All About Wound – Basic microbiology, parasitology, and immunology; nature, reproduction, growth, and transmission of common microorganisms and parasites in Bangladesh; prevention including universal precaution and immunization, control, sterilization, and disinfection; and specimen collections and examination. Students will have an understanding of common organisms and parasites caused human diseases and acquire knowledge about the prevention and control of those organisms.
All About Wound
Definition of Wound
wound is a type of injury which happens relatively quickly in which skin is torn, cut, or punctured (an open wound), or where blunt force trauma causes a contusion (a closed wound).
Or,
Wound may be defined as a breach in anatomical continuity of any living tissue due to any violence. (Such as injury or trauma)
Or,
A wound is the break of natural continuity of any of the tissues of the living body, produced by trauma,
Classifications of Wound:
A. According to rank and Wakefield:
a) Tidy wounds: Tidy wounds are inflicted by sharp instrument and contain no devitalized tissue. Example: Surgical incisions and cuts from glass or knives
b) Untidy wound: Untidy wound result from crushing, tearing, avulsion, vascular injury or burns and will contain devitalized tissue

B. According to level of contamination, a wound can be classified as:
a) Clean wound-made under sterile conditions where there are no organisms present, and the skin is likely to heal without complications.
b) Contaminated wound usually resulting from accidental injury, there are) pathogenic organisms and foreign bodies in the wound.
c) Infected wound the wound has pathogenic organisms present and multiplying, exhibiting clinical signs of infection (yellow appearance, soreness, redness, oozing pus).
d) Colonized wound – a chronic situation, containing pathogenic organisms, difficult to heal (i.e. bedsore).
C. According to Duration/Type of wounds:
a) Acute wounds:
- Closed wounds:
✓ Bruise/contusion
✓ Haematoma
- Open wounds:
✓ Bites and puncture wounds
✓ Abrasions and friction burns
✓ Laceration (sharp and bursting type)
b) Complex wounds:
- Crush avulsion
- Internal organs injury
- War wounds and gunshot injuries
- Tissue loss
c) Injuries to special tissues:
- Fat, muscle, bones and joints
- Nerves, arteries and veins
d) Chronic wound:
- Ulcers
- Pressure sores
D. According to surgical management/Visibility:
a) Closed wounds:
- Bruise
- Ecchymosis
- Hematomas
- Contusion
b) Open wounds:
- Abrasion
- Laceration
- Incised
- Penetrating
- Perforating
E. According to infectivity:
a) Infected wound
b) Non- infected wound
F . According to cleanliness:
a) Clean wounds
b) Clean-contaminated wounds
c) Contaminated wounds
d) Dirty and infected wounds
G. According to thickness of skin loss:
a) Superficial epidermal
b) Partial-thickness
c) Full-thickness
Purposes of Wound Care:
- To protect the wound from contamination with microorganism
- To promote wound granulation and healing.
- To support or splint the wound and healing.
- To promote thermal insulation to the wound surface.
- Keep the wound moist and therefore enhance epithelialization.
- Clean the wound or keep it clean.
- Control the bleeding by putting direct pressure on the wound.
- To promote wound granulation and healing
- To keep the edge of the wound in close approximation.
- To immobilize the affected area.
- To absorb secretions being discharged from the wound.
- To provide for maintenance of high humidity between the wound and dressing
- To promote physical, psychological and aesthetic comfort.
Definition of Surgical Wound:
A surgical wound is a cut or incision in the skin that is usually made by a scalpel during surgery. A surgical wound can also be the result of a drain placed during surgery. Surgical wounds vary greatly in size. They are usually closed with sutures, but are sometimes left open to heal.
Classification of Surgical Wound
Class I – Clean surgical wounds : Clean surgical wounds show no signs of inflammation and do not involve the respiratory, gastrointestinal or genitourinary tracts. Laparoscopic surgeries, surgeries involving the skin (such as biopsies), eye or vascular surgeries are good examples.
Class II-Clean- contaminated : Clean-contaminated wounds are clean wounds with a higher risk of infection such as those involving the gastrointestinal, respiratory or genitourinary tracts, as long as the surgery is uncomplicated. Any wound opened to remove pins or wires, chest procedures, ear surgeries or gynecologic procedures are considered class II surgical wounds.
Class III – Contaminated wounds : Contaminated wounds are created when an outside object comes in contact with the wound. This could be a bullet, knife blade or other pointy object. Or the contamination could be caused by large amounts of spillage from the GI tract into the wound. Any highly inflamed or infected tissue around a surgical wound is considered contaminated.
Class IV – Dirty- infected surgical wounds : Dirty-infected surgical wounds include those with a foreign object lodged in the wound (such as a bullet or other debris). This class also includes traumatic wounds from a dirty source where the treatment was delayed, infected surgical wounds or any wound that has been exposed to pus or fecal matter.
Signs and Symptoms
- Surgical wounds are monitored closely for infection. Signs that a surgical wound is infected include:
- Redness around the wound
- The skin around the wound is hot to the touch
- Drainage that is cloudy, discolored or foul smelling
- Swelling
- Fever
- Increased pain to the area
- The wound is larger or deeper
Important Complication of Surgical Wound:
A. Local effect:
a. Mechanical:
- Hemorrhage
- Haematoma formation
- Deformity
- Loss of function
- Retraction of tissue
b. Biological response:
- Cellular response/Inflammatory response
- Vascular response
- Neural response
- These lead to localized swelling
B. General effect:
- Shock
- Fever due to pyrogen (IL=1, TNF)
C. Secondary effect:
- Wound infection due to gap
- Wound abscess
- Bacteraemia
- Septicemia
- Gas gangrene
- Scarring due to tissue loss
- Contracture
- Wound disruption
- Hypertrophic scar
- Keloid formation
Definition of Wound Healing:
Healing is the process that follows disruption of normal tissue integrity and takes place in tissue which is physically sundered or only changed chemically
Factors Affecting Wound Healing
Factor divided into 3 types:-
A. Local factor
a) Local infection:- delay healing
b) Location:- size and type of wound
c) Blood circulation and blood vessel status.
d) Presence of necrotic tissue and foreign bodies
e) hematoma formation
f) nerve supply
g) previous radiation
h) Ionizing radiation
i) Tissue tension
j) Irritation
k) pressure
i) Foreign bodies such as unnecessary sutures or fragments of steel, glass or even bone constitute impediments to healing
m) Bacteria: bacterial infection causes delay in healing.
n) Mechanism of wound:
- Incision
- Crush
- Crush avulsion
B. Systemic factor
a) Age:-
- Old – slow
- Young – rapid
b) Nutrition :-
- Protein malnutrition
- Vitamin A deficiency
- Vitamin C deficiency
- Vitamin D deficiency
- Vitamin E deficiency
c) Trace metal :-
- zinc, calcium, copper and, magnesium
d) Drug, eg steroidb
C. Systemic disease
a) anemia
b) systemic infection
c) diabetes mellitus
d) granulocytopenia
e) bleeding disorders
f) uremia
g) malignant disease
h) AIDS, jaundice, septicemia, obesity, temperature
Types of Wound Healing:
There are three type of wound healing
1. Healing by first intension
➤ Features:
- Clean cut and incisional wound
- Not contaminated
- Good vascularity
- Less skin loss (Well approximately by suture)
- No or minimum scarring
2. Healing by second intension
➤ Features:
- Open wound
- Infected (contaminated)
- Less vascular tension
- More skin loss
- Maximum scarring
3. Healing by third intension
➤ Features
- Deep seated heavily contaminated wound
- Open infected no stitching
- Only partially closed and kept open
- wound is closed by secondary suture or skin grafting after granulation tissue is formed skin graft in needed as such a large epithelial defect won’t be filled by epithelium alone
- Initially there is a yellow covering. Later (5-6 days) as, there is bright red color due to revascularization within the granulation tissue
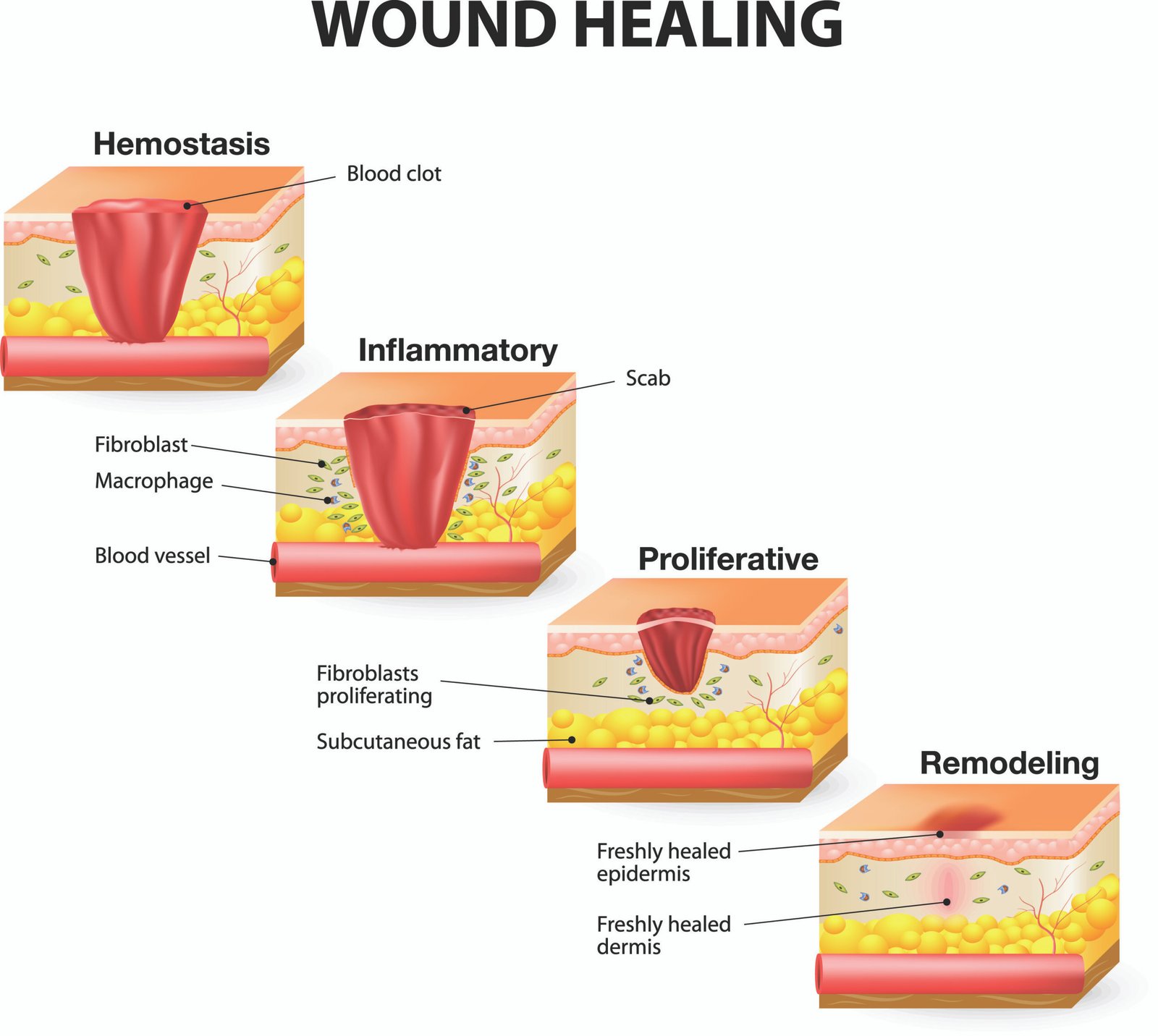
Stages of Wound Healing:
Haemostasis
Inflammation – Neutrophils aggregate
Macrophage – clean up tissue debris
Neo-vascularization
Fibroblast growth
Synthesis of collagens and proteoglycans
Remodeling
Definition of Wound Dressing:
Cleansing a wound or incision and applying sterile protective covering using aseptic technique is called dressing.
Types of Wound Dressing:
A. Open dressing: The antimicrobial cream is applied with a gloved hand and the wound is left open to the air without gauze dressing. The cream is reapplied as needed.
➤ Advantages:
- Increase visibility of the wound
- Freedom for joint mobility.
➤ Disadvantages:
- Increased chance of hypothermia
B. Closed dressing: In closed method, gauzed dressing is impregnated antimicrobial cream and applied to the wound.
➤ Advantages:
- Decrease in evaporative fluid and heat loss from wound surface.
- Gauze dressing aids in debridement.
➤ Disadvantages:
- Mobility limitation.
- Wound assessment is limited
Purposes of Dressing:
1. To protect the wound from contamination with microorganism.
2. To promote wound granulation and healing.
3. To support or splint the wound and healing.
4. To promote thermal insulation to the wound surface.
5. Keep the wound moist and therefore enhance epithelialization.
6. Clean the wound or keep it clean.
7. Control the bleeding by putting direct pressure on the wound.
8. To promote wound granulation and healing.
9. To absorb secretions being discharged from the wound.
10. To provide for maintenance of high humidity between the wound and dressing.
11. To promote physical, psychological and aesthetic comfort,
Or
Dressing is a protective covering on a wound. Dressing may be used for the following reasons:/
1. Keeping the wound clean.
2. Absorbing drainage
3. Controlling bleeding
4. Holding medication in place
5. To assess the healing process.
6. To cover the wound and protect it from microorganisms or mechanical trauma.

Procedure of Wound Dressing:
A. Equipment’s:
a) Sterile dressing tray container:
- Artery forceps 1 (2 for extensive or infected wounds).
- Thumb forceps – 1.
- Cotton swabs
- Gauze pieces.
- Gallipot for cleansing solution.
- Surgical pads.
- Kidney tray.
- Sterile scissors.
b) A clean tray container:
- Clean gloves.
- Sterile gloves.
- Cleaning solution (normal saline).
- Ordered medications.
- Adhesive plaster.
- Bandage scissor.
- Plastic nag
- Waterproof pad or mackintosh.
- Culture tubes
B. Procedure:
1. Identify the patient.
2. Inform patient of dressing change, explain procedure and have patient lie in bed.
3. Gather equipment and arrange at the bedside.
4. Wash hands.
5. Check physicians order for dressing changes and any specific instruction.
6. Close door or curtains order for dressing change and any specific instruction.
7. Assist patient to comfort position that provides easy access to wound area.
8. Place opened, cuffed plastic bag near working area.
9. Looses tapes on dressing (if tape is soiled, don clean gloves before loosening the
tape)
10. Don clean disposable gloves and remove soiled dressings carefully from more clean to less clean area.
11. Assess the amount, color and odor of drainage.
12. Discard dressing in disposal bag. Pull off gloves inside out and discard in appropriate respectable.
13. Using sterile technique, open sterile dressing tray and arrange supplies on work area.
14. Open cleaning solution and pour into the sterile galipot / cup over the work area.A
15. Don sterile gloves.
16. Pick up soaked cotton using artery forceps.
17. For a surgical wound clean from top to bottom or from center outward.shole (
18. Dry the wound using sponge in same motion.
19. Apply medication as ordered.
20. Place sterile gauze slit on side under and around the drain.
21. Apply a second layer of gauze to wound site and surgical pad as the outer most layer.
22. Remove gloves.
23. Wash reusable articles to be sent for sterilization
24. Wash hands.
25. Record dressing change, appearance of wound and describe any drainage in the chart.
The management of crush injury of foot or hand.
A. Immediate management
a) Resuscitation
- Airway-clearance, suction.
- Breathing-active management.
- Circulation-secure an IV channel; send blood for grouping and. cross matching.
- Breaks-split.
- Bleeding-pressure/bandage/tourniquet.
b) Diagnosis and assessment
- Short history
✓ Particulars of the patient.
✓ Where, when and how (time, nature, and mode of injury) the injury was happened.
- Physical examination
✓ Type of injury.
✓ Severity of injury-structures injured.
✓ Contamination of injury-foreign body, blood clot etc.
- General examination: Pulse, BP, Temperature, Respiration, Anaemai,
Dehydration, Heart, Lungs, Urine output.
Systemic examination:
✓ Examination of the wound -site, size, shape, active bleeding, contamination..
✓ Exam of other system.
- Investigation: X-ray to exclude fracture or dislocation.
B. Treatment:
- Removal of clothes from the area and clean the adjacent site of the wound by tap/cold water.
- Then clean the wound with sterile normal saline properly and thoroughly
- Removal of devitalized tissue and FB (foreign bodies)
- If profuse bleeding-stop bleeding by clamping (artery forceps) and ligation of bleeding vessels
- Prevention of infection by appropriate antibiotics and tetanus toxoid
- Examine the wound to see which structures are involved
- Wound excision or debridement (under appropriate anesthesia)
✓ Skin-damaged skin is cut to make the wound margin regular with facilitates healing and suturing.
✓ Muscle-Dead or non-viable muscle are removed
✓ Vessel-are either repaired or ligated by diathermy coagulation.
✓ Tendon and nerves -if inured repaired
- Repair of the wound
✓ Clean wound less than 6 hours-closure by primary suture.
✓ Grossly contaminated wound of <6 hours.
- Should not be closed first.
- Wound is cleaned and debrided and give stitch but no knot,
- Covered with gauze and bandage
- Examine after 24 hours: If no oozing, edema subsides, wound closure by delayed primary suture, keeping a drain and primary skin graft.
✓ Infected wound > 12 hours
- Must always keep open under dressing for 14 days
- Closed by secondary suture and secondary skin graft (after granulation tissue formation)
Post-operative order
✓ Antibiotic and analgesic
✓ Remove the stitch after 7 days