Caesarean section – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Caesarean section
Caesarean section:
It is an operative procedure whereby the fetus / fetuses are delivered after the end of 28th week through an incision on the abdominal and uterine walls.
[Ref: D. C. Dutta’s Obs/9/545]

Indications of caesarean section:
Absolute indications:
1. Central placenta praevia (Type IV).
2. Contracted pelvis or cephalo-pelvic disproportion (absolute).
3. Pelvic mass causing obstruction (cervical or broad ligament fibroid).
4. Advanced Ca cervix.
5. Vaginal obstruction (atresia, stenosis).
Relative indications:
1. Cephalo-petvic disproportion (relative).
2. Previous caesarean section:
➤ Previous two C/S.
➤ Features of scar dehiscence.
➤ When primary C/S was due to recurrent indication,
3. Fetal distress (non-reassuring FHR).
4. Cervical dystocia- due to
Inefficient uterine contraction..
➤ Small pelvis.
➤ Large fetus.
5. Ante-partum haemorrhage (APH):
➤ Abruptio placenta.
➤Placenta praevia.
6. Mal-presentation:
➤ Brow presentation.
➤ Breech presentation.
➤ Shoulder presentation.
7. Failed surgical induction of labour.
8.Failure to progress in labour.
9.Bad obstetric history (recurrent fetal wastage).
10. Hypertensive disorders:
➤ Eclampsia (uncontrolled fit even with MgSO4 therapy).
➤ Severe pre-eclampsia.
11. Medical disorders:
➤ Heart disease.
➤ Uncontrolled DM.
12. Gynaecological disorders: Mechanical obstruction due to –
➤ Benign or malignant pelvic tumor.
➤Following repair of V.V.F.
[Ref-D. C. Dutta’s Obs/9/546]
Common indication of emergency C/S:
1. CPD.
2. Contracted pelvis.
3. APH/central placenta praevia (type-Iv).
4. Fetal distress.
5. Malpresentations.
6. Failed induction of labour.
7. Cervical dystocia.
[Ref-D. C. Dutta’s Obs/9/546]
Complications of C/S:
1. Maternal complications:
During operation:
1. Uterine laceration.
2. Uterine atony.
3. Extension of uterine incision to one or both sides.
4. Cutting of the uterine vessels leading to-
a. Severe haemorrhage.
b. Hypovolumic shock.
c. Broad ligament hematoma.
5. Primary PPH.
6. Morbid adherent placenta.
7. Injury to the urinary bladder.
8. Injury to the ureter.
9. Anesthetic hazards.
Post-operative complications:
Immediate:
1. Post-operative bleeding.
2. Infection
3. Secondary PPH.
4. Intestinal obstruction.
5. Thrombo-embolic disorder.
6. Septic thrombo-phlebitis.
7. Wound complications:
a. Sanguinous or frank pus.
b. Haematoma formation.
c. Dehiscence (peritoneal coat intact).
d. Burst abdomen (involving the peritoneal coat).
Remote:
1. Gynaecological:
a. Chronic pelvic pain.
b. Backache.
c. Menstrual irregularity.
2. General surgical:
a. Incisional herniae.
b. Intestinal obstruction due to bands & adhesions.
e. Wound dehiscence.
d. Excessive scar formation.
For future pregnancy:
- Risk of scar rupture or rupture of the uterus in the subsequent pregnancies.
2. Fetal complications:
a) Iatrogenic prematurity.
b) Respiratory distress syndrome (RDS).
c) Birth injury.
d) Birth asphyxia due anaesthetic hazards.
[Ref-D. C. Dutta’s Obs/9/551-553]
Lower uterine caesarean section:
When the extraction of the baby is done through an incision made in the lower segment through a trans-peritoneal approach, is called lower segment caesarean section.
[Ref: D. C. Dutta’s Obs/9/547]
Steps of LUCS:
1. Pre-operative procedures:
Please write from below
2. Position: Lithotomy position/supine position.
3. Anaesthesia:
a. Spinal anaesthesia.
b. Epidural anaesthesia.
c. General anaesthesia
4. Anti-septic painting: Mid & lower abdomen from umbilicus to inguinal ligament region including vulva & vagina by 10% chlorohexiidin solution.
5. Draping.
6. Proper light
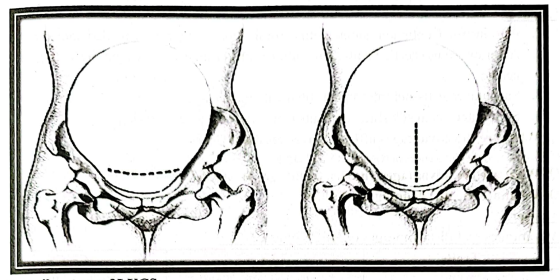
7. Incision: Pfennesteilineision is made commonly 3 cm above the pubic symphysis.
8. Superficial fascia: Fascia of camper & Fascia of scarpa.
9. The recti and pyramidalis muscles are retracted laterally from the midline.
10. Fascia transversalis, extra-peritoneal tissues & parietal peritoneum are divided in a single stroke.
a. The loose peritoneum on the lower segment is cut transversely;
b. A short incision is made in the midline down to the membranes;
c. The incision of the lower segment is being enlarged using index finger of both hands.
11. Delivery of the head.
12. Delivery of the trunk.
13. Removal of the placenta & membranes by CCT.
14. Securing the bleeding vessels properly.
15. Suture of the uterine wound.
Closure:
1. Peritoneum: Continuous suture with chromic 1 or 2 catgut in a rounded bodied needle.
2. Anterior rectus sheath: Continuous suture with chromic 1 or 2 catgut in a cutting bodied needle.
3. Subcutaneous tissue: Interrupted stitch with plain catgut.
4. Skin: Interrupted silk stitches or subcutaneous (cosmetic purpose).
Advantages and disadvantages of LUCS over CUCS:
| Traits | LUCS | CUCS |
| Techniques |
|
|
Postoperative
|
|
|
Wound healing:
|
|
|
|
|
|
| Future pregnancy |
|
|
Pre-operative preparation for elective C/S:
a. History taking:
1. Chief complaints:
2. Period of amenorrhoea& any complaints (if present)
3. History of antenatal checkup.
4. Obstetric history:
a. Menstrual history:
5. H/O significant medical illness.
6. Drug history: Any history of drug hypersensitivity.
7. Immunization history: Status of immunization against tetanus (TT).
b. General examination: Nutrition, pulse rate, blood pressure, temperature, respiratory rate, anaemia, jaundice, cyanosis, oedema, dehydration, heart, lungs, Breast.
c. Systemic examination: CVS & respiratory system examination.
d. Per-abdominal examination:
1. Height of the uterus.
2. Fetal movement.
3. Four grips: Fundal grip, two lateral grip & pelvic grip.
4. Fetal heart rate (FHR).
e. Investigations:
1. Blood routine examination: Hb%, TC, DC, ESR, blood grouping & Rh typing, RBS.
2. Urine R/E: For pus cell, protein.
3. Ultrasonography: To assess fetal wellbeing.
4. ECG
f. Written informed consent.
g. Arrangement for blood transfusion.
h. Arrangement for a neonatologist.
i. Shaving: Shaving of the lower abdomen and vulva, vagin4 perineum & around the anus.
i. Pre-anaesthetic medication:
1. Tab. Diazepam (5mg) at bed time may be prescribed at last night.
2. NPO from 12 hours before operation.
3. An intra-venous cannula (size 18-20) should be opened 2-3 hour before operation.
4. Anti-ulcerant:
- Inj. Pantoprazole (40 mg) should be started to reduce acid secretion.
5. Intra-venous fluid:
- Inf. Hartman’s solution(1000ml): I/V @ 10-15 drops/min 2-3 hours before operation.
- A preload volume of at least 500 ml of Hartman’s solution should be infused just 15 minutes before operation in case of spinal anaesthesia to prevent sudden hypotension.
6. Prophylactic antibiotic: Routine use of prophylactic antibiotic is controversial & varies from obstetrician to obstetrician, but single dose Ceftriaxone I/V is recommended.
5 important steps of preparing a patient:
➤ History taking, clinical examination.
➤ Written informed consent.
➤ NPO for at least 6 hours.
➤ Shaving & cleaning the operation area.
➤ Opening of an intravenous channel before operation.
Operation note:
Date: 20/10/2017
Name of the operation: Lower uterine segment caesarean section (lucs),
Indication: Primigravida with 40 weeks pregnancy with CPD.
Anaesthesia: Spinal
Procedure:
With all aseptic precautions, the abdomen was opened by Pfannesteil incision & reached in the pelvic cavity traditionally. Lower uterine transverse incision is made & was reached in the uterine cavity. A male, healthy baby was delivered. Placenta, cord & membranes were delivered by control cord traction (CCT). Bleeding was average &. after proper haemostasis, abdomen was closed in layers.
Surgeon: Prof. X
Assistant:
15: Dr. Y
2nd: Dr. Z
Anaesthesiologist: Dr. A
Baby note:
➤ Sex: Male
➤ Weight: 3.2 kg
➤ APGAR score: 10/10 in 1 minute and 10/10 in 5 minute.
➤ Congenital anomaly: Absent
1. NPO till further order..
2. Inf. 5% DNS (2L) + Inf. Hartman’s solution (IL) + Inj. Oxytocin (2 amp in each litre of fluid).
3. I/V @ 30 drops/min.
4. Inj. Ceftriaxone (1gm): 1 vial I/V stat & daily.
5. Inj. Metronidazole (500 mg): 1 bottle I/V stat & 8 hourly.
6. Inj. Pethidine (100 mg): 1 amp I/M stat and SOS.
7. Inj. Metoclopramide (12.5 mg): 1 amp I/M stat (15 minutes before pethidine).
8. Inj. Tramadol (100 mg): 1 amp I/M 12 hourly.
9. Inj. Ranitidine (50 mg): 1 amp I/V stat & 8 hourly.
10. Diclofenac suppository (50 mg) 1 stick per-rectally SOS.
11. Continue catheter for 3 days (if obstructed labour then 21 days).
12. Change of posture at two hours interval & messaging in the dependent part of the body to prevent bed sores.
13. Please monitor the vital signs of the patient routinely.
‘0’ POD:
1. Follow the postoperative order.
2. Effective pain management.
3. Examination of the dressing.
4. Routine vital signs monitoring:
- Pulse
- B.P
- Temp
- Resp. rate
5.Urine output monitoring.
6. Auscultation of the abdomen for bowel sound.
1st POD:
1. I/V fluid continue with sips of water orally.
2. Early mobilization.
3. Monitoring of vital signs as before.
4. Checking the bandage.
2th POD:
1. If bowel sound present then liquid diet followed by semi-solid food.
2. I/V Fluid reduced to IL.
3. Antibiotics are given in oral form.
4. Catheter should be clamped.
5. Mobilization continue.
6. Monitoring of vital signs as before.
3rd POD:
1. If no problem then diet is regular high protein and high fiber diet.
2. I/V Fluid is withdrawn.
3. Catheter is withdrawn.
4. Checking the bandage.
5. Monitoring of vital signs as before.
4th POD:
1. Dressing is done.
2. Monitoring of vital signs as before.
5th POD:
1. Continue the same.
6th POD:
1. If wound is healthy alternate stitch may be off.
2. Continue the same.
7th POD:
1. Complete removal of stitch.
2. Discharge the patient with advice.

Discharge note following a C/S:
1. Diet: High nutritious diet containing high class protein, vitamins, minerals, fiber etc.
2.Breast feeding:
- Absolute/Exclusive breast feeding for 1″ 6 months.
- Extra supplementary food for next 1 and half year with breast feeding.
3.Contraception:
- Progesterone only pill for 16 months.
- Barrier method for next 1 year.
4. Coitus:
- Abstinence for 13 months.
- With caution for next 3 months.
5. Immunization:
- Immunized the baby according to EPI schedule.
6. Birth spacing: At least for 2 years
7. Personal cautions:
- Do not bear heavy weight for 6 months.
- Do not strain during defecation.
- Wear abdominal binders for 3 months.