Today our topic of discussion is ” Endocrine Regulation of Kidney Function “. The human urinary system, also known as the renal system, is a sophisticated filtration apparatus responsible for the removal of waste products and excess substances from the bloodstream, thereby maintaining the body’s fluid, electrolyte balance, and blood pressure. It comprises the kidneys, ureters, bladder, and urethra.
The kidneys, being the primary organs, not only filter blood to produce urine but also perform vital functions that include regulation of electrolytes, maintenance of acid-base balance, and regulation of blood pressure. The endocrine system, through a series of hormone-driven interactions, plays a crucial role in managing these functions. This article delves into the endocrine regulation of kidney function, exploring the hormones involved, their mechanisms of action, and the implications of this regulation on overall health.
Endocrine Regulation of Kidney Function : The Urinary System
Hormonal Control of Kidney Function
Several hormones are integral to the kidney’s ability to maintain homeostasis, including antidiuretic hormone (ADH), aldosterone, atrial natriuretic peptide (ANP), and the renin-angiotensin-aldosterone system (RAAS).
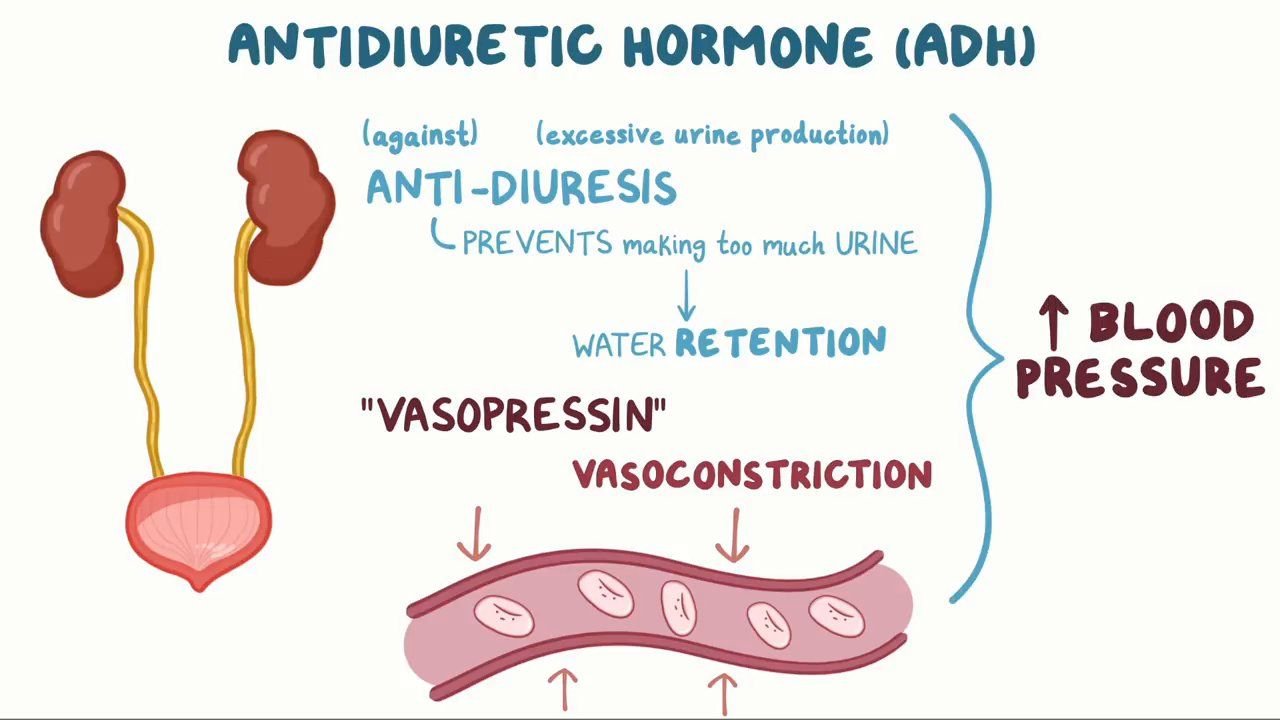
Antidiuretic Hormone (ADH)
Produced in the hypothalamus and released from the posterior pituitary gland, ADH, also known as vasopressin, is essential for water balance. It regulates the amount of water excreted by the kidneys by increasing the permeability of the collecting ducts to water, thereby allowing more water to be reabsorbed back into the bloodstream.
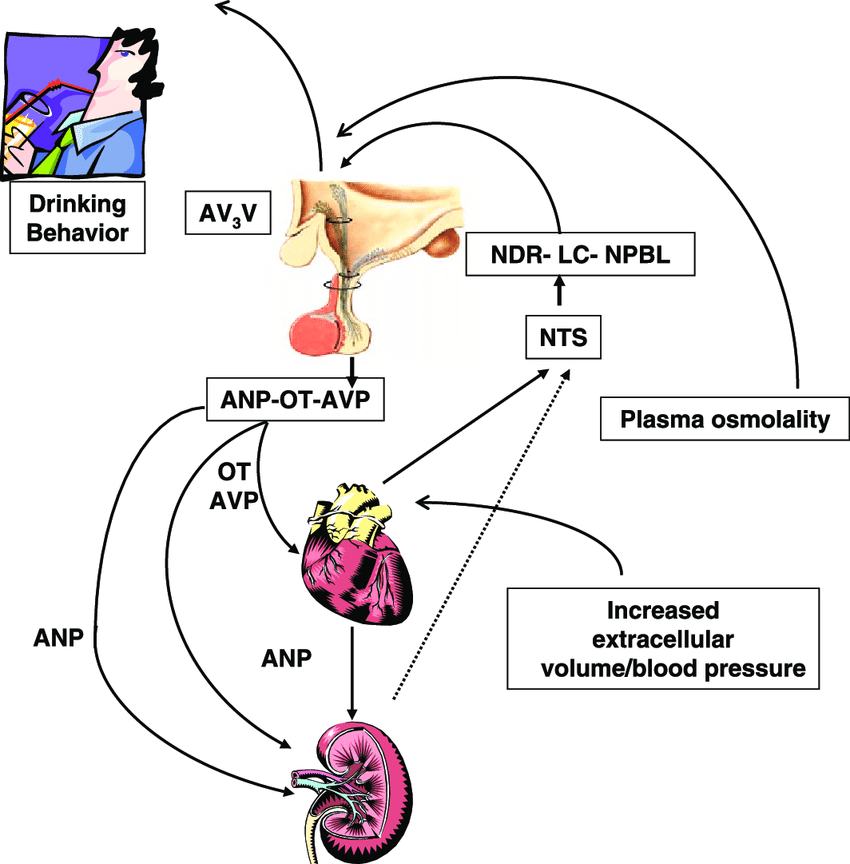
ADH secretion is triggered by increased plasma osmolality (a concentration of solutes in the blood) or decreased blood volume, as sensed by osmoreceptors in the hypothalamus and baroreceptors in the cardiovascular system. When water is conserved, urine becomes more concentrated. Conversely, with decreased ADH, urine becomes diluted, and more water is excreted.
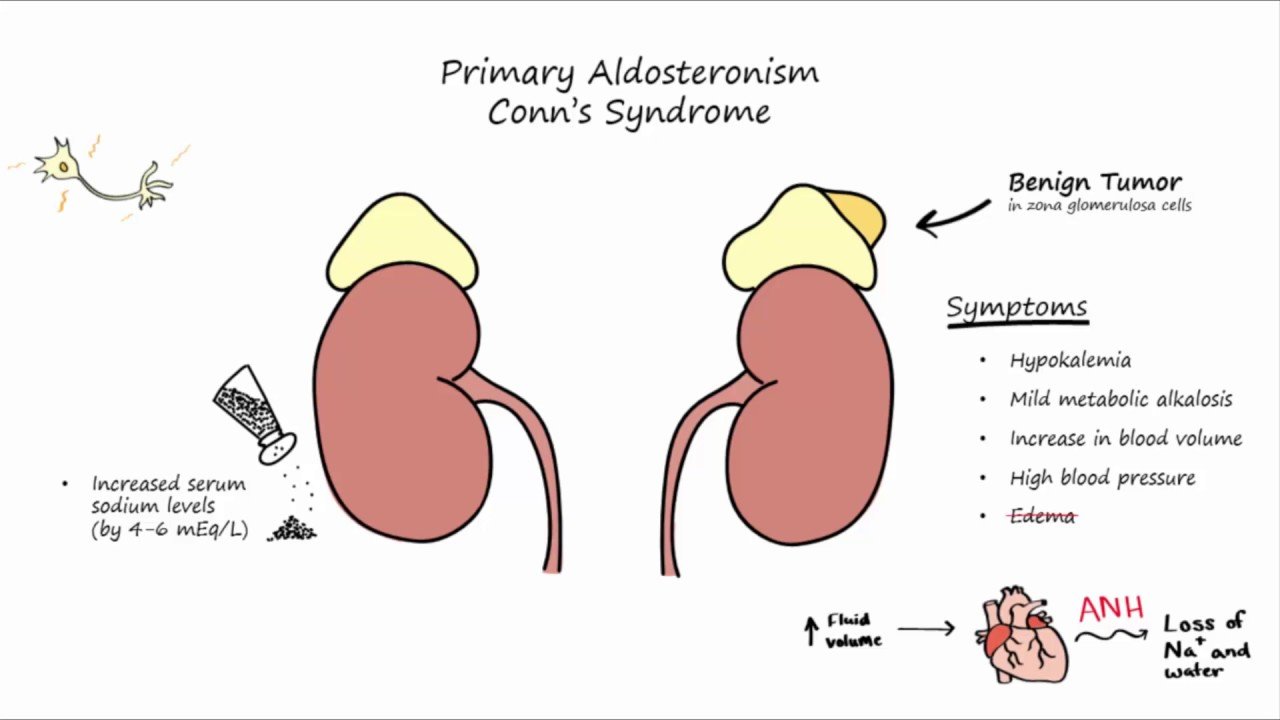
Aldosterone
Aldosterone is a steroid hormone produced by the adrenal cortex. It plays a critical role in the regulation of blood pressure by controlling sodium and potassium levels. When blood volume or blood pressure is low, or when potassium levels are high, aldosterone is secreted.
It acts on the distal convoluted tubules and collecting ducts of the kidney, promoting sodium reabsorption and potassium excretion. As sodium is reabsorbed, water passively follows, increasing blood volume and pressure. Aldosterone secretion is primarily regulated by angiotensin II, part of the RAAS, and plasma potassium levels.
Atrial Natriuretic Peptide (ANP)
ANP is a hormone secreted by the atrial cells of the heart when atrial pressure increases, typically due to increased blood volume. It acts as a counter-regulatory mechanism for the RAAS, inhibiting the secretion of renin, aldosterone, and ADH, leading to vasodilation and decreased blood pressure. ANP promotes the excretion of sodium and water by the kidneys, thus reducing blood volume and pressure. It also inhibits the absorption of sodium in the kidney tubules, further contributing to the excretion of salt and water.
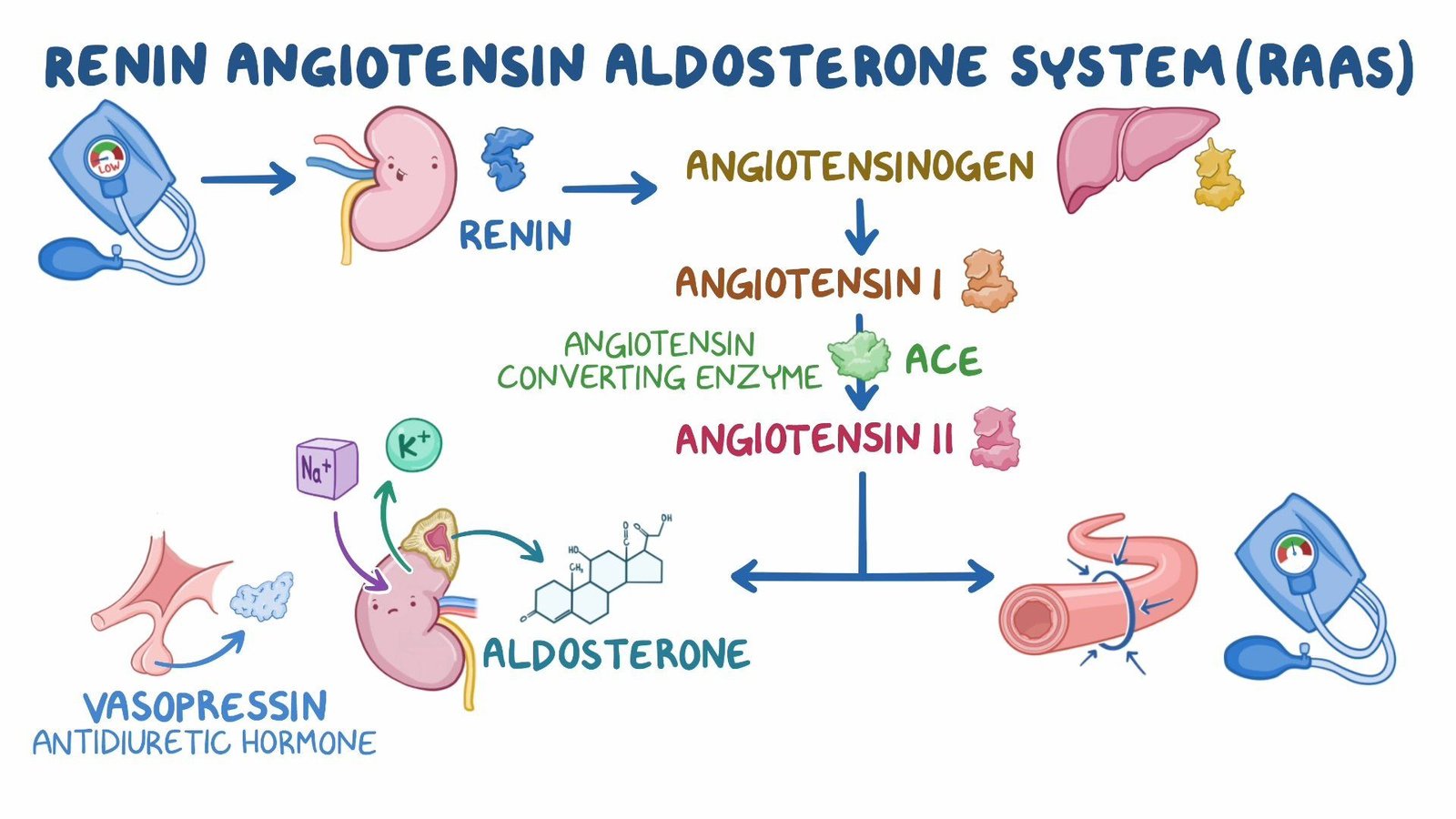
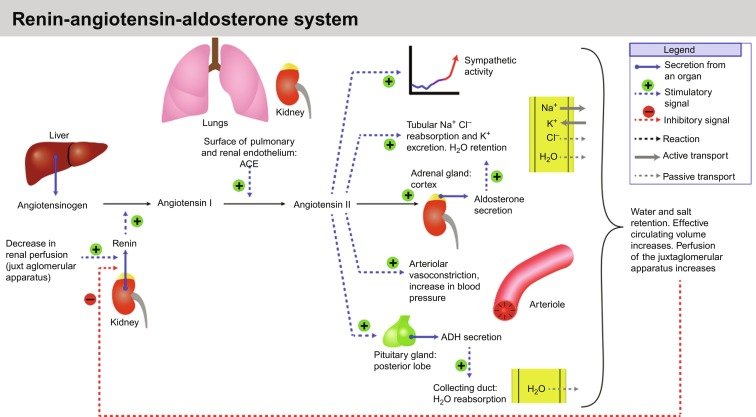
Renin-Angiotensin-Aldosterone System (RAAS)
The RAAS is a critical hormonal pathway in the regulation of renal function. When blood volume or pressure drops, or when there is a decrease in sodium chloride delivery to the distal tubules, the juxtaglomerular cells of the kidneys secrete renin. Renin converts angiotensinogen, a protein synthesized by the liver, into angiotensin I, which is then converted into angiotensin II by angiotensin-converting enzyme (ACE) primarily in the lungs.
Angiotensin II has several effects: it stimulates the secretion of aldosterone, causes vasoconstriction, increases blood pressure, and stimulates ADH release, thereby promoting water reabsorption.
The Interplay of Hormones and Kidney Function
The hormonal control of kidney function is a classic example of negative feedback mechanisms maintaining homeostasis. When blood pressure falls, for instance, the RAAS is activated to increase blood volume and pressure. Once the desired blood pressure is achieved, the stimuli for RAAS activation diminish, decreasing the pathway’s activity. This precise regulation ensures that the internal environment remains stable despite external changes.
Dysregulation of Hormonal Control and Disease
Aberrations in the hormonal control of kidney function can lead to various pathophysiological conditions. For instance, excessive release of ADH can result in water retention and hyponatremia, a condition called syndrome of inappropriate antidiuretic hormone secretion (SIADH). Conversely, insufficient ADH causes diabetes insipidus, characterized by excessive urination and thirst.
Hyperaldosteronism, which involves excess aldosterone secretion, can lead to hypertension and hypokalemia, whereas hypoaldosteronism can result in hyperkalemia and acidosis. ANP dysregulation is often associated with heart failure, where it is released in response to increased atrial pressure, albeit with diminishing effectiveness.

Conclusion
The endocrine regulation of kidney function is an intricate and vital aspect of the body’s ability to maintain homeostasis. The hormones ADH, aldosterone, ANP, and the components of the RAAS work in concert to regulate fluid and electrolyte balance, as well as blood pressure.
Understanding these regulatory mechanisms is essential not only for comprehending normal physiology but also for recognizing the pathophysiology of renal and endocrine disorders. Advances in medical science continue to reveal the complexity of these interactions and the potential for targeted therapies to address the various conditions resulting from their dysregulation.
Read more: