Esophageal atresia/tracheoesophageal fistula- This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Esophageal atresia/tracheoesophageal fistula
Esophageal atresia
Esophageal atresia (EA) is failure of the esophagus to form a continuous passage from the pharynx to the stomach during embryonic development. It is usually associated with tracheoesophageal atresia.
Or
Esophageal atresia is a disorder of the digestive system in which the esophagus does not develop properly. The esophagus is the tube that normally carries food from the mouth to the stomach.
Or
Esophageal atresia is a congenital medical condition (birth defect) that affects the alimentary tract. It causes the esophagus to end in a blind-ended pouch rather than connecting normally to the stomach.
Tracheoesophageal fistula
Tracheoesophageal fistula (TEF) is an abnormal connection between the trachea and esophagus. These disorders are commonly among premature or low birth weight infant and mothers having polyhydramnios. Congenital heart diseases or other gastrointestinal anomalies may present along with these condition.
Or
Tracheoesophageal fistula is an abnormal connection in one or more places between the esophagus (the tube that leads from the throat to the stomach) and the trachea (the tube that leads from the throat to the windpipe and lungs). Normally, the esophagus and the trachea are two separate tubes that are not connected.
Or
It is a congenital communication between the trachea and esophagus.
Or
It is a congenital communication between the trachea and esophagus. Approximately 17-70% of children with TEFs have associated developmental anomalies like-
- Down syndrome.
- Duodenal atresia.
- Cardiovascular defect.
Clinical features of tracheoesophageal fistula
Neonates with TEF usually develop-
1. Copious, fine white frothy bubbles of mucus in the mouth and nose.
2. Secretions recur despite suctioning
3. Infants may develop
4. Rattling respiration
5. Episodes of coughing.
6. Choking in association with cyanosis.
7. Symptoms worsen during feeding in the presence of a TEF.
Or (Another answer)
Tracheoesophageal fistula symptoms
These include:
1. Abdominal distension
2. Profuse, white frothy bubbles of mucus in the mouth and nose
3. Frequent coughing
4. Vomiting
5. Choking
6. Fever
7. Sucking in of food particles or fluids into the lungs
8. Groaning noises while breathing
9. Cyanosis, abnormal blue discoloration of the skin and mucous membranes.
Causes of tracheoesophageal fistula
The exact cause of these anomalies is not known in most cases.
Some factors influencing the incidence of the problems are-
These anomalies may develop due to-
- Aberration or deviations of the septum between the esophagus and trachea or altered growth of septum between them.
- TEF results due to-
➤ Failure of growth along the septum.
➤ EA develops due to-
➤ Deficient growth of the dorsal wall.
Some of its possible causes may include
- Surgical excision of the larynx
- Blunt thoracic injuries
- Neck trauma
- Tremendous pressure exerted by a cuffed endotracheal tube during lung ventilation
- Lung cancer
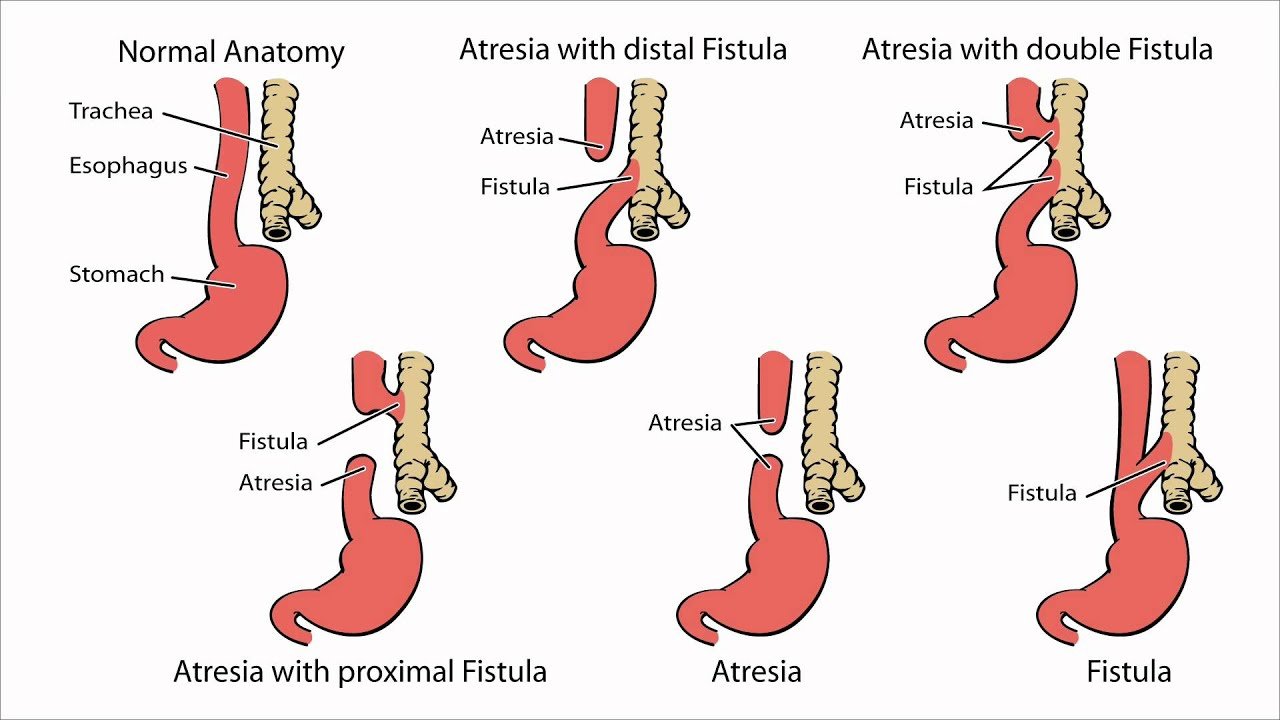
Classifications of EA & TEF
EA with TEF can be classified as follows –
Type-I:
- EA without fistula (87a): It is second most common type. There is no connection of esophagus to trachea. The upper (proximal) segment and low (distal) segment of esophagus are blind.
Type-II:
- EA with TEF (upper): It is rare and found in less than I percent of all cases. Upper segment of esophagus open into trachea by a fistula. The distal or lower segment is blind.
Type-III:
- EA with TEF (lower) (80-90%): It is the most common type. In this condition, proximal or upper segment of the esophagus has blind end. The distal lower-segment of esophagus connects into trachea by a fistula.
Type-IV:
- EA with TEF both upper and lower segment: It is also rare (less than 1%). There is EA with fistula between both proximal and distal ends of qi trachea and esophagus.shoqχής
Type-V:
- H-type TEF: It is found in about 4 percent of all cases and not usually diagnosed at birth. Both proximal / upper and distal / lower segments of esophagus open into trachea by a fistula. No EA present.
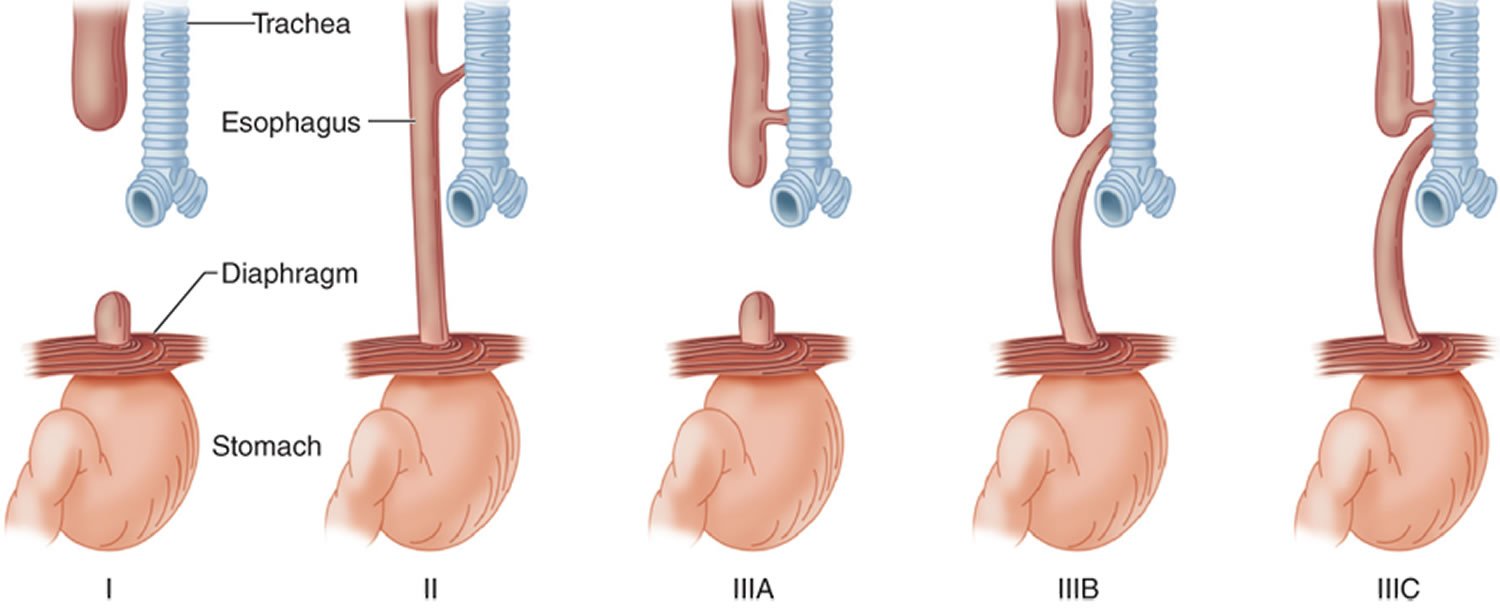
Figure: Esophageal atresia with tracheoesophageal fistula
Management of EA and TEF
Immediate management:
Immediately after diagnosis, the infant should be managed with –
- Propped up position (30° angle) to prevent reflux of gastric secretion.
- Nothing per mouth.
- Airway clearance.
- O₂ therapy.
- IV fluid therapy
- Nasogastric tube aspiration
- The blind pouch to be washed with normal saline to prevent blocking of tube with thick mucus.
- Gastrostomy is done.to decompress the stomach and to prevent aspiration and afterwards to feed the infant
Supportive care should include-
- Maintenance of nutritional requirements and warmth.
- Prevention of infections.
- Antibiotic therapy.
- Respiratory support
- Detection and treatment of complications.
- Continuous monitoring of patients condition
- Chest physiotherapy & postural drainage.
Surgical management
1. The surgical correction of defect is done by end to end anastomosis with excision of the fistula by right posterolateral thoracotomy followed by intercostal chest drainage.
2. This is done when the infant has more than 2 kg body weight and no pneumonia present and the baby is clinically stable.
3. Surgical correction can be done in stages with division of fistula.
4. Other surgical intervention include
- Cervical esophagostomy.
- Esophago-coloplasty
- Esophago-gastroplasty.
Nursing diagnoses about EA & TEF
Preoperative:
- Risk for aspiration related to esophageal abnormality.
- Risk for fluid volume deficit related to inadequate oral intake
- Parental anxiety related to congenital anomalies of the neonate.
Postoperative:
- Ineffective airway clearance related to surgical interventions.
- Altered nutrition, less than body requirements related inadequate oral intake.
- Pain related to surgical interventions.
- Risk for infection related to hospital procedures
- Risk for injury related to complex surgery.
- Impaired tissue integrity related to postoperative drainage.
- Risk for altered parenting related to prolonged illness.
- Knowledge deficit related to home based long-term care.
Nursing interventions of EA & TEF
Preoperative intervention should emphasis on –
- Preventing aspirations by positioning, suctioning and nothing per mouth, thus reducing chance of respiratory infections
- Preventing dehydration by IV fluid, intake and output recording, monitoring of vital signs and child’s general health.
- Preventing infections by infection-control measures.
- Reducing parental anxiety by emotional support.
Postoperative interventions should emphasis on:
- Maintaining clear airway.
- Providing adequate feeding by IV fluid and/or gastrostomy feeding.
- Reducing pain by analgesics and comfort measures.
- Monitoring child’s condition and detecting problems for early interventions
Complications of EA & TEF
1. Death from asphyxia.
2. Pneumonitis secondary to
- Salivary aspiration.
- Gastric acid reflex.
3. Concomitant lesions approximately (40% to 50%)
4. Congenital heart disease.
5. Gl anomalies, particularly imperforated anus.
6. Skeletal and muscular deformities.
7. Renal anomalies.
8. Vertebral defects.
9. Prematurity.
10. Dehydration and electrolyte imbalance.
Tracheoesophageal fistula associated disorders
The existence of other anomalies has been noted in some children with TEF. These areas.
- Laryngeal cleft
- Down syndrome
- Duodenal atresia
- Dysphagia
- Horseshoe kidney
- Polycystic kidney
- Malrotation
- Intestinal malformation
- Rib malformation
- Scoliosis
- Lower limb defect