Iron Deficiency Anaemia – This book covers the entire syllabus of “Nutrition and Dietetics” prescribed by BNMC-for all Diploma in Nursing Science and Midwifery students. We tried to accommodate latest information and topics.
This book is examination friendly setup according to the teachers’ lectures and examination’s questions. At the end of the book previous university questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourished. The unique way of presentation may make your reading of the book a pleasurable experience.
Iron Deficiency Anaemia
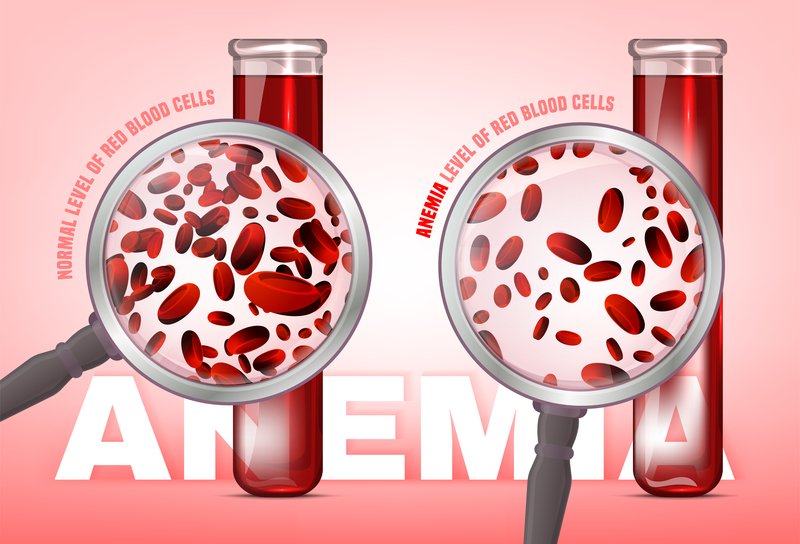
Definition of Iron Deficiency Anaemia:
Iron deficiency anemia develops when body stores of iron drop too low to support normal red blood cell (RBC) production. Inadequate dietary iron, impaired iron absorption, bleeding, or loss of body iron in the urine may be the cause.
or
Iron deficiency anaemia is caused by lack of iron, often because of blood loss or pregnancy. It’s treated with iron tablets prescribed by a GP and by eating iron-rich foods.
Causes of Iron Deficiency Anaemia
a) Increased physiological demand –
- Children during period of growth
- Women during reproductive age:
- Menstruation: 15-30 mg Fe loss
- Pregnancy: 500-600 mg Fe loss
- Parturition
- Lactation
b) Pathological blood loss:
- Injury
- Hookworm infestation
- Bleeding piles
- Peptic ulcer
- Chronic aspirin ingestion
- Haemorrhoids
- Esophageal varices
- Hiatus hernia
- Carcinoma of stomach, colon
- Ulcerative colitis
- Surgical operation
c) Inadequate iron intake:
- Deficient diet
- Gastrectomy or gastro-enterectomy
- Tropical sprue
- Coeliac disease
Clinical Features of Iron Deficiency Anaemia:
a) General feature of anaemia:
- Nonspecific symptoms:
✓ Tiredness
✓ Breathlessness
✓ Ankle swelling - Nonspecific signs:
✓Mucous membrane pallor
✓ Tachypnea
✓ Raised JVP
✓ Flow murmur
✓ Ankle oedema
✓ Postural hypotension
✓ Tachycardia
b) Features of iron deficiency anaemia: Glossitis, Dysphagia, Koilonychias
Treatment of Iron Deficiency Anaemia:
- Tab. ferrous sulphate 200 mg 3 times daily for 3 to 6 months after the hemoglobin become normal.
- If patient intolerable to ferrous sulphate – Ferrous gluconate 300 mg 12 hourly
- Parenteral iron therapy (in severe anaemia especially in late pregnancy, in mal-absorption, haemosiderinuria, unable to take by mouth)
✓ Iron sorbitol 1.5 mg/kg single dose daily intramuscular injection (never IV)
✓ Iron dextrain IV (anaphylactic reaction may occur) or IM (local irritation) - Blood transfusion – IDA with angina, HF or evidence of cerebral hypoxia
- Supportive Rx: If infection – antibiotic
Investigation of Iron Deficiency Anaemia:
✓ Blood for TC, DC, ESR, Hb%:
- Hb%-Reduced
- ESR-Slightly raised
- TC-Reduced
✓ Peripheral blood film:
- Microcytic and hypochromic anaemia
- Target cell, tear drop cell, pencil cell
✓ Biochemical test: Serum ferritin: < 12 µg/L (most specific), (Normal 15-300 µg/L), TIBC increase, Plasma iron increase
✓ For the diagnosis of cause:
- Occult blood test
- Upper and lower GIT endoscopy, Ba studies
- Stool and urine study for parasites (in tropics)
Prevention Of Iron Deficiency Anaemia:
1. Iron and folic acid supplementation. If haemoglobin is between 10-12 g/dl, dosage for
a) Mothers: 1 tablet (60mg of elemental iron + 0.5 mg folic acid) daily for 2 to 3 months or longer depending upon the progress,
b) Children (6 months to 1 and 2 years): tablet (20mg of elemental iron + 0.1 mg of folic acid) daily.
2. Iron fortification, e.g. Iron Fortified Salt.
3. Others: Changing dietary habits, control of parasites, and nutrition education.