concept of nasogastric tube – This book covers the entire syllabus of “Nutrition and Dietetics” prescribed by BNMC for all Diploma in Nursing Science and Midwifery students. We tried to accommodate the latest information and topics. This book is an examination-friendly setup according to the teachers’ lectures and examination questions.
At the end of the book previous university questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourish. The unique way of presentation may make your reading of the book a pleasurable experience.
Concept of nasogastric tube
Nasogastric tube is a tube that is passed through the nose and down through the nasopharynx and esophagus into the stomach.
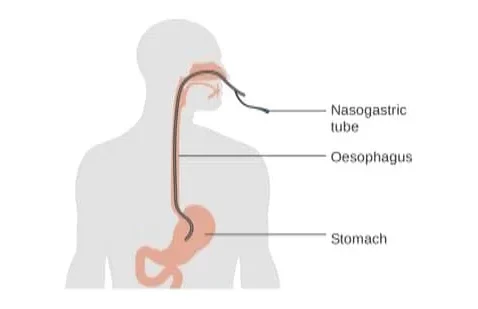
A nasogastric tube is a tube that is inserted into the stomach through the nose. This flexible tube can contain one or two inner ducts and is connected to an external device.
Types of Nasogastric Tube:
There are mainly two types of NG Tube-
| 1. Wide bore tubes (usually PVC): |
|
| 2. Fine bore tubes (polyurethane): |
|
Definition of Nasogastric (NG) Intubation:
Nasogastric intubation is a medical process involving the insertion of a plastic tube (nasogastric tube or NG tube) through the nose, past the throat, and down into the stomach.
Or,
Passing a tube through the nose to the stomach is called nasogastric intubation.
(Ref by-SN Nanjunde Gowda’s/2nd/451)
Purposes of Nasogastric Intubation:
1. To remove fluid and gas from gastrointestinal (decompression) tract.
2. Prevent or relieve nausea and vomiting after surgery.
3. To treat patients with mechanical obstruction and bleeding of the upper gastrointestinal tract.
4. To obtain a specimen of gastric contents for laboratory studies.
5. Administer medications and feeding directly into gastrointestinal tract.
(Ref by-SN Nanjunde Gowda’s/2nd/451)
Indication of Nasogastric Intubation:
A. Diagnostic indications for NG intubation include the following:
- Evaluation of upper gastrointestinal (GI) bleeding (ie, presence, volume)
- Aspiration of gastric fluid content
- Identification of the esophagus and stomach on a chest radiograph
- Administration of radiographic contrast to the GI tract
B. Therapeutic indications for NG intubation include the following: Gastric decompression, including maintenance of a decompressed state
- after endotracheal intubation, often via the oropharynx Relief of symptoms and bowel rest in the setting of small-bowel obstruction
- Aspiration of gastric content from recent ingestion of toxic material
- Administration of medication
- Feeding
- Bowel irrigation
Contraindication of Nasogastric Intubation:
A. Absolute contraindications for NG intubation include the following:
- Severe mid-face trauma
- Recent nasal surgery
B. Relative contraindications for NG intubation include the following:
- Coagulation abnormality
- Esophageal varices (usually, a Sengstaken-Blakemore tube is introduced, but an NG tube can be used for lower-grade varices) or stricture
- Recent banding of esophageal varices
- Alkaline ingestion (the tube may be kept if the injury is not severe)
Procedure of Nasogastric Intubation:
A. Equipment’s for nasogastric intubation:
The following equipment is needed (also see image below):
- Nasogastric tube
-Adult-16-18Fr
-Pediatric In pediatric patients, the correct tube size varies with the patient’s age. To find the correct size, add 16 to the patient’s age in years and then divide by 2 (eg. [8 y+ 16)/212Fr)
- Viscous lidocaine 2%
- Oral analgesic spray (Benzocaine spray or other)
- Syringe, 10 mL
- Glass of water with a straw
- Water-based lubricant
- Toomey syringe, 60 mL
- Tape
- Emesis basin or plastic bag
- Wall suction, set to low intermittent suction
- Suction tubing and container
B. Positioning
- Position the patient seated upright.
C. Procedure:
1. Check the physician’s order, progress notes and nursing care plan.
2. Identify the patient.
3. Explain the procedure to the patient.
4. Pre-determine a signal by which the patient can communicate if he/she require the nurse to halt the procedure, e.g. raise his/her hand.
5. Collect and prepare the equipment.
6. Ensure the patient’s privacy.
7. Help the patient into a comfortable position. Sitting upright either in a bed or on a chair. Support the patient head with pillows.
8. Observe the patient throughout this procedure.
9. Remove the patient’s dentures, if present place in labeled container.
10. Wash and dry hands.
11. Check the patient’s nostrils. Request patient to sniff each nostril in turn or clean the nostrils if necessary.
12. Ask the patient of any nasal defect or tenderness in order to avoid attempting to pass the tube through a defective nasal passage.
13. Establish the distance that the tube is to be passed by measuring the distance on the tube from the patient’s ear lobe to the bridge of the nose to the bottom of the Xiphistemum.
14. Using clean technique assemble the equipment.
15. Lubricate about 15-20 cm of the tube with water soluble jelly, which has been placed on a gauze swab.
16. Ask the patient to relax as much as possible while the tube is passed.

17. Insert the tube and slide it gently but firmly inwards and backwards along the floor of the nose to the nasopharynx. If an obstruction is felt withdraw the tube and try again or use another nostril.
18. Encourage the patient to swallow and breath through his mouth when the tube reaches the pharynx keeping the chin down and head forward to assist the passage of the tube.
19. Advance the tube until the length previously measured has been inserted and the mark has reached the external nares. If the patient shows any signs of distress, e.g. gasping or cyanosis, remove the tube immediately.
20. Ascertain whether the tube is in the stomach by:
- Aspirating the contents of the stomach with a syringe. The aspirate should turn blue litmus paper red.
- Place the stethoscope over the epigastrium and inject 2-3 ml of air to the tube.
21. Secure the tube to the patient’s nose with tape. Secure the free-end of the tube in the suitable position avoiding visual obstruction.
22. Aspirate the stomach contents as per the order of the doctor (if required dispatch specimen to laboratory).
23. Ensure that the patient is left feeling as comfortable as possible.
24. Clean and dispose of the equipment
25. Wash hands.
26. Initiate and maintain intake and output chart.
27. Document the nursing procedure appropriately, monitor after effects and report any abnormal findings immediately.
(Ref by-SN Nanjunde Gowda’s/2nd/452)
Confirmation of NG Tube Inserted Properly:
- Aspiration will bring out gastric contents.
- A few cc. of air is injected into the tube and at the same time auscultation done over epigastrium if the tube is in the stomach, a gurgling sound will be heard.
- In case of Ryle’s tube, a plan X-ray will locate the metallic bead at the tip.
Complications Nasogastric Intubation:
1. Patient discomfort
- Generous lubrication
- Throat irritation
2. Epistaxis
3. Aspiration
4. Weight loss
5. Elevated electrolytes
6. Diarrhea
7. Nausea & Vomiting
8. Constipation
9. Middle ear inflammation
10. Elevated blood sugar
11. Esophageal perforation
Procedure of Removing Nasogastric Tube:
- Remove the adhesive taper on the nose.
- Clamp the tube to prevent any leakage of fluid.
- Ask the patients to take a deep breath and to hold the breath while we steadily and quickly removed the tube. Holding the breathe closes the glottis and prevents the possibility of aspiration. Dispose the tube.
- Provide gauze to the patients to blow the nose and a glass of water to clear the throat. Offer to cleanse the mouth and/or nose. Leave the patient in a comfortable position.
- Record the removal of the tube.