Today our topic of discussion is ” Metabolic States of the Body “. The human body is a marvel of biological engineering, constantly navigating a complex series of metabolic states to sustain life. These metabolic states are defined by the balance between energy intake and energy expenditure, influenced by factors such as nutrient availability, physical activity, hormonal regulation, and genetic makeup.
The interplay between these states and our nutrition forms the essence of metabolic flexibility — the body’s ability to switch between fuel sources based on demand and supply. This article delves into the various metabolic states, their physiological significance, and the nutritional considerations that underpin optimal health.
Metabolic States of the Body : Metabolism and Nutrition
1. Fed State Metabolism (The Anabolic Window)
Energy Abundance and Nutrient Processing
After eating, the body enters a nutrient-rich phase, often termed the “fed state” or “postprandial state,” which can last for several hours. During this time, insulin secretion is stimulated by elevated blood glucose levels, orchestrating the uptake and storage of nutrients.
Carbohydrate Metabolism
Glucose from carbohydrates is the primary source of energy. Excess glucose is stored as glycogen in the liver and muscles or converted to fat.
Protein Metabolism
Dietary proteins are broken down into amino acids, which are then used for protein synthesis, supporting the growth and repair of tissues.
Lipid Metabolism
Dietary fats are primarily stored in adipose tissue. However, a portion is utilized for immediate energy production through β-oxidation or incorporated into cellular structures.
Nutritional Implications
Optimizing nutrient intake during the fed state can bolster anabolism, improve recovery, and support overall metabolic health. This involves consuming a balanced meal with an appropriate ratio of macronutrients.
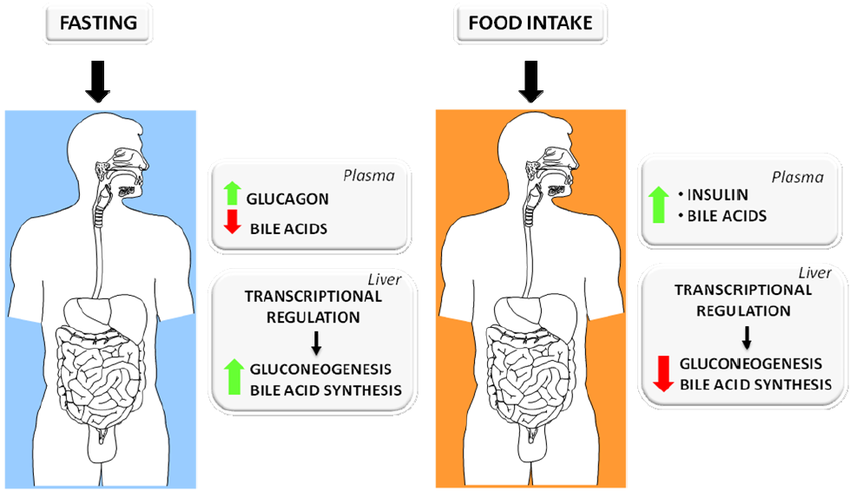
2. Fasted State Metabolism (The Catabolic Phase)
Energy Conservation and Mobilization
Several hours after eating, insulin levels decrease, and the body transitions into the “fasted state,” characterized by the mobilization of stored energy to maintain bodily functions.
Glycogenolysis
The liver breaks down glycogen into glucose, releasing it into the bloodstream to maintain blood glucose levels.
Gluconeogenesis
When glycogen stores are depleted, the liver synthesizes new glucose from non-carbohydrate sources, such as amino acids and glycerol.
Lipolysis
Stored triglycerides in adipose tissue are broken down into free fatty acids (FFAs) and glycerol, which serve as alternative energy sources.
Nutritional Implications
During fasting, maintaining muscle mass and overall metabolic health is critical. Amino acid availability and the consumption of medium-chain triglycerides (MCTs) can influence the body’s metabolic response.
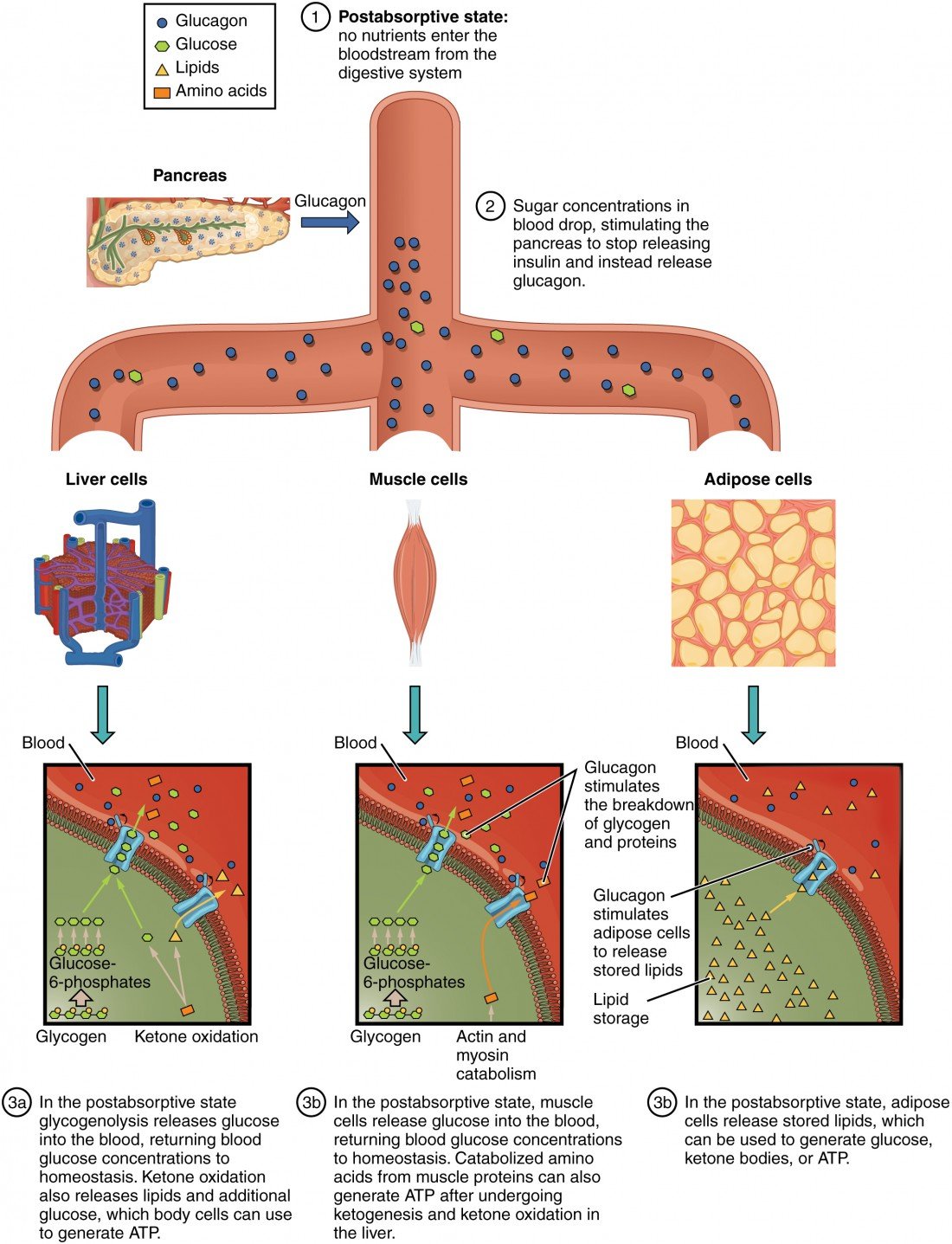
3. Post-Absorptive State (The Transition Phase)
Balancing Nutrient Release and Utilization
The post-absorptive state, occurring 4 to 6 hours after a meal, is a transitional phase where the body begins to rely more on internal stores of energy.
Shift to Endogenous Energy Sources
The gradual shift from insulin to glucagon dominance prompts the use of internal energy reserves, with a minor increase in catabolic activities to maintain energy balance.

Nutritional Implications
The quality of the preceding meal can impact how smoothly the body transitions into using stored energy. Foods with a low glycemic index and high in fiber can promote sustained energy release.
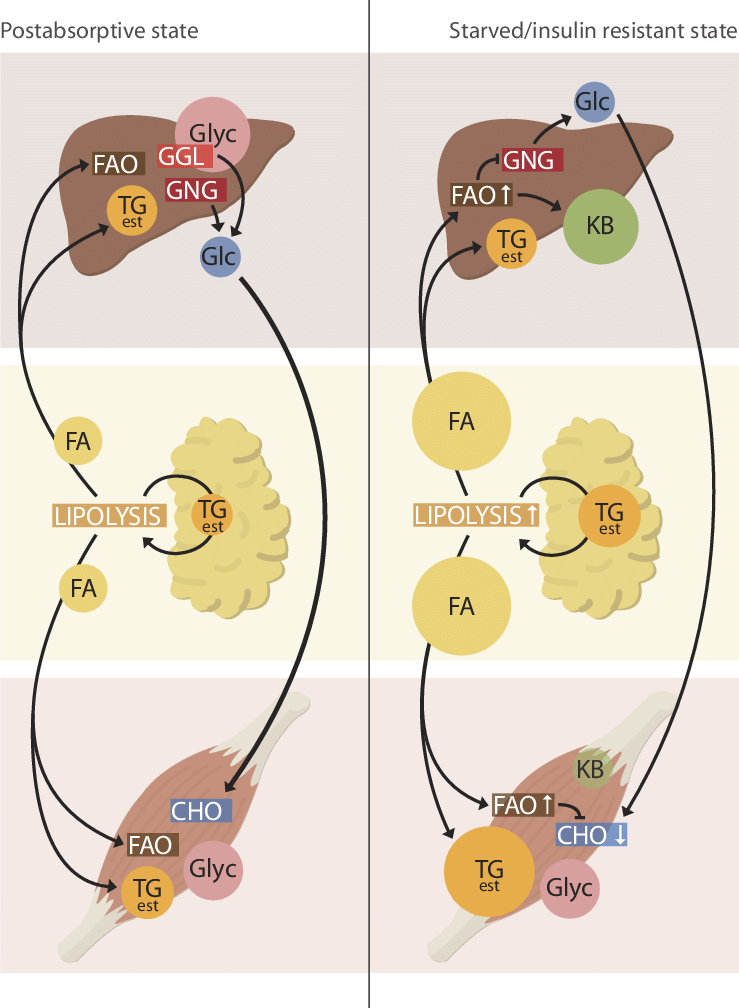
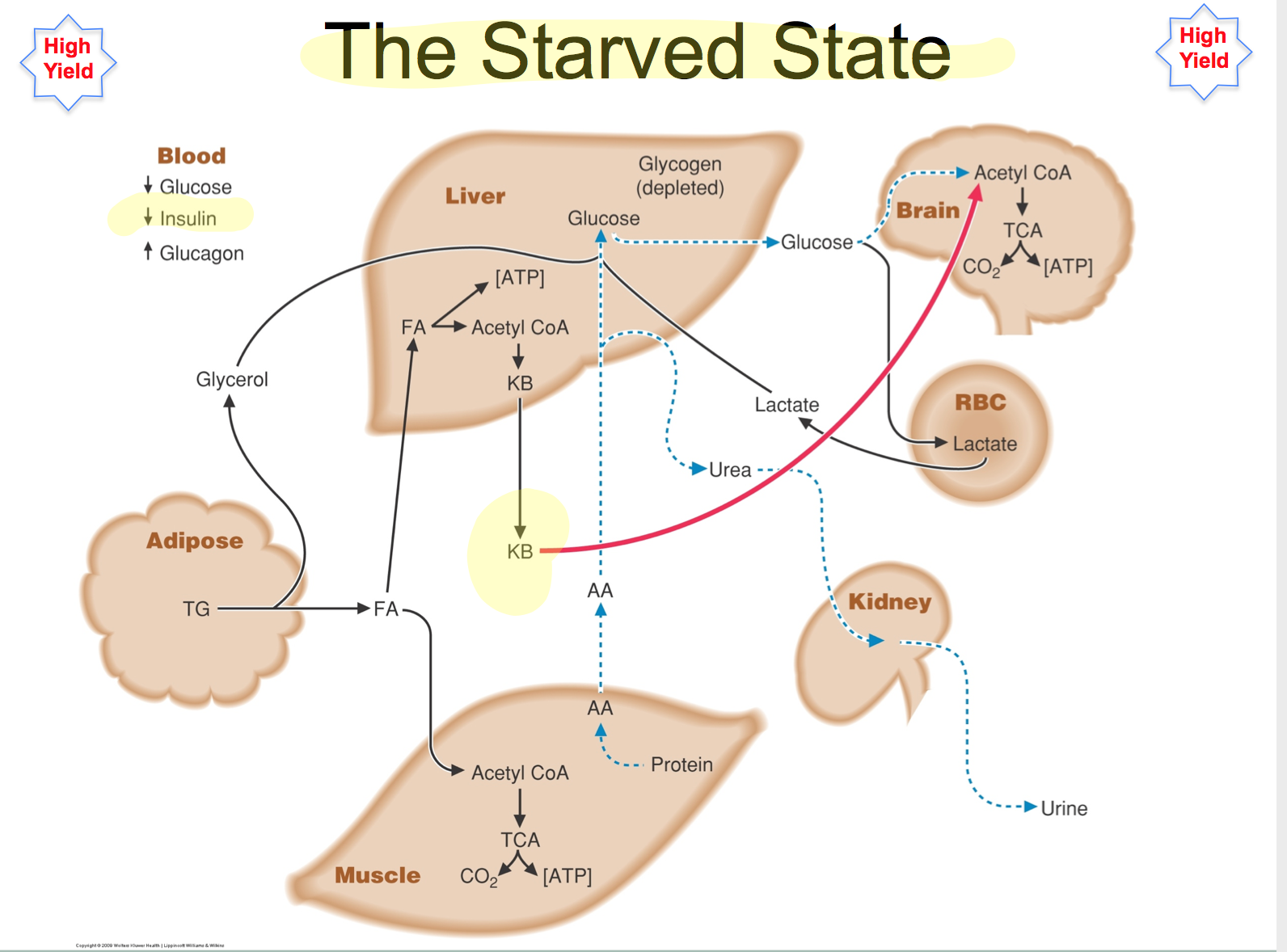
4. Starvation State Metabolism (Adaptation and Survival)
Prolonged Energy Deprivation
Extended periods of food deprivation push the body further into a starvation state, triggering more profound metabolic adaptations to conserve energy and protect vital tissues.
Ketogenesis
As the starvation state progresses, the liver increases ketone body production, providing an essential energy source for the brain and other tissues.
Protein Conservation
The body reduces its reliance on protein catabolism for gluconeogenesis, preserving muscle mass and vital proteins.
Nutritional Implications
Refeeding after a period of starvation requires careful nutritional management to avoid refeeding syndrome and ensure the restoration of normal metabolic functions.
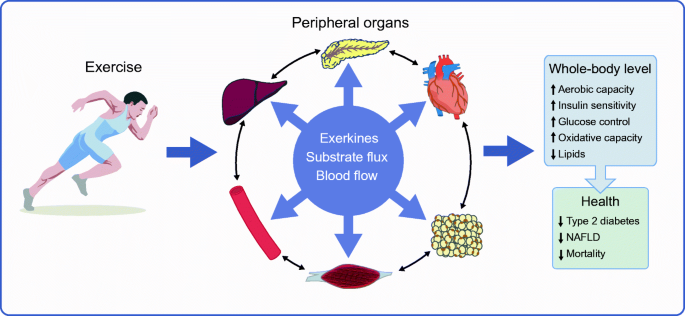
5. Exercise-Induced Metabolic State (The Active Shift)
Increased Energy Demand and Utilization
Physical activity significantly increases energy expenditure, inducing a unique metabolic state where carbohydrate and fat utilization is enhanced.
Energy Systems During Exercise
The body recruits different energy systems based on exercise intensity and duration, ranging from immediate phosphagen use to aerobic oxidative metabolism.
Nutritional Implications
Nutrition plays a pivotal role in exercise performance and recovery. Strategic intake of carbohydrates, proteins, and hydration before, during, and after exercise can enhance metabolic responses to training.
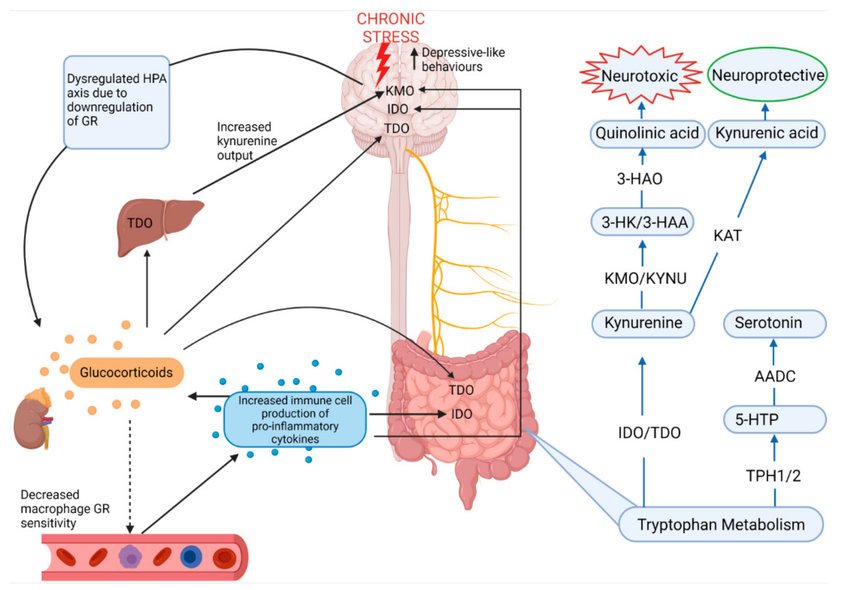
6. Stress-Induced Metabolic State (The Hormonal Flare)
The Metabolic Response to Stress
Acute or chronic stress induces hormonal changes, particularly in cortisol levels, that influence energy metabolism, often leading to increased gluconeogenesis and protein catabolism.
Nutritional Implications
Adequate nutrition can help modulate the body’s stress response, emphasizing the need for a balanced diet rich in antioxidants, omega-3 fatty acids, and other nutrients that support the body’s adaptation mechanisms.
Conclusion
The body’s metabolic states are a reflection of a complex biological interplay between nutrition intake, energy demands, and environmental factors. Understanding these states not only illuminates the science behind energy utilization and storage but also underscores the importance of nutrition in shaping metabolic health. The mastery of nutritional strategies to complement each metabolic state can foster enhanced health outcomes, improved performance, and a deeper understanding of the body’s remarkable metabolic flexibility.
Read more:
