Postpartum Depression – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.

Postpartum Depression
Postpartum depression
Postpartum depression is a mood disorder that can affect women after childbirth. Mothers with postpartum depression experience feelings of extreme sadness, anxiety, and exhaustion that may make it difficult for them to complete daily care activities for themselves or for others.
There’s no single cause of postpartum depression, but physical and emotional issues may play a role.
1. Physical changes. After childbirth, a dramatic drop in hormones (estrogen and progesterone) in the body may contribute to postpartum depression. Other hormones produced by thyroid gland also may drop sharply which can leave feeling tired, sluggish and depressed.
2. Emotional issues. When sleep deprived and overwhelmed, it may have trouble handling even minor problems. It may be anxious about the ability to care for a newborn. It may feel less attractive, struggle with the sense of identity or feel that lost control over life. Any of these issues can contribute to postpartum depression.
Risk factors of postpartum depression
Postpartum depression can develop after the birth of any child, not just the first. The risk increases if:
- Depression or anxiety during pregnancy.
- Stressful life events during pregnancy or soon after giving birth.
- Traumatic childbirth experience.
- Preterm delivery.
- A baby needing neonatal intensive care.
- Lack of social support.
- Previous history of depression.
- Breastfeeding problems.
Other risk factors include:
- Baby blues after delivery.
- Unplanned or unwanted pregnancy.
- A baby with birth defects or other medical problems.
- Multiple babies (such as twins or triplets).
- Family history of psychiatric problems.
- Being single.
- Low socioeconomic status or financial instability.
- Domestic violence.
- Unemployment.
- Many medical appointments during pregnancy.
- Pregestational or gestational diabetes.
Or (Another answer)
While the causes of PPD are not understood, a number of factors have been suggested to increase the risk:
- Prenatal depression or anxiety.
- A personal or family history of depression.
- Moderate to severe premenstrual symptoms.
- Maternity blues.
- Birth-related psychological trauma.
- Birth-related physical trauma.
- Previous stillbirth or miscarriage.
- Formula-feeding rather than breast-feeding
- Cigarette smoking.
- Low self-esteem.
- Childcare or life stress.
- Low social support.
- Poor marital relationship or single marital status.
- Low socioeconomic status.
- Infant temperament problems/colic.
- Unplanned/unwanted pregnancy,
- Elevated prolactin levels.
- Oxytocin depletion.
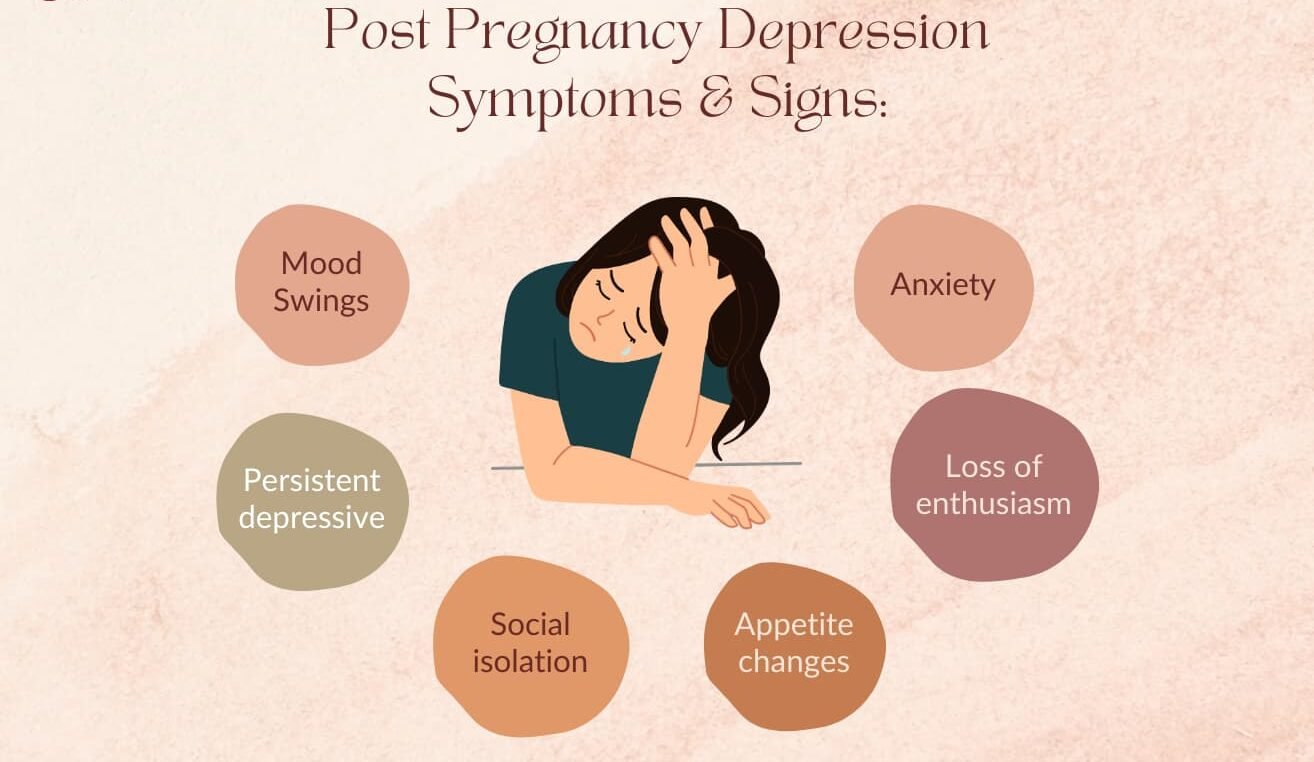
Postpartum depression symptoms
Some of the more common symptoms a woman may experience include:
Emotional:
- Persistent sadness, anxiousness or “empty” mood.
- Severe mood swings.
- Frustration, irritability, restlessness, anger.
- Feelings of hopelessness or helplessness.
- Guilt, shame, worthlessness.
- Low self-esteem.
- Numbness, emptiness.
- Exhaustion.
- Inability to be comforted.
- Trouble bonding with the baby.
- Feeling inadequate in taking care of the baby.
Behavioral:
- Lack of interest or pleasure in usual activities.
- Low or no energy.
- Low libido,
- Changes in appetite.
- Fatigue, decreased energy and motivation.
- Poor self-care.
- Social withdrawal.
- Insomnia or excessive sleep.
Cognition:
- Diminished ability to make decisions and think clearly.
- Lack of concentration and poor memory.
- Fear that you cannot care for the baby or fear of the baby.
- Worry about harming self, baby, or partner
General Measures
- Get as much rest as you can.
- Accept help from family and friends.
- Connect with other new moms.
- Create time to take care of yourself.
- Avoid alcohol and recreational drugs, which can make mood swings worse.
There are effective treatments for postpartum depression. A woman’s health care provider can help her choose the best treatment, which may include: Postpartum depression is often treated with psychotherapy (also called talk therapy or mental health counseling), medication or both.
A. Psychotherapy: It may help to talk through your concerns with a psychiatrist, psychologist or other mental health provider. Through therapy, you can find better ways to cope with your feelings, solve problems, set realistic goals and respond to situations in a positive way. Sometimes family or relationship therapy also helps.
B.Counseling/Talk Therapy: This treatment involves talking one-on-one with a mental health professional (a counselor, therapist, psychologist, psychiatrist, or social worker). Two types of counseling shown to be particularly effective in treating postpartum depression are:
- Cognitive behavioral therapy (CBT), which helps people recognize and change their negative thoughts and behaviors; and
- Interpersonal therapy (IPT), which helps people understand and work through problematic personal relationships.
C. Antidepressants: Doctor may recommend an antidepressant. If breast-feeding, any medication that can take will enter breast milk. However, some antidepressants can be used during breast-feeding with little risk of side effects for baby. Work with doctor to weigh the potential risks and benefits of specific antidepressants.
With appropriate treatment, postpartum depression usually goes away within six months. In some cases, postpartum depression lasts much longer, becoming chronic depression. It’s important to continue treatment after you begin to feel better. Stopping treatment too early may lead to a relapse.
D. Lifestyle and home remedies: Postpartum depression isn’t generally a condition that can treat on own things for that build on a treatment plan and help speed recovery,
- Make healthy lifestyle choices: Try to get adequate rest. Eat healthy foods and avoid alcohol
- Set realistic expectations: Don’t pressure to do everything. Scale back expectations for the perfect household.
- Make time for self.
- Avoid isolation: Talk with partner, family and friends about how are feeling. Ask other mothers about their experiences. Breaking the isolation may help feel human again.
- Ask for help