Genital Prolapse – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Genital Prolapse
Genital prolapse:
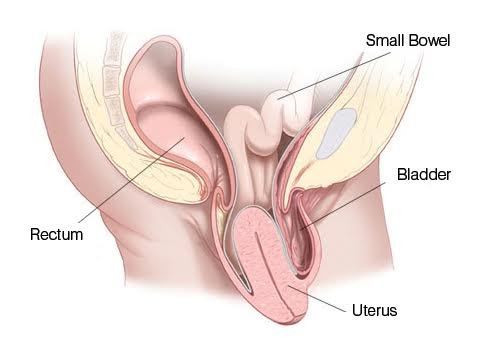
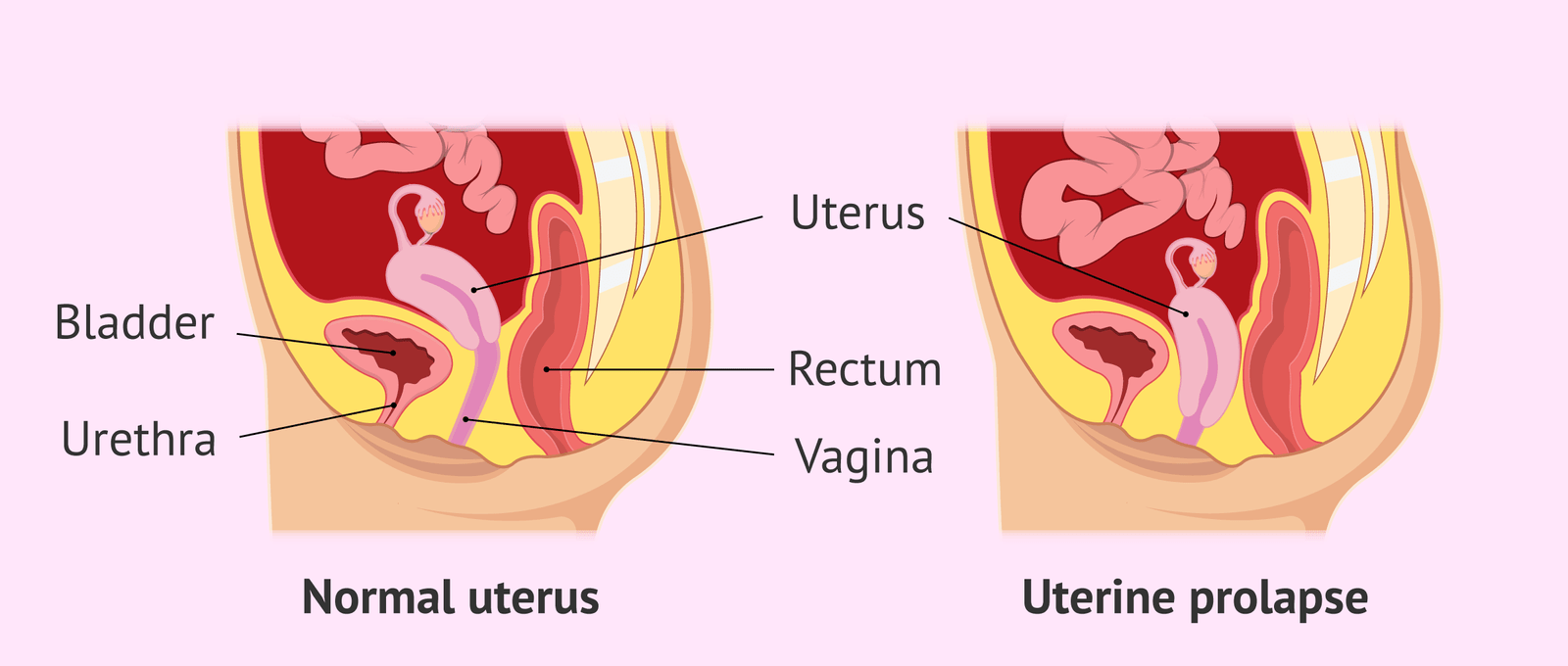
Descent of the pelvic organs (e,g uterus and vagina) from its normal position in the pelvis through the vagina is known as genital prolapse.
Types of genital prolapse:
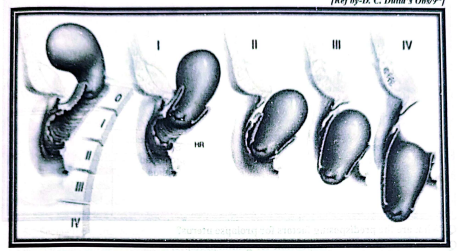
1. Uterine prolapse:
Uterine descend is always associated with vaginal descend. So it is also called utero-vaginal prolapse.
A. 1st degree: Slight descent of the uterus (cervix below the level ofischial spine/ external os) but the cervix remains within vagina or introitus.
B. 2nd degree: Descent of the uterus to that extent that the cervix projects at or outside the
introitus with or without straining
C. 3rd degree: The whole uterus prolapse outside the introitus. This is also called procidentia.
[Nice to learn:
1°= Cx crosses the external os, but uterus remains in vagina or introitus.
20- Cx crosses the introitus but not the whole part of uterus.
3º The whole uterus crosses outside the uterus.]
2. Vaginal prolapse:
Vaginal wall can be prolapsed in absence of uterine descend. Vaginal prolapse may involve prolapse of its anterior wall, posterior wall or both. Nomenclature is given according to the underlying structures involved.
A. Anterior vaginal wall prolapse:
a) Cystocele: When the upper part of the anterior vaginal wall descends along with the base ofthe bladder, the condition is called cystocele. Weakening of the pubo-cervical fascia gives rise to the development of cystocele
b) Urethrocele: When the lower part descends along with the urethra, it is called urethrocele. Due to damage to the triangular ligament, the urethra is displaced backwards & downwards from its normal position of subpubic angle.
c) Cysto-urethrocele
B. Posterior vaginal wall prolapse:
a) Enterocele: Upper part of the posterior vaginal wall descends along with the pouch of Douglas. As the pouch usually contains coils of intestine, the condition is called enterocele. Correction of herniation of pouch is essential, even if not associated with obvious enterocele, because, there will be vault prolapse following hysterectomy.
b) Rectocele: Descend of the middle portion of the posterior vaginal wall along with the anteriorwall of rectum, is known as rectocele. This condition develops due to weakening of the rectovaginal fascia.
Lower third of the posterior vaginal wall becomes lax due to damage of the perineal body.
[Ref by-D. C. Dutta’s Obs/9th]
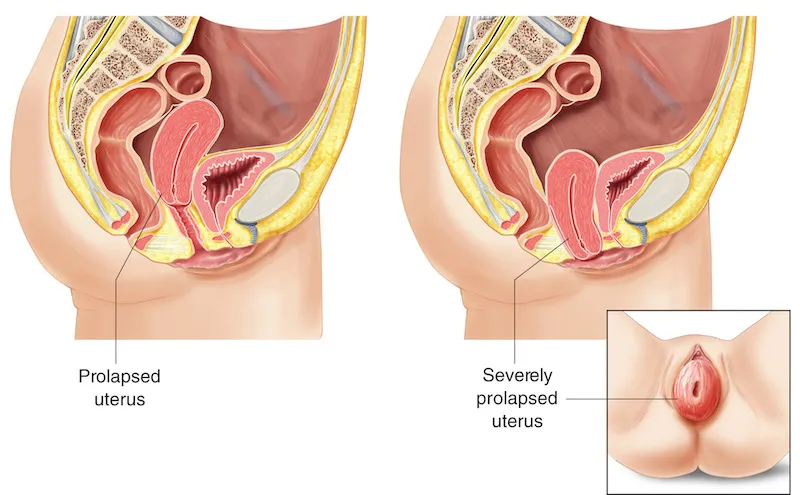
Uterine prolapse:
Uterine prolapse occurs when the uterus sags or slips from its normal position and into the vagina, or birth canal.
Factors responsible for genital prolapse:
Anatomical factor:
➤ Gravitational stress due to human bipedal posture.
➤ Anterior inclination of pelvis directing the force more anteriorly.
➤ Stress of parturiation (Intemal rotation) causing damage maximum on puborectal fibers of levatorani.
➤ Pelvic floor weakness due to urogmital hiatus and the direction of obstetric axis through the hiatus.
➤ Inherent weakness of the supporting structures.
Clinical:
Predisposing factors:
Acquired:
➤ Ligaments
➤ Endopelvic fascia
➤ Levatorani muscle
➤ Perinealbody.
➤ Neuromuscular damage due to repeated childbirth.
Congenital:
➤ Inherent weakness of the supporting structures
Aggravating factors:
➤ Post merropausal atrophy.
➤ Poor collagen tissue repair with age.
➤ Increased intra-abdominal pressure as in’ chronic cough and constipation
➤ Asthenia and under nutrition.
➤ Obesity.
➤ Increased weight of the uterus as in fibroid or myohyperplasia
[Ref by-D. C. Dutta’s Obs/9/th]
Signs and symptoms of uterine prolapse:
Women who have a minor uterine prolapse may not have any symptoms. Moderate to severe prolapse may cause symptoms, such as:
1. Feeling like sitting on a ball.
2. Vaginal bleedin.girls
3. Increaseddischarge.
4. Problems with sexual intercourse.
5. Seeing the uterus or cervix coming out of the vagina.
6. A pulling or heavy feeling in the pelvis.
7. Constipation.
8. Recurrent bladder infections.
Genital prolapse is common in Bangladesh due to following reasons:
➤ Multiparity and repeated childbirth: 95% cases present with genital prolapse ismulltiparous.
➤ Mismanagement of 2nd & 3rd stage of labor.
➤ Bearing down before full dilatation of cervix.
➤ Application of forcep and ventous before full cervical dilatation.
➤ Downward pressure over fundus during attempts of placenta delivery. Prolonged and difficult labor.
➤ Rigid perineum with improper episiotomy.
➤ Improper postnatal care.
➤ Surgical injury- D& C, Sub-total abdominal hysterectomy, abdomino – perineal operations.
➤ Manopause: Withdrawal of hormones cause atrophy ana weakness of ligament.
Other precipitating factors include:
➤ Increased intra-abdominal pressure due to chronic cough, chronic constipation, chronic retention of urine, ascites, heavy weight lifting, tumor etc.
➤ Increased weight of uterus due to sub-involution, small tumor, myohyperplasia.
➤ Traction of uterus by vaginal prolapse, large cervical polyp.
➤ General condition Malnutrition, asthenia etc.
Mismanagement of 2nd & 3rd stage of labor:
➤ Bearing down before full dilatation of cervix.
➤ Application of forcep and ventous before full cervical dilatation.
➤Downward pressure over fundus during attempts of placenta delivery.
➤ Prolonged and difficult labor.
➤ Rigid perineum with improper episiotomy.
Prevention of genital prolapse:
Family planning & family spacing as well as conducted labor by trained birth attendant.
A. During labour:
➤ Avoid prolonged 2nd stage of labor by necessary steps like- Episiotomy, Forceps Vacuum extraction wherever required.
➤ Avoid delivery prior to full dilatation of cervix.
➤ Proper repair of all tear & lacerations carefully in layers after delivery.
➤ Avoid downward pressure over fundus during attempts of placental delivery.
B. During puerperium:
➤ Early ambulation.
➤ Exercise.
➤ Perineal exercise- contraction and relaxation of levatorani.
➤ Lying down in prone position.
➤ Correction of puerperal retroversion.
➤ Treatment of constipation.
➤ Early evacuation of bladder.
➤ General improvement of health.
➤ Prevention of early resumption of work.
C. At hysterectomy:
Abdominal hysterectomy (Fothergil’s operation)-
➤ Stumps of round ligament, utero-sacral ligament, and transverse cervical ligament are fixed with vaginal vault.
➤ Vaginal wall is closed from side to side instead of from front to back.
Vaginal hysterectomy –
➤ Excision of redundant peritoneum.
➤ Tightening of the cardinal, utero-sacral ligament and their inclusion in the vaginal vault.
Management:
Diagnosis:
Pt. profile: Usually multiparous, elderly around 50 years.
A.C/F:
Symptoms:
a) Vaginal bleeding.
b) Increased discharge.
c) Problems with sexual intercourse.
d) A pulling or heavy feeling in the pelvis.
e) Constipation.
f) Recurrent bladder infections.
Signs:
a) General exam: No abnormality detected.
b) Abdominal exam: No abnormality detected.
c) Vaginal examination: Feeling of descent cervix on straining.
d) Speculum exam: Cervix descent below the ischial spines on straining.
B. Investigations:
➤ Blood for Hb%, TC, DC, ESR.
➤ Blood grouping & cross matching.
➤ Blood sugar.
➤ Blood urea & Serum creatinine.
➤ Urine R/M/E.
➤ X ray chest P/A view.
➤ ECG (if age > 40 years).
Treatment:
General Rx:
➤ Rx of UTI.
➤ Rx of decubitus ulcer.
➤ Rx of atrophied & senile vaginitis with oestrogen therapy.
Specific Rx:
1. In case of a woman of 60 years with prolapse:
Vaginal hysterectomy with pelvic floor repair (Anterior colporrhaphy& posterior colpoperineorrhaphy)
3. In case of a woman of<40 years with prolapse:
4. If family is complete: Fothergill’s operation with tubectomy. If family is incomplete: Fothernill’s operation.
Post-operative Rx:
➤ Continuous catheterization for 5 days.
➤ Ring pessary/vaginal pack for 24 hrs.
➤ Abstinence for 2 months.
➤ No heavy work for 6 months
➤ Antibiotics.
[Ref by-D. C. Dutta’s Obs/9th]
Management:
Diagnosis:
A. C/F:
a. Symptoms:
1. Something coming down per vagina.
2. Heaviness in lower abdomen & vagina.
3. Frequency, difficult and incomplete voiding. (-> dysuria due to ch. retention of urine -> UTI)
4. Difficult defaecation.
5. Backache
6. Vaginal discharge which may be sometimes blood stained, (decubitus ulcer).
b. Signs:
1. General exam: No abriorrnality detected.
2. Abdominal exam: No abnormality detected.
3. Vaginal examination:
Inspection
1. Cervix is outside the introitus and is congested. Decubitus ulcer may be a
2. Vulvular atrophy.
3. Cystocele & rectocele may be present.
4. Stress incontinence or coughing -> urine comes out.
Palpation:
1. At the introitus, cervix is felt in between the anterior and posterior vaginal walls.
2. Get above the swelling: +ve in 3º and -ve in 20
Bimanual examination:
1. Uterus is normal in size, mobile and the fornices are free. No mass.
2. No adnexal mass.
Per speculum exam: Mass is reduced,
1. Retract the post, vaginal wall by Sim’s speculum, Pt. cough
- Upper ant. wall bulge ->
- cystocele Lower ant, wall
- bulge urethrocele
2. Retract the ant. vaginal wall by Sim’s speculum. Pt. cough-
- Upper part bulge ->enterocele
- Lower part bulge > rectocele:
- Rectocele is present.
Investigations: For pre-operative assessment-
➤ Blood for Hb%, TC, DC, ESR.
➤ Blood grouping & cross matching.
➤ Blood sugar.
➤ Blood urea & Serum creatinine.
➤ Urine R/M/E.
➤ X ray chest P/A.view.
➤ ECG (if age > 40 years)
Treatment:
General Rx:
➤ Rx of UTI
➤ Rx of decubitus ulcer.
➤ Rx of atrophied & senile vaginitis with oestrogen therapy.
Specific Rx:
1. In case of a woman of 60 years with prolapse: Vaginal hysterectomy with pelvic floor repair (Anterior colporrhaphy & posterior colpoperineorrhaphy).
2. In case of a woman of<40 years with prolapse: If family is complete: Fothergill’s operation with tubectomy. If family is incomplete: Fothernill’s operation.
Post-operative Rx:
➤ Continuous catheterization for 5 days.
➤ Ring pessary/vaginal pack for 24 hrs.
➤ Abstinence for 2 months.
➤ No heavy work for 6 months
➤ Antibiotics.
[Ref by-D. C. Dutta’s Obs/9]
Management:
Diagnosis:
Symptoms: See above.
➤ General exam: No abnormality detected.
➤ Abdominal exam: No abnormality detected.
Vaginal examination:
1. A mass is protruded from the vaginal introitus.
2. A thumb is placed anteriorly and the fingers posteriorly above the mass outside the introitus are apposed.
3. Vagina becomes thickened, corrugated & white with keratin.
4. Ulceration in the prolapsed uterus.
C. Investigations: See above.
D. Treatment: See above.
D/D of genital prolapse:
1. Congenital elongation of cervix.
2. Any growth in cervix or vagina:. Gartner’s cyst, Myomatous polyp.
3. Chronic uterine inversion.
[Nice to know:
(Congenital elongation of cervix: Vaginal part is elongated. Fornix is deep. Rx: Amputation of cervix.]
Different Rx options of uro-genital prolapse:
In case of a woman of 60 years with prolapse: Vaginal hysterectomy with pelvic floor repair
(Anterior colporrhaphy posterior colpoperineorrhaphy)
If only cystocele (Only anterior colporrhaphy Rectocele (Posterior colpoperineorrhaphy)
Treatment of genital prolapse in post-menopausal patients:
Vaginal hysterectomy with pelvic floor repair (Anterior colporrhaphy & posterior colpoperineorrhaphy).
Treatment of utero-vaginal prolapse at 35 vrs of age:
➤ If family is complete: Fothergill’s operation with tubectomy. If family is incomplete: Fothergill’s operation.
a. Elongated cervix is associated with lengthening of the portio vaginalis. (vaginal portion of Cx is elongated).
b. There will be no associated uterine descend.
c. Vaginal fornices will be deep & narrow.
d. There will be no laxity of the vaginal wall.
e. There will be increase in utero-cervical canal as evidenced by uterine sound.
Complications of genital prolapse:
1. Keratinization of the vagina: Prolapsed vaginal wall constantly exposed to the air & possibly to trauma, becomes thickened, corrugated & white with keratin.
2. Decubitus ulceration.
3. Hypertrophy of cervix: Elongation of the supra-vaginal cervix, congestion & edema, glandular hypertrophy.
4. Obstructive lesions of the urinary tract: Bladder hypertrophy &trabeculation, hydro-ureter, hydro-nephrosis.
a) Renal failure. Residual urine -> cystitis ->> ascending infection, pyelitis & pyelonephritis ->>renal failure.
b) Incarceration of the prolapse (irreducible).
c) Ca cervix or vagina rarely develops on decubitus ulcer.
d) Peritonitis.
[Ref by-D. C. Dutta’s Obs/9th]
