weeks, relative bradycardia with involvement of lymphoid tissue and constitutional symptoms. Enteric fever: Any of a group of febrile illnesses associated with enteric symptoms caused by salmonella, especially typhoid and paratyphoid fever.
[Ref by-K. Park/26/272]
Epidemiological Features of Typhoid Fever
Bangladesh situation: Typhoid is endemie in Bangladesh. It is the most common cause of febrile illness in the community and hospital in our country.
Agent factors:
- Agent: Salmonella typhi and paratyphi
- Reservoir of infection: Man (cases and carriers)
- Source of infection: Stools and urine of cases and carriers
Host factors:
- Age: Commonest ages of victims are 10 to 30 years, though all age groups are susceptible
- Sex: Cases are more among males but carriers are more in female
- Immunity: Gastric acidity and local intestinal immunity contribute to resistance
Environmental factors:
- Poor socioeconomic environment
- Poor personal hygiene
- Non-availability of safe drinking water
- Inadequate excreta disposal
Incubation period: 10-14 days
Mode of transmission:
- By water and food contaminated with feces and urine of patients and carriers
- Flies may infect foods in which the organisms then multiply to achieve an infective dose.
[Ref by-K. Park/26/273]
Pathogenesis of Typhoid/Enteric Fever:
- Causative agent – Salmonella (at least 106-109microorganisms)
- Route of entry-Faeco-oralroute
- Incubation period – 10-14 days.
| PATHOPHYSIOLOGY Ingest contaminated food ↓ Ingested bacilli invade small intestinal mucosa ↓ Taken up by macrophage & transported to regional lymph node ↓ S.typhi multiply in the intestinal lymphoid tissue ↓ Intact with enterocytes & M celbtileal Peyer’s pathches) during the 1-3 week of incubation period (Diarrhoea) ↓ End of incubation period, bacilli enter bloodstream (Bacteraemia phase) (onset of typhoid fever) ↓ Bacteria invade the gallbladder, biliary system and lymphatic tissue of the bowel and multiply in high number ↓ Then pass into the intestinal tract (stool) |
Or (Another answer)
Pathogenesis of Typhoid/Enteric Fever:
- Causative agent – Salmonella (at least 106-109microorganisms)
- Route of entry- Faeco-oralroute
- Incubation period-10-14 days.
Entry of salmonella to the stomach
Duodenum
|
| Multiply in mononuclear phagocytes of peyer’s patches
|
Intestine
| Penetrate intestinal endothelial
lining Mesenteric lymphnodes [multiply] Via thoracic
↓
duct Enter blood [primary bacterimia]
Intestine
↓ MPS clears bacteria from blood Liver, spleen, Bone marrow, Kidney, lung
↓
Secondary heavy bacterimia [onset of clinical illness
↓
localize Gall bladder, liver, spleen [2nd & 3rdweeks]
↓
Payer patches of intestine
↓
Lymphanc follicles
↓
Necrosis & sloughing Typhoid fever [4th & sthweeks]
[Ref by: Lange Review 140/ 10th +Lange medical microbiology/24th+M.R.Choudhury293/5]
Clinical feature of enteric fever/typhoid fever:
a) Fever-insidious onset
- Temperature rises in step ladder pattern for 4-5 days associated with malaise
- with increase headache.
- Headache and drowsiness
- Myalgia
- Bradycardia
- Constipation (diarrhea and vomiting)
b) End of first week:
- Rose spots on trunk
- Splenomegaly
- Cough
- Abdominal distension
- Diarrhea
c) End of second week:
- Delirium
- Complications
- Coma and death (if untreated)
[Ref By-Davidson/23/339-40]
Preventive and Controlling Measures of Typhoid Fever:
1. Treatment of patients and carriers
2. Education on hand washing, particularly food handlers, patient and children givers
3. Sanitary disposal of feces and control of flies
4. Provision of safe and adequate water
5. Safe handling of food
6. Exclusion of typhoid carriers and patients form handling of food and patients
7. Immunization for people at special risk
8. Regular checkup of food handlers in food and drinking establishment.
Clinical feature of enteric fever/typhoid fever
a) Fever-insidious onset
- Temperature rises in step ladder pattern for 4-5 days associated with malaise
- with increase headache.
- Headache and drowsiness
- Myalgia
- Bradycardia
- Constipation (diarrhea and vomiting)
b) End of first week:
- Rose spots on trunk
- Splenomegaly
- Cough
- Abdominal distension
- Diarrhea
c) End of second week:
- Delirium
- Complications
- Coma and death (if untreated)
Investigation/Diagnostic Test:
a) Blood count (Blood for TC &DC): Leucopenia with relative lymphocytosis.
b) Blood culture: Diagnostic in Is tweek. c) Widaltest: Positive in 2ndweek.
d) Stool & urine culture: Positive in 3rdweek.
e) Bone marrow culture already received antibiotics
Treatment:
A. Specific Rx:
- Ciprofloxacin 500 mg 12 hourly for 14days. Or,
- Cotrimoxazole 960 mg (2tab.) 12 hourly for 14days Or,
- Amoxycillin 750 mg 6 hourly for 14days. Or,
- Chloramphenicol 500 mg 6 hourly for 14days. Or,
- Ceftriaxone 1-2 gm IV 12 hourly for 14days. Or
- Azithromycin 500mg daily for 14days.
B. AchroniccarrieristreatedbyCiprofloxacinfor4wks.Cholecystectomymaynecessary.
C. Symtomatic Rx:
- Complete bed rest.
- Soft nutritious diet.
- Care of oralhygiene.
- Prevention ofbedsore.
- Cold sponging infever.
[Ref By-Davidson/23/339-40]
Complication of Enteric Fever:
A. Bowel:
- Perforation
- Haemorrhage
B. Septicaemiafoci:
- Bone & joint infection (Arthritis, osteomyelitis).
- Meningitis
- Cholecystitis.
- Pneumonia
C. Toxic phenomena:
- Myocarditis
- Nephritis.
D. Chronic carriage:
- Persistent gallbladder carriage
[Ref by-K. Park/26/274]
Multi drug resistant enteric fever:
to chloramphenicol, ampicillin. Cotrimoxazole and tetracycline. Rx:
1. Thus, the fluoroquinoloneremains the drug of choice-
- Ciprofloxacin 500 mg 12 hourly for 14day.
2. Extended-spectrum cephalosporins:
- Ceftriaxone and cefotaxime, are useful alternatives.
3. Where fluoroquinolone resistance is present then-
- Azithromycin (500 mg once daily) has useful alternative.
[Ref by-K. Park/26/273]
Dengue Fever

Epidemiological features:
1. Agent: Dengue virus
2. Reservoir: Man and mosquito
3. Transmission cycle: Man mosquito → Man
4. Host factors: Age and sex – All ages and both sexes are susceptible
5. Environmental factors: Epidemics often during rainy season and post monsoon.
6. Vector: Mosquito (species of Aedes)
7. Mode of transmission: Bite of infected Aedes mosquito
8. Incubation period: 3-10 days (commonly 5-6 days)
[Ref by-K. Park/26/284]
Prevention of dengue:
Mosquito control: the vectors of DF and DHF breed in and around the house.
- Anti-larval measures:
- Environment control (source reduction): The environment should be cleaned up and got rid of water holding containers such as discarded tins, empty pots, and broken bottles and similar other artificial collection of water.
- Chemical control: Larviciding – temophos (abate) can be freely used in water collection
- Anti-adult measures: Residual sprays
- Protection against mosquito bites:
-Use of Mosquito net
-Use of Mosquito repellents (Diethyltolenamide)
a) Notification: Occurrence of epidemics needs to be reported
b) Appropriate treatment of DF and DHF.
c) Vaccine:
- A live attenuated vaccine effective against all 4 strains of the dengue virus
- Clinical traits in adult volunteers have shown the vaccine to be safe and the immunological response to be encouraging.
[Ref by-K. Park/26/294]
Clinical features:
A. Prodromal (2 days): Malaise, Headache
B. Acute:
- Fever: Acute onset, high, continuous or, saddle back, with break on 4-5th day and lasting 2-8 days
- Headache, backache, arthralgia
- Generalized pain-break bone fever
- Pain on eye movement, lacrimation
- Anorexia, nausea, vomiting
- Depression
- Relative bradycardia
- Lymphadenopathy
- Rash transient macular in first 1-2 days
-Maculopapular, scarlet
-From 3-5th day on trunk, spreading centrifugally sparing palm and sole
-May desquamate on resolution
-Prostration
-Scleral injection
C. Convalescence- slow
D. Any of the following hemorrhagic manifestation: Petechiae, purpura, echymosis, epistaxis, gum bleeding and haematemesis
E. Features of shock – manifested by
-Sweating on forehead
-Rapid thread pulse
-Hypotension
-Shallow breathing
-Cold clammy skin
-Restlessness
-Oliguria
Management of DHF:
a) Management of DHF during the febrile phase is similar to that of DF
b) Oral electrolyte solution of fruit is juice is recommended during the febrile phase
c) Monitor:
- Platelet count and Het value should be estimated at least daily.
- Frequent recording of vital signs is recommended for adjusting replacement avoiding over hydration
d) Fluid therapy: A rise of haematocrit of 20 or more indicates the need for IV fluids therapy
- Ringers lactate solution
- 0.9% W/V normal saline
- 5% dextrose in half strength normal saline solution
e) Blood transfusion: In case of significant/ severe bleeding
f) Shock: In case of shock give oxygen
g) Acidosis: For acidosis use sodium bicarbonate
h) Evaluation of patients condition
- Frequent recording of vital signs
- Pulse, BP, respiration and temperature every 30 minutes
- Monitoring of urine output
- Platelet court and haematocrit determination
- Haematocrit level 2 hours for first 6 hours then every 4 hours
- Fluid balance sheet
Grading the severity of the DHF:
- Gradel: Fever accompanied by nonspecific constitutional symptoms the only hemorrhagic manifestation is appositive tourniquet test.
- Gradell: Above sign plus spontaneous bleeding
- GradeIII: Above sign plus circulatory failure
- Grade IV: Profound shock: undetectable BP and pulse (Grade III and Grade IV known as DSS)
Clinical laboratory investigation in DHF:
- Haematocrit – increase 20%
- Platelet count – Thrombocytopenia
- WBC count and DC
- Coagulograme. PT, partial thromboplastin time, fibrinogen level and fibrinogen degradate products
- Serum protein particularly albumin
- Liver function tests
- Serum electrolyte particularly sodium
- Blood gas analysis
- Renal function and urine examination
- Serum complements
- Stool examination OBT
- ECG
- Chest X-ray
- USG of abdomen
- CSF. Plus
- Diagnosis for dengue virus isolation and serology (IgM and IgG).
[Ref by-K. Park/26/288-90]
Malaria
Definition of malaria:
Malaria is a protozoal disease caused by infection with parasites of the genus plasmodium and transmitted to man by certain of infected female anophelene mosquito.
Epidemiological features:
A) Agent factors:
a) Agent: Malaria in man is caused by 4 distinct species of malaria parasite
-Plasmodium vivax
-Plasmodium falciprum
-Plasmodium malariae
-Plasmodium ovale
b) Reservoir of infection: Human
c) Period of communicability: Malaria is communicable as long as gametocytes exist in the blood to infect vector mosquito.
B) Host factors:
-Age: Malaria affects all ages
-Sex: Male are more exposed than female
-Social and economic factor: More in underdeveloped countries
-Housing: More in all ventilated and ill lighted house
-Pregnancy: The risk
-Occupation: More in agriculture practitioner
-Human habits sleeping out of house and mosquito net
C) Environmental factors:
-Season: Maximum prevalence is from July to November
-Temperatures: 20°C -30°C
-Humidity: 60%
-Rain fall: Necessary for breeding
D) Mode of transmission:
- Vector transmission: Infected female anopheles mosquito
- Direct transmission:
-Blood transmission
-Infected needles
-Congenital-very very rare
E) Incubation period: Varies according to species –
-12 (9-14) days for P. falciparum
-14 (817) days for P. vivax
-28 (18-40) days for P. malaria
-17 (16-18) days for ovale malaria
[Ref by-K. Park/26/294-95]
History and investigation of malaria
a) Patient may give H/O travel of malarious locality
b) Onset is insidious with malaise, headache, vomiting
c) Fever:
-No particular pattern
-Cold, hot and sweating stages are seldom found
-Not so high temperatures
d) Cough and mild diarrhea
e) Weakness
f) Patient may present with complication of the disease
-Unconsciousness
-Acute renal failure
-Black water fever
-Acute renal respiratory syndrome
-Septicemia
One examination (O/E):
-Patient anemia
-Jaundice may present
-Increase Temperature
-Hepato splenomegaly
Lab. diagnosis of malaria:
A) Direct evidences
-Thick film: To detect the presence of parasite
-Thin film: To detect the species of parasite
B) Indirect evidences:
-Serological test
-Blood for TC, DC, ESR, H6%
-Liver function test
-Examination of urine
[Ref by-K. Park/26h/301-302]
Management of malaria
A) Uncomplicated malaria:
| Day | Drug and dose | Tablet | Total dose |
| 1 | Chloroquine (150 mg) | 4 tab. single dose once after meal | 600 mg |
| 2 | Chloroquine (150 mg) | 3 tab. single dose once after meal | 450 mg |
| 3 | Chloroquine (150 mg) | 3 tab. single dose once after meal | 450 mg |
| 4 | Primaquine 15 mg | 3 tab. single dose |
B. Treatment of Chloroquine resistant malaria/Treatment failure malaria: In most areas of the world P. falciparum is now resistant to chloroquine.
| Day | Drug and dose | Tablet | Total dose |
| 1 | Quinine 300 mg base | 2 tab. (8 hourly 3 times daily) | 600 mg |
| 2 | Quinine 300 mg base | 2 tab. (8 hourly 3 times daily) | 600 mg |
| 3 | Quinine 300 mg base | 2 tab. (8 hourly 3 times daily) | 600 mg |
| 4 | Quinine 300 mg base + Fansider | 2 tab. (8 hourly 3 times daily) + 3 tab. single dose 2 time daily | 600 mg |
On 8 ^ (th) day primaquine 15 mg single dose 3 tablet
B) Severe malaria/cerebral malaria:
a. Loading dose: Quinine dihydrochloride 20 mg/kg bdoy weight by IV infusion
b. Maintenance dose: After 8 hours
- Quinine salt: 10 mg/kg body weight, over 4 hours by IV infusion
- Maintenance dose should be continued 8 hurly until the patient can swallow tab to complete the 7 day course
c. Fansidar single dose on the 3rd day
d. Primaquine single dose on the 4th day
[Ref by-K. Park/26/302-304]
Life cycle of malaria parasite:
Life cycle of malaria parasite: the cycle is completed by two cycle, 1) human cycle, 2) Mosquito cycle
Schizogony or asexual human cycle:-
Mosquito bite sporozoite enters → exoerythrocytic cycle in hepatocytes → merozoites → enter red cell ring → trophozoite → mature trophozoite → immature schizont → mature schizont → merozoites → enter red cells → microgametocyte and macro gametocyte the cycle is repeated
Sporogony or sexual mosquito cycle:-
Mosquito bite infected human and takes blood → fertilization of microgamete and macrogamete → zygote → oocyst → sporozoites in oocyst → sporozoites in salivaof mosquito → the cycle is repeated.
Causative Agent:
Malaria in man is caused by 4 distinct species of malaria parasite
-Plasmodium vivax
-Plasmodium falciprum
-Plasmodium malariae
-Plasmodium ovale
The factors those are responsible for difficulties of malaria eradication programme in Bangladesh are –
a. Administrative fallure:
-Shortage of finance, manpower, drugs, insecticides transport
-Shortage of administrative personnel’s
b. Technical failure: Development of insecticides in vector and parasitic resistance to drugs
c. Operational failure: Due to inadequate surveillance, case detection and treatment
d. General failure:
- Common border of Bangladesh and India
- Sleeping without mosquito net
- Poor standard of environmental sanitation
- Lack of health education
e. Epidemiological factors:
- Presence of extra-lumax reservoir of infection
- Presence of human carrier state
- Presence of sub clinical cases.
[Ref by-K. Park/26/302-304]
Control of malaria:
A. Measures to be applied by the individual:
- Prevention of man/Vector contact: Using repellants protection clothing bed-nets screening of houses
- Destruction of adult mosquitoes: Use of domestic space spray
- Destruction of mosquito larvae: Peri-domestic sanition intermittent during of water container
- Source reduction: Small scale drainage system
- Measures against malaria parasite: Chemoprophylaxis and chemotherapy
B. Measures to be applied by the community:
- Prevent of man/vector contact: Site selection and screening of houses
- Destruction of mosquito larvae: Using larvicides
- Source reduction: Prevention of manmade malaria environment sanitation water management
- Measures against malaria parasite: Presumptive treatment radical treatment mass drug administration.
Rabies
Definition:
Rabies (also known as hydrophobia) is an acute highly fatal viral disease of the central nervous system caused by lyssavirus type 1.
Epidemiological features:
A) Occurrence: It occurs throughout the world except in develop countries. Rabies is endemic in Bangladesh.
B) Ecological triad:
♦ Agent: Rabies virus (Lyssavirus type 1) it is RNA virus
♦ Host: Rabies virus can infect all mammals. Man is infected accidentally
♦ Environment: It may occur at any time but is more prevalent in the summer months
C) Natural history:
♦ Reservoir: Stray and pet dogs, cats, fox, wolf, jackal, hyena etc.
♦ Source of infections: saliva of the rabid animals.
♦ Mode of transmission:
- Animal bites: By rabid dog bites
- Licks: Saliva comes in to direct contact with mucosa or fresh skin wounds
- Human to human Transmission by bite is theoretically possible and evidence is also present
- Others: Rarely, by inhalation of virus containing aerosol or transplantation of an infected organ.
- Incubation period: Commonly 3-8 weeks, but may vary from 4 days to many years
[Ref by-K. Park/26/317-318]
Clinical features:
A) Prodromal symptoms:
General
Headache
Sore throat
Slight fever for 3-4 days
- Local: Paraesthesia (pain and tingling) at the site of the bite 80% patient complain
B) Systemic manifestation:
a) Furious rabies (seen in most patients):
I. Sympathetic system:
- Dilation of the pupil
- Increase sweating
- Increase salivation
- Increase lacremation
II. Motor system: Increase reflexes and muscle spasm
III. Mental change:
- Anxious
- Anger
- Irritable
- Fear of death
- Depression
- Delusion and hallucination may developed accompanied by spitting, biting and mania
IV. Sensory system: Intolerant to noise bright light a cold draught of air, aerophobia may presentIV. Sensory system: Intolerant to noise bright light a cold draught of air, aerophobia may present
a) Paralysis and death: Death may occur due to respiratory paralysis.
Treatment:
A) Post exposure prevention: Post-exposure prophylaxis depends on the category of exposure.
- Wound wash: Wash the wound with running tap water or speedy running water and soap for 15 minutes
- Assess the wound: According to WHO guideline
- Vaccination: anti rabies vaccination (ARV) with IDRV/TCV
- RIG: in category III exposure (not later than 7 days after 1″ vaccination)
- Tetanus toxoid: When indicated
- Systemic antibiotic: where necessary
B) Symptomatic rables:
- Treatment of rabies patients should be supervised by MOs and referral to appropriate
- health facility to be done There is no specific treatment of rabies. Supportive and symptomatic treatment is the aim.
- Patient should be in isolation in a quiet room protected as far as possible from bright light, noise and clod draughts of air.
Immunization regimen with IDRV: (Intra-dermal rabies practiced in government hospitals at free of cost)
| Vaccine | Day | Dosage |
| 1 dose 2 dose 3 dose 4 dose | D0 D3 D7 D28
| 0.1ml * 2 (0.1 ml into each deltoid region) 0.1ml * 2 (0.1 ml into each deltoid region) 0.1ml * 2 (0.1 ml into each deltoid region) 0.1ml * 2 (0.1 ml into each deltoid region) |
Immunization regiment of ARV (IM Injection):
- One dose of vaccine (1 ml, same for children, adolescents and adult) on days: 0, 3, 7, 14, 28, (5 doges schedule) or
- Two dose of vaccine (right and left deltoid muscle) on day 0, and one dose is applied in to the deltoid muscle on days 7 and 21 (2-1-1 regimen). In small children the vaccine is to be given in to the thighs.
[Ref by-K. Park/26/317-318]
Rabies can be controlled in the following way:
- Licensing and vaccination of domestic dogs
- Killing of stray dogs
- Monitoring of reservoir hosts
- Control and quarantine of imported animals
- Vaccination of at-risk animals and man (pre-exposure prophylaxis) Post exposure measurement (local treatment of wound and immunization)
- Health education of people regarding the care of dogs and prevention of rabies.
[Ref by-K. Park/26/319]
Diagnosis a case of rabies from dog bite:
a) Clinical diagnosis:
- History of bite by rabid animal
- Characteristics signs and symptoms of rabies
b) Laboratory diagnosis:
- The head of the animal, duly packed in ice in an air tight container is sent for laboratory examination.
- Microscopic examination: Identification of regri bodies in the brain
- Fluorescent antibody test for diagnosis of rabies within a few hours
- Animal (mice) inoculation test with brain tissues of rabid animal.
Types of Rabies Vaccine:
There are two basic types of rabies vaccine –
- A preventative vaccine that is available for both dogs and humans, and
- The post-exposure series of vaccinations given to individuals that have been bitten by a suspect animal
Define hydrophobia
A term once commonly used for rabies because in the later stages of that disease, the animal (or person) has difficulty swallowing and so fears a drink of water. Literally, an irrational fear of water, to drink or to swim in. Someone who is scared of the water is hydrophobic
Or,
A symptom of rabies in humans consisting of an aversion to swallowing liquids.
Causes of Hydrophobia:
Hydrophobia can be a very dangerous, crippling disease that can lead to severe mental problems and create social obstacles, such as the inability to bathe. Hydrophobia can also be caused by rabies and noticed in the later stages of infection. In the latter case, it is imperative you visit a health professional immediately.
Symptoms of Hydrophobia:
Since Earth is made up of about 70 percent of water, it is easy to see why this fear can be a very difficult one to live with. If you notice common symptoms associated with hydrophobia, consider visiting a health professional to discuss the treatment options available to you. Here are several situations in which a hydrophobic person may be uncomfortable with:
- Fear of drowning or being submerged, even by irrational amounts of water.
- Avoiding any and all situations in which a body of water may be present.
- Avoidance of most liquids, not just water.
- Keeping a distance from liquid sources such as sinks and showers.
aquaphobia
Aquaphobia is a specific phobia. This is an irrational fear of something that doesn’t cause much danger. You may have aquaphobia if you find that any source of water causes you an excessive amount of anxiety. This can include a swimming pool, a lake, an ocean, or even a bathtub.
Aquaphobia is often mistaken for another phobia called hydrophobia. Even though they both involve water, aquaphobia and hydrophobia aren’t the same. Hydrophobia is an aversion to water that develops in humans during the later stages of rabies.
Symptoms of aquaphobia:
Seeing water can trigger intense fear and anxiety in a person with aquaphobia. This could be a very small amount of water, like what’s found in the bathroom sink, or a large body of water, such as an ocean. The amount of water isn’t what causes the phobia. It’s the water itself that creates the fear and resulting anxiety.
Some of the more common symptoms of aquaphobia include:
- an immediate feeling of intense fear, anxiety, and panic when thinking about water
- a persistent, excessive, or unreasonable fear when exposed to water recognizing that the fear of water is excessive or out of proportion to the actual threat
- avoidance of water
- sweating
- rapid heartbeat
- tight chest and difficulty breathing
- nausea
- Dizziness or fainting.
[Ref by-K. Park/26]
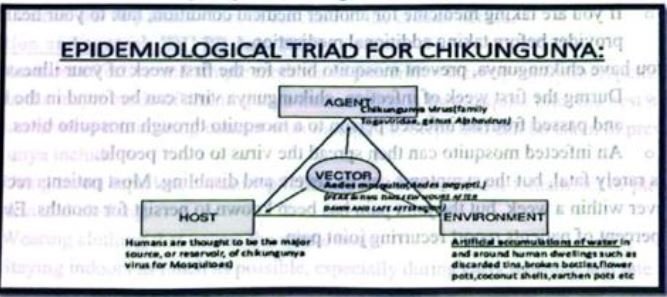
Chikungunya
Chikungunya (pronunciation: chik-en-gun-ye) virus is transmitted to people by mosquitoes. The most common symptoms of chikungunya virus infection are fever and joint pain. Other symptoms may include headache, muscle pain, joint swelling, or rash.
Outbreaks have occurred in countries in Africa, Asia, Europe, and the Indian and Pacific Oceans. In late 2013, chikungunya virus was found for the first time in the Americas on islands in the Caribbean. There is a risk that the virus will be imported to new areas by infected travelers.
There is no vaccine to prevent or medicine to treat chikungunya virus infection. Travelers can protect themselves by preventing mosquito bites. When traveling to countries with chikungunya virus, use insect repellent, wear long sleeves and pants, and stay in places with air conditioning or that use window and door screens.
History
The word “chikungunya” comes from the Makonde (or Kimakonde) language, spoken on the Makonde plateau where the disease was first described. It means, “that which bends up,” “to become contorted,” or “to walk bent over,” describing the stooped appearance of patients with joint pain.
Chikungunya is an RNA virus and a member of the Togaviridae family. The disease was first described during an outbreak in Tanzania in 1952. Immediately after the first description of the disease, there was a wealth of scientific papers published covering the new condition. This initial interest all but disappeared until a fresh outbreak occurred in and around the Indian Ocean in 2005.
Historically, chikungunya was considered a tropical disease because it had only been documented in Africa, Asia, and India. However, since 2007, outbreaks have occurred in Italy, France, Croatia, and the Caribbean islands. In total, more than 60 countries have identified cases of chikungunya virus.
Define Chikungunya
Chikungunya is an infection caused by the chikungunya virus (CHIKV), Symptoms include fever and joint pain. These typically occur two to twelve days after exposure. Other symptoms may include headache, muscle pain, joint swelling, and a rash.
Symptoms
- Most people infected with chikungunya virus will develop some symptoms.
- Symptoms usually begin 3-7 days after being bitten by an infected mosquito.
- The most common symptoms are fever and joint pain.
- Other symptoms may include headache, muscle pain, joint swelling, or rash.
- Chikungunya disease does not often result in death, but the symptoms can be severe and disabling
- Most patients feel better within a week. In some people, the joint pain may persist for months
- People at risk for more severe disease include newborns infected around the time of birth, older adults (265 years), and people with medical conditions such as high blood pressure, diabetes, or heart disease.
- Once a person has been infected, he or she is likely to be protected from future infections.
Diagnosis:
- The symptoms of chikungunya are similar to those of dengue and Zika, diseases spread by the same mosquitoes that transmit chikungunya.
- See your healthcare provider if you develop the symptoms described above and have visited an area where chikungunya is found. peg stitems in dilera anast
- If you have recently traveled, tell your healthcare provider when and where you traveled.
- Your healthcare provider may order blood tests to look for chikungunya or other similar viruses like dengue and Zika
Treatment
- There is no vaccine to prevent or medicine to treat chikungunya virus.
- Treat the symptoms
- Get plenty of rest
- Drink fluids to prevent dehydration.
- Take medicine such as acetaminophen (Tylenol®) or paracetamol to reduce fever and pain
- Do not take aspirin and other non-steroidal anti-inflammatory drugs (NSAIDS until dengue can be ruled out to reduce the risk of bleeding).
- If you are taking medicine for another medical condition, talk to your healthcare provider before taking additional medication.
- If you have chikungunya, prevent mosquito bites for the first week of your illness.
- During the first week of infection, chikungunya virus can be found in the blood and passed from an infected person to a mosquito through mosquito bites.
- An infected mosquito can then spread the virus to other people.
1 year, 20 percent of patients report recurring joint pain.
- naproxen
- ibuprofen
- acetaminophen
For longer-lasting aches, physiotherapy may be helpful.
Chikungunya vaccine:
Currently, there is no vaccine or antiviral treatment, but, in general, the disease is short-lived and rarely fatal. Medication focuses on relieving the symptoms rather than the cause. The National Institute of Health (NIH) are currently funding a phase 2 clinical trial of a chikungunya vaccine. The vaccine consists of so-called virus-like particles (VLPs) rather than inactivated or weakened viruses.
VLP-based vaccines can stimulate immune responses simular to those generated by naturally acquired immunity following viral infection. However, VLPs are not infectious and cannot replicate. Since whole viruses are not used to produce VLP vaccines, they do not need to be prepared in high-level biocontainment facilities.
Complications can include:
- Uveitis-inflammation of the layer in the eye between the inner retina and the outer fibrous layer composed of the sclera and cornea.
- Retinitis-inflammation of the retina.
- Myocarditis-inflammation of the heart muscle.
- Hepatitis-inflammation of the liver.
- Nephritis-inflammation the kidneys.
- Hemorrhage – bleeding.
- Meningoencephalitis – inflammation of the membranes of the brain and adjoining cerebral tissue.
- Myelitis-inflammation of the spinal cord.
- Guillain-Barré syndrome – rare peripheral nervous system disease characterized by muscle weakness.
- Cranial nerve palsies-loss of function in the cranial nerves.
Prevention and control: [DU PB July 20171
One of the most effective and simple methods of prevention is using mosquito repellent. Seeing as the major mode of chikungunya transmission is by mosquito bite, the best methods of prevention involve minimizing contact with mosquitos. Steps that can be taken to prevent chikungunya include:
- Using insect repellent containing DEET (N, N-Diethyl-meta-toluamide) or picaridin on skin and clothing.
- Wearing clothing that covers the whole body.
- Staying indoors as much as possible, especially during early morning and late afternoon.
- Avoiding traveling to areas experiencing outbreaks.
- Using products containing oil of lemon eucalyptus or PMD (p-Menthane-3,8-diol) can be effective.
- Using air-conditioning – this deters mosquitos from entering rooms.
- Sleeping under a mosquito net.
- Using mosquito coils and insecticide vaporizers.
Although chikungunya is very rarely fatal, the symptoms are distressing and can be long-lived. Avoiding mosquitos is key.
[Ref by-K. Park/26/330-3361]