Definition of Immobility – An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Definition of immobility:
Immobility means not moving or unable to move or work or standing still and disinclined to move, as in an animal suddenly blinded; responds to other stimuli unless immobility is part of a dummy syndrome when all stimuli are ignored.
Or
Any disease or disability that requires complete bed rest or extremely limits our activity is considered immobility. Patients who have had a stroke resulting in partial or complete hemi paresis / paralysis, spinal cord injury resulting in paraplegia or quadriplegia, fracture, or prolonged bed rest after surgery are considered immobilized.
Immobility occur due to the following causes / reasons:
1. Neurological disorder :
i. Parkinson’s disease.
ii Stroke.
iii. Others such as cerebellum dysfunction neuropathies, ex
iv. Due to treatment-post operative.
2. Musculoskeletal disorder:
i. Due to pathology i.e. Arthritis.
ii. Osteoporosis,
iii. Due to traumatic injury i.e. multiple type of fracture, spinal cord injury
iv. Due to treatment-post operative.
3. Cardiovascular disorder:
i. Congestive cardiac failure,
ii. Coronary artery disease( MI, Angina),
iii. Peripheral vascular disease, iv. Berger disease(male), Raynauds disease(female)
4. Pulmonary disorder:
i. Chronic obstructive lung disease (COLD).
ii. Pleural effusion.
iii. Pneumothorax
5. Sensory disorder:
i. Impairment of vision,
ii. Fear from instability and fear of falling.
6. Environmental factors;
i. Force immobility,
ii. In educate aids for mobility.
7. Other factors:
i. Patient with cast (plastering), traction, fracture spine,
ii. Acute or chronic pain,
iii. Severe or critically ill patient,
iv. Depression.
V. Drugs side effects,
vi. Others such malnutrition.

Adverse effect of immobility:
1. Effects on musculoskeletal system:
i. Muscle atrophy( Shrinkge of cell size).
ii. Decreased muscle strength and tone.
iii. Decreased mass.
iv. Contracture-(a shortening of the muscle).
v. Stiffness and pain of the joint (collagen tissue “ankylosis”).
vi. Osteoporosis (effect in immobility).
2. Effects on cardiovascular system;
i. Increased heart rate (Tachycardia),
ii. Dependent oedema (Increased venous pressure); noted in sacrum and heels, feet and ankles) when up in chair.
iii. Venous thrombosis (pooling of blood and damaged vessels),
iv. Orthostatic hypotension (Drop in systolic BP by 15 mmHg, Drop in diastolic BP by 10 mmHg.
3. Effects on respiratory system:
i. Pooling of secretions (rarely sighs, lack of coughing).
ii. Atelectasis (collapse of lobe or lung).
iii. Altered function of mucous membrane and cilia.
iv. Aspirate or hypostatic pneumonia.
4. Effects on metabolic system;
i.Negative nitrogen balance (increase catabolism).
ii. Negative calcium balance (Hypercalcaemia).
iii. Decreased Basal Metabolic Rate (anorexia),
iv. Pressure ulcer.
v. Delayed wound healing.
5. Effects on urinary system;
i. Urinary stasis.
ii. Urinary tract infection,
iii. Retention of urine,
iv. Renal calculi.
6. Effects on the gastrointestinal system;
i. Constipation.
7. Effects on the integument;
i. Reduce skin turgor.
ii. Skin break down.
8. Effects on psycho neurological system (Perception);
i. Social isolation,
iii. Decreased self esteem,
iv. Sensory deprivation,
v. Decreased self efficacy.
vi. Altered social role,
vii. Decreased learning & problem solving,
viii. Increase stress decreased in stress tolerance.
9. Rest and sleep pattern;
i. Altered sleeping pattern,
ii. Disorientation of time.
10. Sexually pattern:
i. Altered sexually functioning.
Risk for developing complication of immobilize patient: Risk for developing complications during immobility’s are:
1. Age.
2. Level of immobilization.
3. Level of conscious.
4. Degree of impaired neurovascular function or underlying diseases.
5. Risk assessments:
- Health history.
- Sign & symptoms.
- Physical examination.
- Laboratory.
- Screening tools such as pressure ulcer risk assessment tool.
Risk Assessment:
| System | Assessment |
| 1. Musculoskeletal system |
|
| 2. Cardiovascular system |
|
| 3. Respiratory system |
|
| 4. Metabolic system |
|
| 5. Urinary system |
|
| 6. Gastrointestinal system |
|
| 7. Integumentary system |
|
| 8. Psychological system |
|
Prevent or decreased adverse effects:
1. By repositioning.
2. Using supported devices.
3. Promote exercise.
4. Nutritional support
5. Social support.
Management of adverse effect of immobility:
A. Cardiovascular system;
1. Decrease cardiac out put & cardiac workload.
2. An in cased rate in the coagulation of blood. During periods of immobility, calcium leaves bones and enters the blood, where it has an influence on blood coagulation.
3. Orthostatic hypotension probably due to a decrease in the neurovascular reflexes, which normally causes vasoconstriction, and to a loss of muscle tone. The result is that blood pools and does not squeeze from veins in the lower part of the body to the central circulatory system. The immobilize person is more susceptible to developing orthostatic hypotension. The person tends to feel weak and faint when the condition occurs.
B. Respiratory system:
1. Hypostatic pneumonia. The depth and rate of respirations and the movement of secretions in the respiratory tract is decreased when a person is possible. The pooling secretions and congestion predispose to respiratory tract infections.
2. Atelectasis. When areas of lung tissue are not used over a period of time, incomplete expansion or collapse of lung tissue may occur.
3. Increasing coughing mechanism may be due to the patient’s position in bed.
C. Musculoskeletal system:
1. Muscle atrophy. Disuse leads to decreased muscle size, tone and strength.
2. Contracture. Decreased joint movement leads to permanent shortening of muscle tissue, resistant to stretching. The strong flexor muscles pull tight, causing a contraction of the extremity or a permanent position of flexion.
3. Ankylosis. Consolidation and immobility of a joint in a particular position due to contracture. 4. Increase in calcium absorption, weakening the bone.
D. Gastrointestinal system:
1. Decreased activity resulting in anorexia.
2. Utilization of nutrients resulting in constipation.
3. Increase protein metabolism.
E. Urinary system:
1. Decreased bladder muscle tone resulting in urinary retention.
F. Metabolism:
1. Increased risk of electrolyte imbalance. An absence of weight on the skeleton and immobility causes protein to be broken down faster than it is made, resulting in a negative nitrogen balance.
2. Decreased metabolic rate.
G. Psychosocial functioning:
1. Increase concept and increase in sense of powerlessness due to inability to move purposefully and dependence on someone for assistance with simple self-care activities.
2. Increase sensory stimulation.
3. Increase social interaction.
Risk factors of immobility:
It is a major nursing responsibility to prevent the complications of immobility. Hence, the nurse needs to identify patients at risk of developing such complications before they arise.
Patients at risk include those who:
1. Are poorly nourished.
2. Have decreased sensitivity to pain, temperature or pressure.
3. Have existing –
- Cardiovascular problem.
- Pulmonary problem.
- Neuromuscular problems.
4. Unconscious.
[Ref-SN Nanjunde Gowda’s “Foundations of Nursing” 1″ edition page-221]
Complications of immobility:
Prolonged immobility can cause complication with all body systems. Common complications of immobility are given in the below according to the different system with their abnormal finding:
1. Metabolic system:
- Slowed wound healing.
- Muscle atrophy.
- Decreased amount of subcutaneous fat.
- Generalized edema.
2. Respiratory system:
- Asymmetrical chest wall movement.
- Dyspnea.
3. Cardiovascular system:
- Increased respiratory rate.
- Orthostatic hypotension.
- Increased heart rate.
- Third heart sound.
- Weak peripheral pulses
- Peripheral edema.
4. MusculoskeJetal system :
- Decreased ROM.
- Erythema.
- Increased diameter in calf or thigh.
- Joint contracture.
- Activity intolerance.
- Muscle atrophy.
5. Skin:
- Break in skin integrity.
6. Elimination:
- Decreased urine output.
- Decreased frequency of bowel movements.
- Distended bladder and abdomen.
- Decreased bowel sounds.
[Ref-SN Nanjunde Gowda’s “Foundations of Nursing” 1″ edition page->221-2]
Prevention of bed sore in an immobile patient :
1. Find out and detect the patients who are prone to bed sores.
2. Daily observation of the pressure points and prompt reporting in case of suspicion.
3. Stimulate circulation by cleaning and back care especially pressure areas and massage of all areas exposed to pressure.
4. Provide Proper Positioning: Positioning interventions prevent the adverse effects of pressure, friction, and shear. For most clients, maintaining current activity levels, mobility, and range of motion are sufficient to prevent pressure ulcers. For the immobilized client, the following interventions may help prevent the development of pressure ulcers:
a. Turn and reposition the client at least every 1 to 2 hours so ischemic areas can recover. If a reddened area does not blanch when pressed, turn the client more often.
b. When positioning, pay attention to body alignment. The position relieves pressure on the sacrum and trochanters. There should be a 30 degree angle between the client’s trochanters and the surface of the bed. The hips and knees should be flexed. To maintain this position, support the client’s back with a pillow or foam wedge, and put a pillow between the knees.
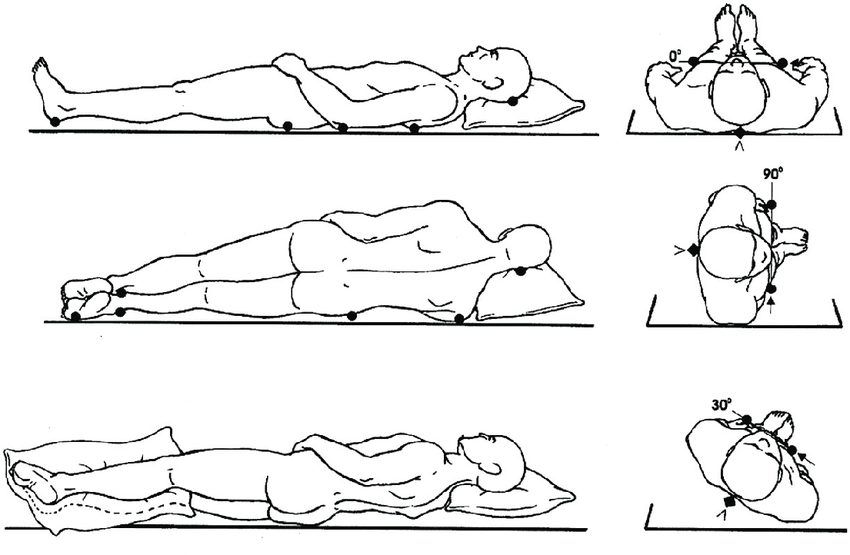
c. When turning the client, remove the pillows and wedges, lower the head of the bed, and use a draw sheet to lift, not drag, the client to a new position. Maintain the head of the bed at 30° or less to prevent shearing.
d. If the client is supine, make sure the heels are not resting on the mattress. Suspend them by placing a pillow or foam pad lengthwise under the lower legs.
e. Place at-risk clients on pressure-reducing surfaces.
f. Have clients who are able to sit up shift their weight every 15 minutes; those who cannot do so need to be repositioned at least every hour.
g. Use a pressure-reducing device such as a foam overlay on the seating surface to reduce pressure on the ischial tuberosities by redistributing weight over a much larger surface area. Do not use donut-shaped cushions, which reduce blood supply to the affected area, leading to even more ischemia.
5. Relative pressure by:
a. Frequent movement of helpless patient in bed changing the position 2 hourly.
b. By using comfort devices, take off pressure from the pressure points e.g. air cushions, air rings etc.
c. Avoid the use of rubber rings.
d. Use a bed cradle to take the weight of the linen especially children having rheumatic fever.
e. Use pillow between legs. Don’t allow two bony prominences meet the patient.
f. Early ambulation of the patient.
g. Use of Dunlop mattress for equal distribution of the weight of the patients body on the mattress.
h. Padding pressure points inside plaster casts.
i. Loosing tight bandages.
j. Allow the patient to get up and walk about as soon as possible.
6. Avoid friction by :
a. Making a proper bed without crumbs or wrinkles. Tightly tucked beds are used.
b. Do not badly chipped or rough bed pans.
c. Use adequate amount of cotton under splints and plaster casts to avoid friction.
7. Avoid moisture :
a. Immediate and proper changing left wet linen.
b. Absolute cleanliness and dryness of the skin.
c. After each urination and detection give back care.
d. Special care should be taken during the patient’s urination and defection to prevent soiling of bed linen.
e. Wipe off perspiration and keep the patient dry.
8. Prevent injury by:
a. Cutting nails short of bath, nurses and patients.
b. Taking special care while giving and removing bed pan to avoid scratching skin. Better to use steel bed pan.
d. If splints are used these should be well padded.
c. Help should be taken while moving heavy and difficult while moving heavy and difficult patients.
Pathogenic organism prevent by –
a. Bed should be kept neat and tidy.
b. Personal hygiene should be maintain.
c. Regular back care.
10. Diet: Diet should be well balanced with lots of proteins and plenty of vitamins. It will help the tissues remain healthy and reduce the risk bed sores: Vitamin C is good for healing.
11. Fluid: Plenty of fluid should be given to the patient, restricted according to disease condition only.
[Reference: Fundamentals of Nursing, Annamma Jacob,Vol-1, P-92-94+ Lecture]
Definition of exercise :
Exercise is any physical activity involving muscles that elevates the heart rate above its resting level. Exercise reduces joint pain and stiffness and increases flexibility.
Or
[Reference: Fundamentals of nursing, Sue C. DeLaune, Ed-4th, P-1091]
Physical exercise is any bodily activity that enhances or maintains physical fitness and overall health and wellness. It is performed for various reasons including strengthening muscles and the cardiovascular system, honing athletic skills, weight loss or maintenance, as well as for the purpose of enjoyment. Frequent and regular physical exercise boosts the immune system, and helps prevent the “diseases of affluence” such as heart disease, cardiovascular disease, Type 2 diabetes and obesity.
[Reference: en.wikipedia.org]
Types of exercise: Mainly it is two type. These are –
1. Fitness exercise (Physical activity performed by healthy adults): It develops and maintains cardio respiratory function, muscular strength and endurance. There are five categories of fitness exercise:
a. Aerobic: Improve cardiovascular fitness; assist with weight control; improve general functional ability. Example- rowing, jumping rope, walking, running.
b. Strengthening: Maintain or increase muscle strength. Example- weight training, calisthenics,
physical labor.
c. Isometric: Maintain muscle tone and strength. Example quadriceps setting, gluteal setting, triceps setting.
d. Isotonic: Increase and maintain muscle tone and strength; shape muscles; maintain joint mobility; improve cardiovascular fitness. Example weight lifting, working with pulleys, ROM exercises, performance of activities of daily living (ADL).aliba
e. Isokinetic: Condition muscle groups. Example exercise equipment and resistive water exercises.
2. Therapeutic exercise: (activity performed by people with health risk of those being treated for an existing health problem) are performed to prevent health related complications or to restore lost functions. Therapeutic exercise may be isotonic or isometric, isotonic exercise are performed actively or passively.
a. Active exercise (Therapeutic activity performed independently): It is performed after proper instruction. For example, patients who have undergone a mastectomy are taught to exercise the arm on the surgical side by combing their hair, squeezing a soft ball, finger climbing the vertical surface of a wall and swinging a rope attachment to a doorknob. Active therapeutic exercise is often limited to a particular part of the body that is in a weakened
condition. It is assumed that patients will use their unaffected muscle groups while performing activities of daily living such as bathing and dressing.
b. Passive exercise (Therapeutic activity performed independently): It is provided when a patient cannot move one or more parts of the body. For example, for comatose patients and those paralyzed from a stroke or spinal injury, nurses perform exercise that maintain muscle tone and
flexible joints. One form of passive therapeutic exercise that is frequently provided is range of motion exercises. Another is delivered with a continuous passive motion machine.
c. Range of motion (ROM):
i. Active range of motion: It performed independently by the client. During active ROM exercises, the client moves various muscle groups.
ii. Passive range of motion : Passive ROM exercises are done by the nurse to help maintain or restore a client’s mobility by achieving several outcomes, including the following:
- Prevent contractures
- Improve muscle strength and tone
- Increase circulation
- Decrease vascular complications of immobility
- Facilitate client comfort.
Benefits of physical exercise for immobility/bed ridden person :
The U.S. Surgeon General’s report Physical Activity Guidelines for Americans (U.S. Department of Health and Human Services, 2008) lists the following health benefits of exercise:
1. Lower risk of:
- Early death.
- Heart disease.
- Stroke.
- Type 2 diabetes.
- High blood pressure.
- Increased lipid levels.
- Colon and breast cancers.
2. Improve cardiovascular system.
3. Reduction of blood pressure.
4. Increase muscle tone and strength.
5. Greater physical endurance.
6. Reduction of elevated blood sugar.
7. Decrease low density of blood lipids.
8. Improve physical appearance.
9. Regular bowel elimination.
10. Better health function in older adults. to
11. Reduced abdominal obesity.
12. Weight maintenance after weight loss.
13. Lower risk of hip fracture.
14. Increased bone density.
15. Improved sleep quality.
16. Reduction in tension and depression.
[Reference: Fundamentals of nursing, Sue C. DeLaune, Ed-4th, P-1091+ Lecture]