Dying and Death Care – Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialisms with differing levels of prescriber authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurses are permitted by most jurisdictions to practice independently in a variety of settings depending on training level. In the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient’s family, and other team members, that focus on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of an interdisciplinary healthcare team such as therapists, medical practitioners, and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
Dying and Death Care
Definition of Dying Patient
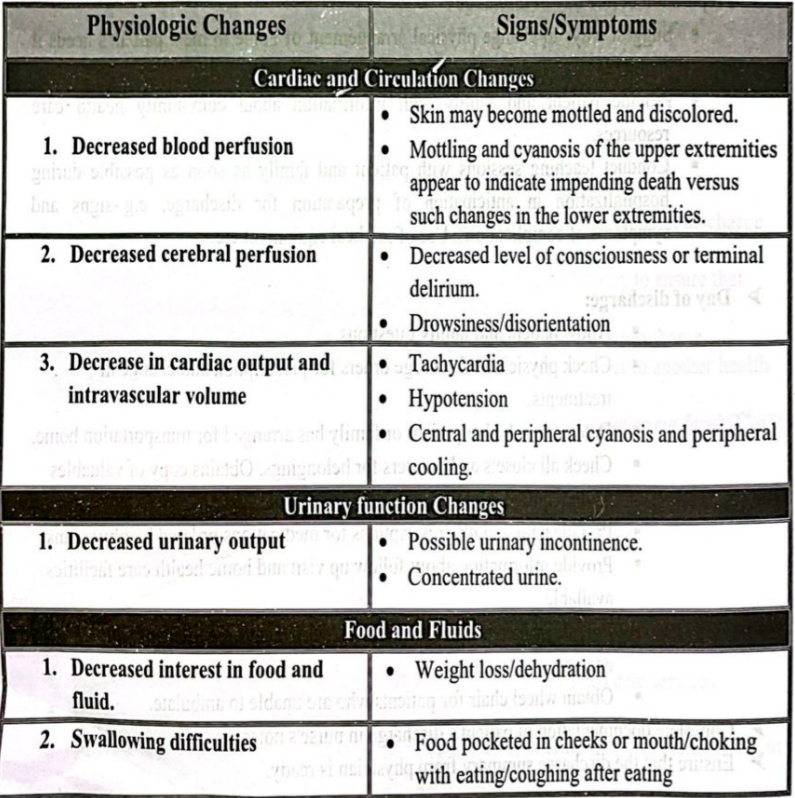
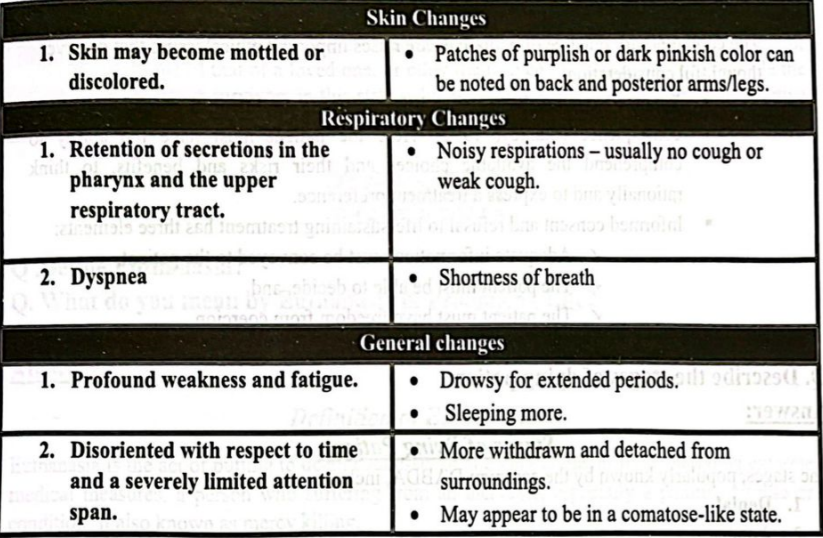
Dying patients are very close to death, and exhibit many signs and symptoms of near-death. For instance, actively dying patients are often times unresponsive, and their blood pressure often drops significantly.
Management of Dying Patient:
1. The person who deals with the dying patient must commit to:
- Deal with mental anguish and fear of death,
- Try to respond appropriately to patient’s needs by listening carefully to the complaints and
- Be fully prepared to accept their own counter transferences, as doubts, guilt and damage to their narcissism are encountered.
2. Management of the dying patient often elicits anxiety in nursing staff. Education and role playing can improve perspective taking and empathetic skills, respect each other’s point of view as well as appreciate the situation of patient and their families.
- Developing a sense of control and efficacy,
- Encouraging peer groups for families coping with bereavement.
- Developing increased resourcefulness in dealing with death related situations.
- Recognizing that a moderate level of death anxiety is acceptable.
- Improving our understanding of pain and suffering will also improve communication and effective interactions.
3. Ethical and Legal Issues
The contemporary practice of palliative care raises important ethical issues that deserve thoughtful consideration.
- Patients have a right to refuse Life-sustaining treatment, even if they die as a consequence (Stanley, 1992). Here the patient must have the ability to comprehend the available choices and their risks and benefits, to think rationally and to express a treatment preference.
- Informed consent and refusal to life-sustaining treatment has three elements:
✓ Adequate information must be conveyed to the patient,
✓ The patient must be able to decide, and
✓The patient must have freedom from coercion.
Stages of Dying Patient:
The stages, popularly known by the acronym DABDA, include:
1. Denial
2. Anger
3. Bargaining
4. Depression
5. Acceptance
Denial – The first reaction is denial. In this stage, individuals believe the diagnosis is somehow mistaken, and cling to a false, preferable reality.
Anger – When the individual recognizes that denial cannot continue, they become frustrated, especially at proximate individuals. Certain psychological responses of a person undergoing this phase would be: “Why me? It’s not fair!”; “How can this happen to me?”; “Who is to blame?”; “Why would this happen?”
Bargaining – The third stage involves the hope that the individual can avoid a cause of grief. Usually, the negotiation for an extended life is made in exchange for a reformed lifestyle. People facing less serious trauma can bargain or seek compromise. Examples include the terminally ill person who “negotiates with God” to attend a daughter’s wedding, an attempt to bargain for more time to live in exchange for a reformed lifestyle or a phrase such as “If I could trade their life for mine”.
Depression – “I’m so sad, why bother with anything?”; “I’m going to die soon, so what’s the point?”; “I miss my loved one; why go on?” During the fourth stage, the individual despairs at the recognition of their mortality. In this state, the individual may become silent, refuse visitors and spend much of the time mournful and sullen.
Acceptance – “It’s going to be okay.”; “I can’t fight it; I may as well prepare for it.” In this last stage, individuals embrace mortality or inevitable future, or that of a loved one, or other tragic event. People dying may precede the survivors in this state, which typically comes with a calm, retrospective view for the individual, and a stable condition of emotions.
Euthanasia
Definition of Euthanasia:
Euthanasia is the act of putting to death painlessly or allowing to die, as by withholding extreme medical measures, a person who suffering from an incurable, especially a painful, disease or condition. It also known as mercy killing.
Or,
Euthanasia may be defined as the act or practice of killing someone who is very sick or injured in order to prevent any more suffering
Or
Euthanasia is the termination of a very sick person’s life in order to relieve them of their suffering.
Prolonging Life
Prolonging life means multidisciplinary life care of the client which helps to improve physical, mental, social & spiritual health of the client.
Or
Prolonging life means prolongation of life by providing supportive care to improve health condition of the client, relief him/her from sufferings, pain and maintaining of healthy life.
Types of Euthanasia
Different practices fall under the label “euthanasia.” Here are some distinctions demarcating different versions.
Active Euthanasia:
- Killing a patient by active means, for example, injecting a patient with a lethal dose of a drug. Sometimes it called “aggressive” euthanasia.
Passive euthanasia:
- Intentionally letting a patient die by withholding artificial life support such as a ventilator or feeding tube is known as Passive euthanasia.
- Some ethicists distinguish between withholding life support and withdrawing life support (the patient is on life support but then removed from it).
Voluntary euthanasia:
- With the consent of the patient
Involuntary euthanasia:
- Without the consent of the patient, for example, if the patient is unconscious and his or her wishes are unknown.
- Some ethicists distinguish between “involuntary” (against the patient’s wishes) and “non- voluntary” (without the patient’s consent but wishes are unknown) forms.
Self-administered euthanasia
- The patient administers the means of death.
Other-administered cuthanasia:
- A person other than the patient administers the means of death.
Assisted:
- The patient administers the means of death but with the assistance of another person, such as a physician
- There are many possible combinations of the above types, and many types of euthanasia are morally controversial. Some types of euthanasia, such as assisted voluntary forms, are legal in some countries.
Mercy-killing
- The term “mercy-killing” usually refers to active, involuntary or non-voluntary, other- administered euthanasia. In other words, someone kills a patient without their explicit consent to end the patient’s suffering. Some ethicists think that
Physician-assisted suicide:
- The phrase “physician-assisted suicide” refers to active, voluntary, assisted euthanasia where a physician assists the patient. A physician provides the patient with a means, such as sufficient medication, for the patient to kill him or herself.
Advantages and Disadvantages of Euthanasia:
1. Advantages of Euthanasia;
- Painless death.
- Speedy termination of physical and emotional sufferings.
- Saves family money
- Orgar can be put to good use.
- It provides a way to relieve extreme pain
- It provides a way of relief when a person’s quality of life is low
- Frees up medical funds to help other people
- It is another case of freedom of choice
2. Disadvantages of Euthanasia:
- Euthanasia devalues human life
- Euthanasia can become a means of health care cost containment
- Physicians and other medical care people should not be involved in directly causing death
- Religious grounds: it is immoral for Muslims, Catholics and other religious beliefs.
- Common sense grounds: Euthanasia is permanent
Why people want euthanasia?
- Most people think unbearable pain is the main reason people seek euthanasia, but some surveys in the USA and the Netherlands showed that less than a third of requests for euthanasia were because of severe pain.
- Terminally ill people can have their quality of life severely damaged by physical conditions such as incontinence, nausea and vomiting, breathlessness, paralysis and difficulty in swallowing.
- Psychological factors that cause people to think of euthanasia include depression, fearing loss of control or dignity, feeling a burden, or dislike of being dependent.