Definition of Blood Transfusion – Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialisms with differing levels of prescriber authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurses are permitted by most jurisdictions to practice independently in a variety of settings depending on training level. In the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient’s family, and other team members, that focus on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of an interdisciplinary healthcare team such as therapists, medical practitioners, and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
Definition of Blood Transfusion
Blood transfusion is generally the process of receiving blood or blood products into one’s circulation intravenously. Transfusions are used for various medical conditions to replace lost
components of the blood.
Or,
Blood transfusion consists of administration of compatible donor’s whole blood or any of its components to correct/treat any clinical condition.

Purposes of Blood Transfusion:
1. To increase circulating blood volume following surgery, trauma or hemorrhage.
2. To increase the number of red blood cells and to maintain hemoglobin levels in clients with serve anemia.
3. To provide selected cellular components as replacement therapy, (e.g. clotting factors, platelets, albumin).
4. To replace circulating blood volume.
5. Restores or improves the ability to control bleeding.
6. Improves the ability to overcome infection.
7. Replace clotting factors or increases intravascular fluid volume by increasing colloidal osmotic pressure.
8. Treats blood clotting disorders such as hemophilia.
9. To correct anemia.
Indications of Blood Transfusion:
- Severe blood loss or haemorrhage.
- To replace circulating volume and maintain oxygen delivery.
- Major operative procedures.
- Following severe bums where there is excessive haemolysis and dehydration.
- Postoperatively in severe debilitated & anemic patients.
- During pre-operative preparation in severe anaemia.
- To arrest haemorrhage or as a prophylactic measure prior to surgery, in a patient with a haemorrhage state such as thrombocytopenia, haemophilia or liver disease.
Contraindication of Blood Transfusion:
- Coronary thrombosis.
- Congestive cardiac failure (CCF).
- Acute renal failure.
- Hypertension.
- Polycythaemia
Procedure of Blood Transfusion:
A. Articles:
1. Blood transfusion set.
2. Blood or Blood components-sterile in appropriate container
3. I/V cannula No 18/20
4. Antiseptic solution or disinfectant- spirit, Betadine etc.
5. Sterile, cotton swab.
6. Tourniquet.
7. Adhesive tape.
8. Scissors
9. Sterile gauze or cotton.
10. Infusion stand.
11. Roller bandage and splint (optional)
12. Kidney tray or disposable bag.
13. Gloves.
B. Procedure:
1. Verify doctor’s order. Inform the client and explain the purpose of the procedure.
2. Check for cross matching and typing. To ensure compatibility
3. Obtain and record baseline vital signs
4. Practice strict asepsis
5. At least 2 licensed nurse check the label of the blood transfusion. Check the following:
- Serial number
- Blood component
- Blood type
- Rh factor
- Expiration date
- Screening test (VDRL, HBsAg, malarial smear) – this is to ensure that the blood is free from blood-carried diseases and therefore, safe from transfusion.
6. Warm blood at room temperature before transfusion to prevent chills.
7. Identify client properly. Two Nurses check the client’s identification.
8. Use needle gauge 18 to 19 to allow easy flow of blood.
9. Use BT set with special micron mesh filter to prevent administration of blood clots and particles.
10. Start infusion slowly at 10 gtts/min. Remain at bedside for 15 to 30 minutes. Adverse reaction usually occurs during the first 15 to 20 minutes.
11. Monitor vital signs. Altered vital signs indicate adverse reaction (increase in temp, increase in respiratory rate)
12. Do not mix medications with blood transfusion to prevent adverse effects. Do not incorporate medication into the blood transfusion. Do not use blood transfusion lines for IV push of medication.
13. Administer 0.9% NaCl before; during or after BT. Never administer IV fluids with dextrose. Dextrose based IV fluids cause hemolysis.
14. Administer BT for 4 hours (whole blood, packed RBC). For plasma, platelets, w cryoprecipitate, transfuse quickly (20 minutes) clotting factor can easily be destroyed.
15. Observe for potential complications. Notify physician.
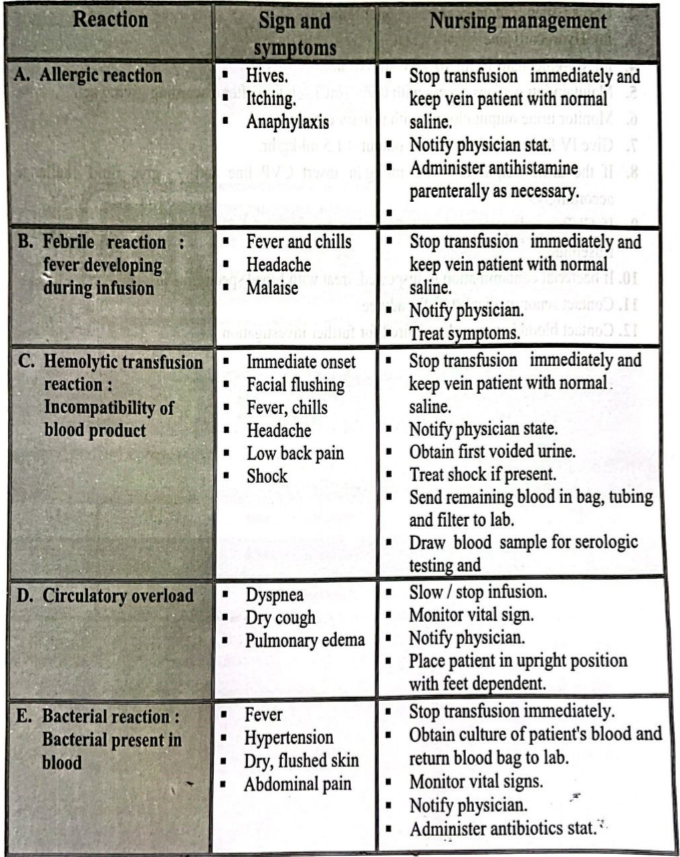
Hazards/Reaction of Blood Transfusion & Management:
Management of Mismatch Blood Transfusion:
1. Stop transfusion immediately.
2. Check patient’s identity against donor unit.
3. Inj. Hydrocortisone 2 vial IV stat.
4. Inj. Ca-gluconate 10 ml 10% IV slowly stat.
5. Maintain intravenous access with 0.9% NaCl solution after discarding giving set.
6. Monitor urine output closely with urinary catheter.
7. Give IV fluid to maintain urine output < 1.5 ml/kg/hr.
8. If the urine output is 1.5 ml/kg/hr insert CVP line and give fluid challenge accordingly.
9. If CVP is adequate and still the urine output is 1.5 ml/kg/hr, then give injection frusemide.
10. If bacterial contamination is suspected, treat with broad spectrum IV antibiotics.
11. Contact senor medical staff for advice.
12. Contact blood ban sample required for further investigation.
Advantages of Oral Route:
1. Oral route is cheap, safe and painless route.
2. Convenient route because drug can be given in the form of tablet or capsule which contain exact dose.
3. Self-medication is possible
4. Prolong action can be obtained by delaying absorption
5. Drugs need not sterile and highly purified.
. Free from fear and anxiety for pricking needle &associated with pain.
6 7. This route has psychological effect on the patient that he has taken medicine.
8. It is easy and patient can take the drug without interrupting his activity.
9. Hypersensitivity reaction in many cases is less.
Disadvantages of Oral Route:
1. Onset of drug action is slow due to delayed absorption. So not suitable for emergency cases.
2. Irritant, unpleasant and hypertonic drugs cannot be administered.
3. This route may not be useful in presence of vomiting or diarrhea.
4. This route cannot be employed in an unconscious or non-co-operative patient.
5. Drugs that are destroyed by digestive juice are not administered orally, e.g. insulin, heparin.
6. Drugs having high first pass metabolism are not given orally, e.g. Testosterone.
7. The absorption of certain drugs are irregular and negligible, e.g. Streptomycin, Neomycin.
Purposes of Oral Medications:
1. To provide a medication that has systematic or local effect on gastrointestinal tract.
2. To prevent the disease.
3. To cure the disease.
4. To promote the health.
5. To give palliative treatment.
6. To give as a systematic treatment.