Definition of Haemorrhage – Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialisms with differing levels of prescriber authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurses are permitted by most jurisdictions to practice independently in a variety of settings depending on training level. In the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Definition of Haemorrhage | CHAPTER 21 | Fundamentals of Nursing
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient’s family, and other team members, that focus on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of an interdisciplinary healthcare team such as therapists, medical practitioners, and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
Definition of Haemorrhage/Bleeding
Bleeding, also known as hemorrhage or haemorrhage, is blood escaping from the circulatory system. Bleeding can occur internally, where blood leaks from blood vessels inside the body, or externally, either through a natural opening such as the mouth, nose, ear, urethra, vagina or anus, or through a break in the skin, Hemorrhage or bleeding is a flow of blood from an artery, vein or capillary.
Bleeding, or hemorrhage, is the name used to describe blood loss. It can refer to blood loss inside the body, called internal bleeding. Or it can refer to blood loss outside of the body, called external bleeding
Or,
Haemorrhage is the condition in which the blood flows out from the blood vessels due to some accident or injuries,
Types/Classification of Haemorrhage:
A. According to its Situation/Visibility:
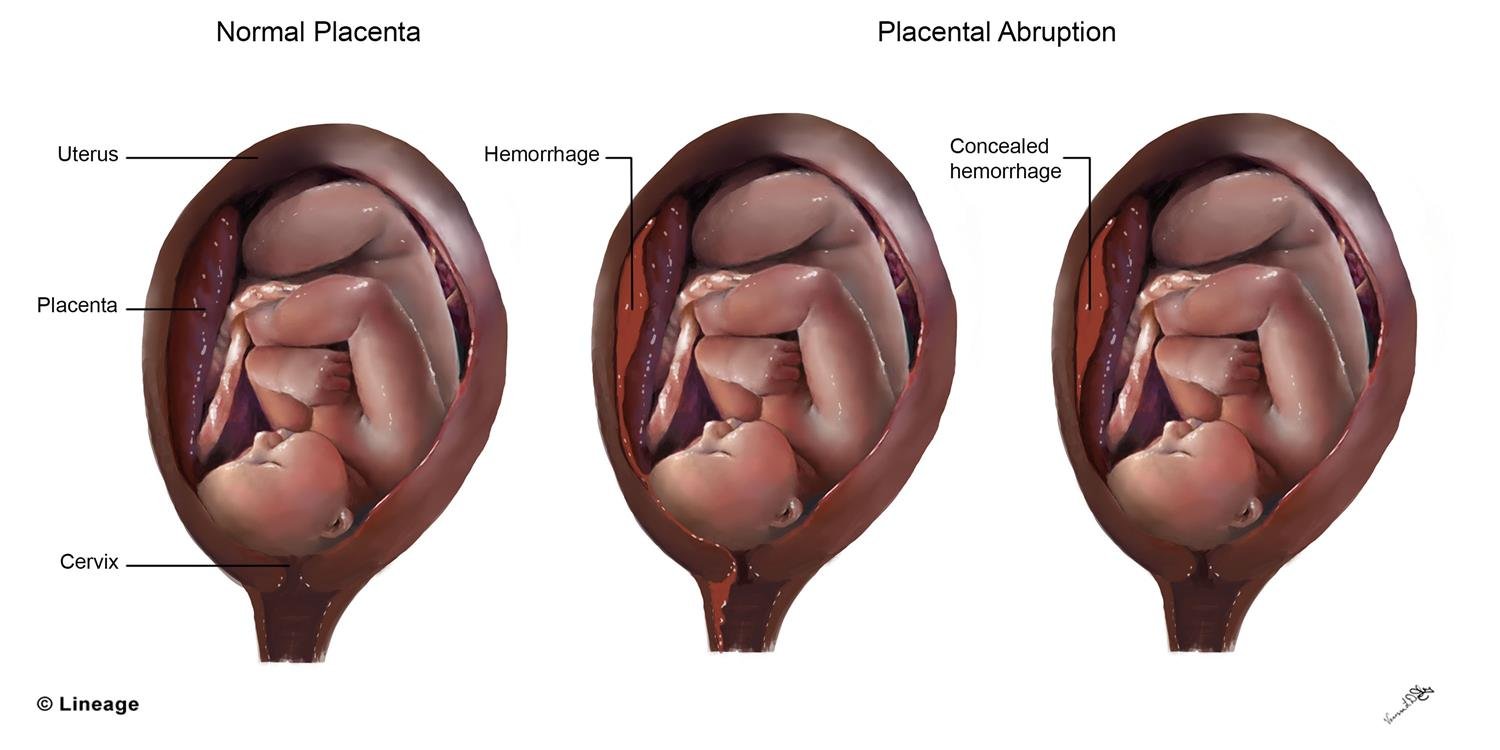
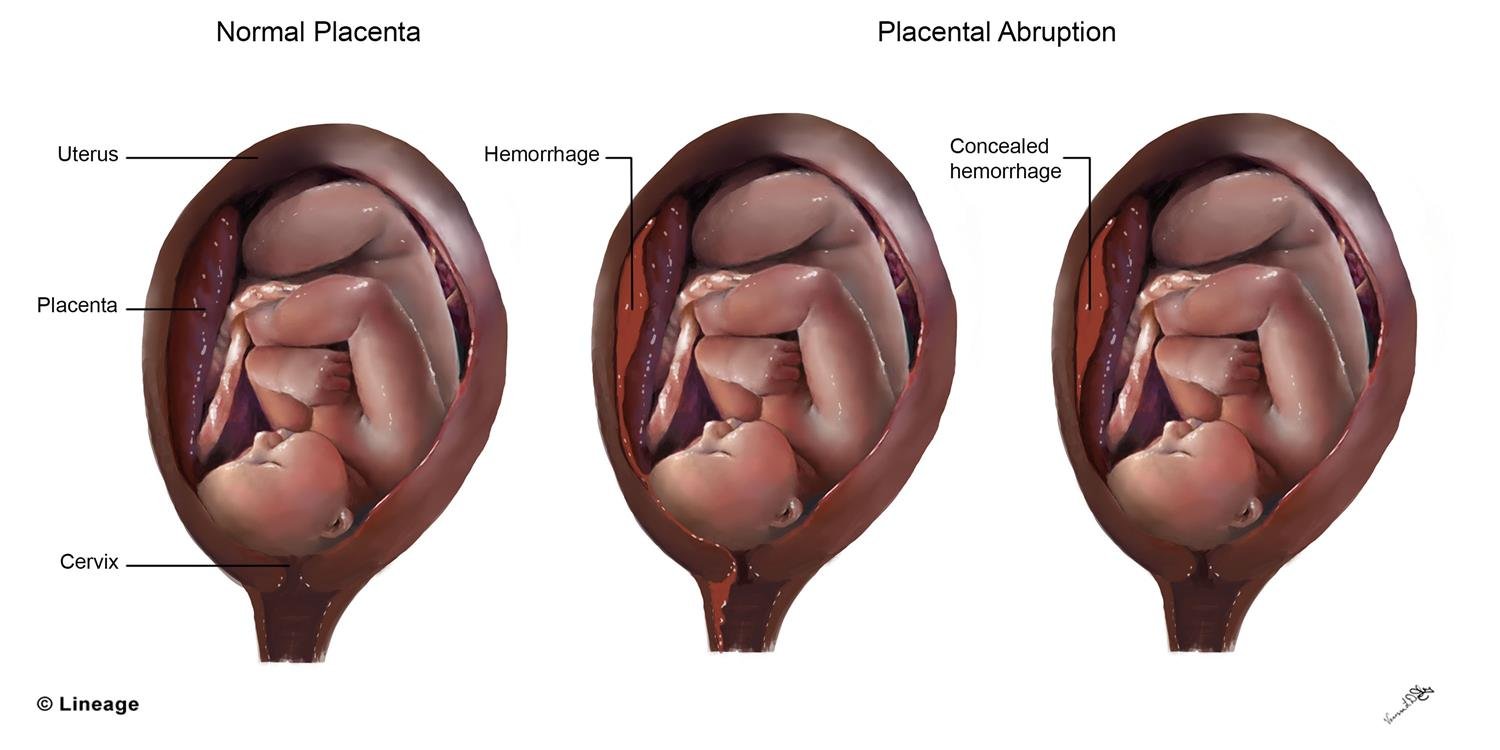
a) External haemorrhage: In this instance, the blood escapes from the blood vessel on the surface of the body and can be seen
b) Internal or concealed haemorrhage: In this type of haemonhage blood escapes from a blood vessel into a cavity or organ of the body or into the tissues.
B. According to sources of haemorrhage: Haemonhage may be classified according to the type of blood vessel involved.
a) Arterial bleeding:
If an artery is served the blood will be-
- Bright red in colour. This is due to the presence of oxygen in the blood.
- Spurting from the wound-each spurt coincides with the heartbeat.
- Escaping from the wound under great pressure.
(Artery a tube or vessel that carries blood from the heart to all parts of the body)
b) Venous bleeding: If a vein is served the blood will be-
- Dark red in color; This is due to the small amount of oxygen present in the blood
- Flowing from the wound in a steady stream and will not be under great pressure.
- Escaping from the part of the wound farther away from the heart.
c) Capillary bleeding: This occurs in superficial wounds for example in the blood will be-
- Oozing from the wound,
- Neither bright red nor dark red in color.
- Welling up from all over the wound.
- It is important to realize that in large lacerated wounds all types of blood vessels may be involved.
C. According to the time it occurs:
a) Primary haemorrhage: This occurs at the time of the injury or operation or when diseases have damaged the blood vessels.
b) Reactionary haemorrhage: It is important to appreciate that up to twenty-four hours after an injury or operation bleeding may commence again. This bleeding is due to the reaction of the body. If there has been a hemorrhage nature employs there agencies to prevent serious loss of
blood.
c) Secondary haemorrhage: Fortunately, this type of hemorrhage sudden occurs but if it does, it takes place in anything from seven to ten days after the injury or operating and is due to infection.
D. According to mode of action:
a) Acute haemorrhage: Stab injury, ruptured spleen and liver, bleeding during operation.
b) Chronic haemorrhage: Hook warm infestation, bleeding peptic ulcer, haemorroids, menorrhagia, cancer.
Signs and Symptoms of Internal Haemorrhage:
- Abdominal pain
- Blood in the stool
- Black, tarry stool (melena)
- Blood in the urine
- Vomiting blood
- Chest pain
- Abdominal swelling
- Pale, clammy, sweaty skin.
- Breathlessness.
- Extreme thirst.
- Unconsciousness.
Sign and symptoms of External Bleeding:
- Changes in the skin, it becomes pale and white.
- Subnormal temperature (35°C or 95 °F)
- Tachycardia and bradycardia
- Pain
- If the patient conscious the patient looks like anxious, afraid, and restless
- Excessive thirst.
- Signs and symptoms of shock
- Air hunger respiration
- Empty vein
- Blurred vision
- Dialated pupil.
- Buzzing
Causes of Haemorrhage
Bleeding arises due to either traumatic injury, underlying medical condition
A) Traumatic Injury: Traumatic bleeding is caused by some type of injury. There are different types of wounds which may cause traumatic bleeding. These included
a) Abrasion – Also called a graze, this is caused by transverse action of a foreign object boold against the skin, and usually does not penetrate below the epidermisun
b) Excoriation – In common with Abrasion, this is caused by mechanical destruction of the skin, although it usually has an underlying medical cause
c) Hematoma – Caused by damage to a blood vessel that in turn causes blood to collect under the skin
d) Laceration – Irregular wound caused by blunt impact to soft tissue overlying hard tissue or tearing such as in childbirth. In some instances, this can also be used to describe an owan incision.
e) Incision – A cut into a body tissue or organ, such as by a scalpel, made during surgery..
f) Puncture Wound – Caused by an object that penetrated the skin and underlying layers, such as a nail, needle or knife
g) Contusion – Also known as a bruise, this is a blunt trauma damaging tissue under the surface of the skin boold emitimo
h) Crushing Injuries – Caused by a great or extreme amount of force applied over a period of time. The extent of a crushing injury may not immediately present itself. nimobdA
i) Ballistic Trauma – Caused by a projectile weapon such as a firearm. This may include two external wounds (entry and exit) and a contiguous wound between the two
B) Medical condition
a) Intravascular changes – changes of the blood within vessels (e.g. ↑ blood pressure, ↓ clotting factors)
b) Intramural changes – changes arising within the walls of blood vessels (e.g. aneurysms, dissections, AVMs, vasculitides)
c) Extravascular changes – changes arising outside blood vessels (e.g. H pylori infection, brain abscess, brain tumor)
Origin of Haemorrhage
A. Mouth
- Tooth eruption – losing a tooth
- Hematemesis – vomiting fresh blood
- Hemoptysis-coughing up blood from the lungs
B. Anus
- Hematochezia-rectal blood
- Malena-loss of blood through faeces
C. Urinary tract
- Hematuria-blood in the urine from urinary bleeding
D. Upper head
- Intracranial hemorrhage – bleeding in the skull. pealdsitsmejal temves
- Cerebral hemorrhage – a type of intracranial hemorrhage, bleeding within the brain tissue itself.
- Intracerebral hemorrhage – bleeding in the brain caused by the rupture of a blood adio od vessel within the head. See also hemorrhagic stroke.
- Subarachnoid hemorrhage (SAH) implies the presence of blood within the subarachnoid space from some pathologic process. The common medical use of the term SAH refers to the nontraumatic types of hemorrhages, usually from rupture of a berry aneurysm or arteriovenous malformation (AVM). The scope ofis article is limited tok these non-traumatic hemorrhages.
E. Lungs
- Pulmonary hemorrhage
F. Gynecologic
- Vaginal bleeding
✔ Postpartum hemorrhagen
✔ Breakthrough bleeding
- Ovarian bleeding. This is a potentially catastrophic and not so rare complication among lean patients with polycystic ovary syndrome undergoing transvaginal oocyte retrieval
G. Gastrointestinal
- Upper gastrointestinal bleed
- Lower gastrointestinal bleed
- Occult gastrointestinal bleed
H. Epistaxis- bleeding from nose
The World Health Organization made a standardized grading scale to measure the severity of bleeding
1. Grade 0 No bleeding
2. Grade 1 Petechial bleeding,
3. Grade 2 Mild blood loss (clinically significant);
4. Grade 3 Gross blood loss, requires transfusion (severe);
5. Grade 4 Debilitating blood loss, retinal or cerebral associated with fatality
Effect of Haemorrhage
- The loss of red blood cells causes a lack of oxygen to the body system.
- A decrease in blood volume causes a decrease in blood pressure.
- The heart’s pumping rate increases to compensate for reduced blood pressure.
- The force of the heart beat is reduced since there is less blood to pump.
First Aid Treatment of Internal Bleeding
1. Keep the patient in comfortable position, patient must be rest in mind.
2. If available put synthetic gloves on as bleeding may become apparent.
3. Check airway, breathing and circulation. Begin cardiopulmonary resuscitation (CPR) if necessary. If you want to understand CPR in more depth then go to CPR-Q’s & A’s.
4. If unconscious and breathing – place the person in the recovery position and with legs higher than the heart if possible. Injuries permitting.
5. If conscious lie the casualty down and raise or bend legs if injuries permit.
6. Keep casualty warm. This may help delay the onset of shock by minimizing the bodies heat loss.
7. Reassure and stay calm. This helps provide security for the injured person.
8. Continue to check pulse and breathing.
9. Treat other injuries as appropriate.
10. Do not give anything to eat or drink as they may require surgery to stop the bleeding.
11. Keep a record of any specimen passed or vomited by casualty. If possible send sample in the hospital.
12. Sedation should be given. Such as inj.
13. Send the patient to the hospital as soon as possible to prevent further complication.
First Aid Treatment of External Bleeding:
1. Calm and reassure the person.
2. Lay the person down.
3. Apply firm, direct pressure using a clean pad (or sterile dressing if available) over the wound. The person’s own hand can be used to apply pressure whilst getting a suitable dressing/putting on your gloves.
4. Whilst applying the direct pressure, elevate and support the injured area above the level of the heart.
5. Firmly wrap a bandage around the pad or dressing to hold it in place, but not so firmly that it cuts off the circulation extremities.
6. If blood soaks through the pad and bandage, do not remove but cover with another pad and bandage, continuing to apply pressure to the wound until bleeding is controlled.
7. Monitor for symptoms of shock: pale, cold or clammy skin; rapid breathing; rapid or weak pulse; reduced level of consciousness.
8. If symptoms of shock are present:
- With the person lying down, raise and support their legs above the level of their heart (continue to keep the injured part elevated as well).
- Loosen any tight clothing around their neck or their waist.
- Keep the person warm.
Epistaxis
Definition of Epistaxis:
Epistaxis is the common occurrence of bleeding from the nose. It is usually noticed when the blood drains out through the nostrils.
Or
Hemorrhage from the nose, usually due to rupture of small vessels overlying the anterior part of the cartilaginous nasal septum is known as epistaxis.
Or
Any bleeding per nose is called epistaxis. It is a symptom as well as a sign. It is not a disease but is the result of some local or systemic disease
Causes of Epistaxis
The two most common causes of nosebleeds are:
A. Dry air when your nasal membranes dry out, they’re more susceptible to bleeding and infections
B. Nose picking
C. Other causes of nosebleeds include
- Acute sinusitis
- Allergies
- Aspirin use
- Hemophilia (and other bleeding disorders)
- Blood thinners (anticoagulants), such as warfarin and heparin
- Chemical irritants, such as ammonia
- Chronic sinusitis
- Cocaine use
- Common cold
- Deviated septum
- Foreign body in the nose
- Nasal sprays, such as those used to treat allergies, if used frequently
- Non-allergic rhinitis
- Trauma to the nose
D. Less common causes of nosebleeds include:
- Alcohol use
- Leukemia
- Nasal polyps
- Nasal surgery
- Nasal tumor
- Second trimester pregnancy
Sign and Symptoms of Epistaxis:
A. Signs
- Anxious
- Shock
- Discharge of blood
B. Symptoms
- Sudden onset of bleeding from the nose
- Movement increase bleeding.
First aid management of epistaxis patient
1. Place the patient in a chair in a sitting position with the head held forward. In severe bleeding this will prevent the blood following to the back of the nose and throat and may prevent it from being nou swallowed or inhaled.
2. Loosen tight clothing round the neck, chest, and waist and place the patient near an open window.
3. Ask the patient to breathe through his or her mouth.
4. Pinch the nose firmly between the thumb and force finger.
5. A cold compress in the form of a handkerchief wrung out in iced water can be applied over the bridge of the nose and at the back of the neck.
6. Keeping the patient sitting very still
7. Tell the patient not blow his nose for a few hours.
8. If the bleeding is very severe and does not stop within several minuets the patient may require to ambe seen by a doctor who will carry out any further treatment which may be necessary.
Nursing Management of Epistaxis:
1. Continuous monitoring of-
- Vital signs
- Bleeding.
- Hypoxiad
- Respiratory difficulty and
- Nasal packing
2. Teaching the parents and family members about measures to stop epistaxis and immediate medical help are also important.
3. Instructions to be given to the parents to apply lubricant to nasal septum twice daily to reduce dryness and to avoid nasal blowing or packing nose after nose bleed.
4. Preventive measures of foreign body in the nose.
5. Preventive measures of nasal injury.
6. Need for management of local and systemic cause of epistaxis should be informed and emphasized.
Haemoptysis
Definition of Haemoptysis:
Hemoptysis or haemoptysis is the act of coughing up blood or blood-stained mucus from the bronchi, larynx, trachea, or lungs.
Or
This is the term used to describe “coughing up” of blood. The blood may be coming from any part of the respiratory tract, commonly it is coming from the lungs.
Coughing up blood, irrespective of the amount is called haemoptysis.
Haemoptysis is the coughing of blood originating from the respiratory tract below the level of the larynx.
Signs and Symptoms of Haemoptysis:
A. Symptoms
a) Abrupt-onset cough, fever with bloody and purulent sputum – suggestive of acute pneumonia or bronchitis.
b) Chronic productive cough – suggestive of chronic bronchitis or bronchiectasis.
c) Fevers, night sweats and weight loss – consider TB and other infections or malignancy.
d) Anorexia, weight loss and changing cough – think of possible bronchogenic carcinoma.
e) Dyspnoea, fatigue, orthopnoea, paroxysmal nocturnal dyspnoea, frothy pink sputum suggestive of congestive heart failure.
f) Dyspnoea and pleuritic chest pain – consider a PE.
B. Signs
a) Signs of vasculitis.
b) The diastolic murmur of mitral stenosis.
c) Signs of LVF.
d) Anaemia
e) Clubbing
f) Raised temperature.
g) Lymphadenopathy.
h) Tachypnoea, tachycardia
i) Inspiratory and expiratory rhonchi (associated with airway secretions and blood).
Causes of Haemoptysis:
A. Trachea or bronchusa
a) Malignancy:
- Bronchogenic carcinoma.
- Endobronchial metastatic tumour.
- Kaposi’s sarcoma.
- Carcinoid tumour.
b) Bronchitis.
c) Bronchiectasis.
d) Airway trauma.
e) Foreign body.
B. Lung parenchyma
a) Lung abscess.
b) Pneumonia – bacterial (eg, Staphylococcus aureus, Pseudomonas aeruginosa) or viral (eg, influenza).
c) Tuberculosis (TB).
d) Fungal infection and mycetoma.
e) Hydatid cysts.
f) Lupus pneumonitis.
g) Lung contusion.
h) ‘Crack’ lung.
C. Vascular
a) Arteriovenous malformation
b) Aortic aneurysm.
c) Pulmonary embolism (PE).
d) Mitral stenosis.
e) Trauma.
D) Other
a) Pulmonary endometriosis.
b) Congenital or acquired systemic coagulopathy – eg, leukaemia.
c) Anticoagulant or thrombolytic agents.
d) Factitious haemoptysis.
First Aid management of Haemoptysis:
1. The patient should be placed in a comfortable position. Sitting up in a chair of at home propped up in bed.
2. Tight clothing around the neck, chest and waist should be loosened.
3. The patient must be reassured and kept very still and quite. Any movement or excitement might. Cause further bleeding.
4. Ice may be given to suck.
5. Medical aid should be obtained. It is important to have the extent of the damage investigated as soon as possible.
6. Keep all specimens of sputum for the doctors inspection by examining them he may be able to assess the amount of damage.
Haematemesis
Definition of Haematemesis:
Hematemesis or haematemesis is the vomiting of blood. The source is generally the upper gastrointestinal tract, typically above the suspensory muscle of duodenum.
The medical word for vomiting blood is haematemesis. This symptom is usually due to a problem within the upper gut. That is, the gullet (oesophagus), stomach or the first part of the small intestine (duodenum).
or
This is the term for “vomiting” blood. The blood may be coming from any part of the upper alimentary tract, probably the commonest site of bleeding is from gastric ulcer (Stomach), but the bleeding may be from the oesophagus or from a duodenal ulcer.
Causes of Haematemesis:
Oesophageal
- Reflux oesophagitis
- saton Oesophageal varices (portal hypertension)
- Oesophaeal tumours
- Mallory-Weiss mucosal tear
Gastric
- Gastric ulcer – usually benign
- Haemorrhagic gastritis
- Gastric varices
- Gastric cancer
Duodenum
- Delafoy lesion
- Duodenal ulcer
- Duodenitis
Clinical Features of Haematemesis
A. Symptoms:
1. History of peptic ulcer or other conditions which causes haematemesis
2. Vomiting out of blood: Fresh blood, bright red or coffee ground in colour.
3. Passes of black tarry stool.
4. Dryness of mouth and throat.
5. Blurring of vision,
6. Faintness.
B. Signs:
1. Features of volume depletion or shock:
- Cold and clammy skin.
- Rapid and thready pulse.
- Hypotension.
- Sweating.
- Decrease urinary output!
2. Progressive pallor.
3. Signs of dehydration :
- Sunken eyes.
- Dry tongue.
- Reduce elasticity of skin.
4. Local examination:
- Blood pressure is low.
- Epigastric tenderness.
5. Anaemia.
(Ref by-Lecture)
First Aid Management of Haematemesis
1. The patient should be immediately made to lie down.
2. Tight clothing around the neck, chest and wrist should be loosened.
3. Reassurance of the patient because if the vomiting is severe patient will be afraid.
4. The patient should be kept absolutely still and quite, any movement at all may increase the bleeding.
5. The patient should not be given anything by mouth.
6. Ice may be given to suck
7. This may be help to avoid nasty taste in the mouth.
8. Oxygen inhalation if the patient is in shock.
9. A doctor must be sent for to assess the extent of the bleeding.
10. Transport the patient to hospital further treatment.
(Ref by-Lecture)
Melaena.
Definition of Melaena:
In medicine, melena refers to the black “tarry” feces that are associated with upper gastrointestinal bleeding. The black color is caused by the hemoglobin in the blood being altered by digestive chemicals and intestinal bacteria.
(Ref by-en.wikipedia.org)
Melaena is the term used for black coal tar colored stool. It is caused due to passage of blood in stool. When iron from hemoglobin gets decomposed in intestine while passing through, it gives dark black color to the stool.
Or,
Melaena means passes of black stools. Blood passing through the intestinal canal is also altered black and tarry (sticky) stool.
Causes of Melaena:
Black stool or melena causes include
1. Peptic ulcer that includes stomach ulcer, duodenal ulcer.
2. Stomach cancer.
3. Patient on anti-coagulant drugs such as Warfarin may cause melena.
4. Gastritis (inflammation of stomach) and esophageal varices.
5. Hemorrhagic blood disease such as purpura.
6. Viral hemorrhagic fevers.
7. Gastroenteritis.
8. Gastritis.
9. Chronic viral hepatitis.
10. History of Smoking.
11. Swallowed blood as in case of nose bleeding can also give rise to melena.
12. Intestinal worms
Sign and Symptoms of Melaena:
A. Symptoms:
1. History of peptic ulcer or other conditions which causes melaena.
2. Passes of black and tarry stool.
3. Dryness of mouth and throat.
4. Blurring of vision.
5. Faintness.
B. Signs
- Features of volume depletion or shock:
- Cold and clammy skin.
- Rapid and thready pulse.
- Hypotension.
- Sweating.
- Decrease urinary output mod
2. Progressive pallor.
3. Signs of dehydration:
- Sunken eyes.
- Dry tongue.
- Reduce elasticity of skin.
4. Local examination:
- Blood pressure is low.
- Epigestric tenderness.
- Anaemia.
First Aid Treatment of Melaenaвич С
1. Ensure complete bed rest.
2. Tight clothing around the neck, chest and wrist should be loosened.
3. Reassurance of the patient because if the bleeding is severe patient will be afraid.
4. Close monitoring of:
- Pulse.
- Blood pressure.
- Central venous pressure.
- Urine output
5. The patient should be kept absolutely still and quite, any movement at all may increase the bleeding.
6. The patient should not be given anything by mouth.
7. Any specimen of stool or blood should be kept for inspection,
8. A doctor must be sent for to assess the extent of the bleeding.
9. Transport the patient to hospital further treatment.
Haematuria
Definition of Haematuria:
Hematuria is defined as the presence of red blood cells in the urine,
Or,
Passing of blood with urine from the urinary tract or bladder is called haematuria.
Or,
This term means blood in the urine. The blood may escape from vessels in the kidneys, the ureters, the urethra or the bladder.
Causes of Haematuria
There are many possible causes of hematuria, including:
A. Infection: cystitis, tuberculosis, prostatitis, urethritis, schistosomiasis, infective endocarditis.
B. Tumor: renal carcinoma, Wilms’ tumour, carcinoma of the bladder, prostate cancer, urethral cancer or endometrial cancer.
First Aid Management of Haematuria:
1. The patient should be advised to go to bed and kept quiet and still
2. Keep patient warm
3. A doctor should be sent for to assess the situation
4. Give plenty of fluid by mouth
5. A specimen of urine should be kept for inspection by the doctor.