Definition of Malaria – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Definition of Malaria
Definition of Malaria-Malaria is an infectious disease caused by plasmodium and transmitted by the bite of female anopheles mosquito, characterized by-fever, anemia, splenomegaly etc.
Or
Malaria is a protozoal disease caused by infection with parasites of the genus plasmodium and transmitted to man by certain of infected female anopheles mosquito.
Epidemiological Features of Malaria:
A) Agent factors:
- a) Agent: Malaria in man is caused by 4 distinct species of malaria parasite
- Plasmodium vivax
- Plasmodium falciparum
- Plasmodium malariae
- Plasmodium ovale
- b) Reservoir of infection: Human
- c) Period of communicability: Malaria is communicable as long as gametocytes exist in the blood to infect vector mosquito.
B) Host factors:
- a) Age: Malaria affects all ages
- b) Sex: Male are more exposed than female
- c) Social and economic factor: More in underdeveloped countries
- d) Housing: More in all ventilated and ill lighted house
- e) Pregnancy: The risk
- f) Occupation: More in agriculture practitioner
- g) Human habits sleeping out t of house and mosquito net
C) Environmental factors:
- a) Season: Maximum prevalence is from July to November
- b) Temperatures: eratures: 20°C -30°C
- c) Humidity: 60%
- d) Rain fall: Necessary for breeding
D) Mode of transmission:
- a) Vector transmission: Infected female anopheles mosquito
- b) Direct transmission:
- Blood transmission
- Infected needles
- Congenital-very very rare
E) Incubation period: Varies according to species –
- a) 12 (9-14) days for P. falciparum
- b) 14 (8-17) days for P. vivax
- c) 28 (18-40) days for P. malariae
- d) 17 (16-18) days for P. ovale

Classification of Plasmodium/Malarial parasites:
- Plasmodium vivax
- Plasmodium falciparum
- Plasmodium ovale
- Plasmodium malariae
species of plasmodium are common in Bangladesh
The following 2 species of plasmodium are more common in Bangladesh –
- Plasmodium vivax: common in plain land.
- Plasmodium falciparum: common in hilly areas.
Difference between P. Vivax & P. Falciparum:
| Traits | P. vivax | P. falciparum |
| Schizogony | 48 hours | 48 hours or under |
| Forms in peripheral blood | Trophozoites, schizonts and gametocytes. | Rings and crescents only. |
| Trophozoites- a) Ring form b) Growing form | Size, 2.5 micrometer, cytoplasm is thicker. | Size, 1.25 to 1.5 micrometer, cytoplasm is thinner. |
| Schizont (mature) | Irregular with a vacuole. | Assumes a compact form. |
| Merozoites | Size, 9 to 10 micrometer, regular. | Size, 4.5 to 5 micrometer. Fill two-thirds of a R.B.C. |
| Malarial pigments | 12 to 24, arranged in irregular grape-like cluster. | 18 to 24 or more, arranged in a grape-like cluster. |
| Infected R.B.C | Yellowish-brown, fine granules. | Dark-brown or blackish. |
| Gametocyte | Enlarged, pale, Schuffher’s dots present. | Usually unaltered, crenation, reddish violet colour and Maurer’s dots. |
| Spherical | Crescentic (banana-shaped) |
Clinical Types of Malaria and the Causative Plasmodium Parasites:
| Clinical types of malaria | Plasmodium parasite |
| 1. Benign tertian malaria |
|
| 2. Malignant tertian malaria |
|
| 3. Quartan malaria |
|

Dangerous Malaria;
Falciparum malaria is dangerous as
- They can infect both mature & immature RBC (reticulocytes). So, there is severe anaemia. On the other hand, other malaria species only infect immature RBC (reticulocyte).
- Falciparum shows resistance to common antimalarial drugs.
- Complications are higher and fatal, e.g. cerebral malaria, black water fever etc.
- Early diagnosis is difficult, so patient rapidly developed complications.
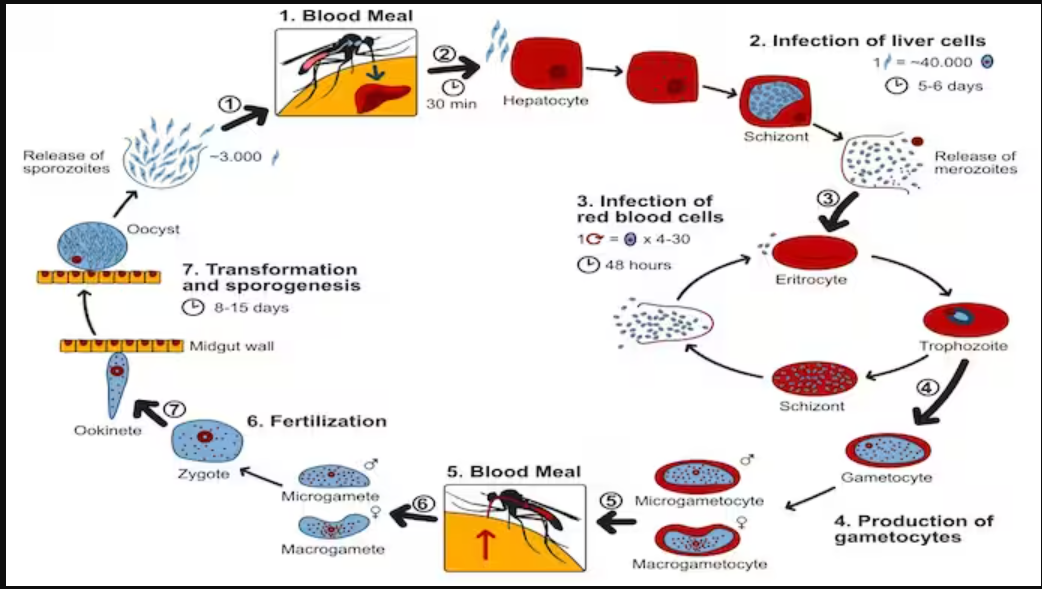
Life Cycle of Malarial Parasites:
➤Human cycle/ asexual cycle. –
➤ Mosquito cycle / sexual cycle.
Human cycle (Asexual cycle): 4 stages
- Pre-erythrocytic schizogony/hepatic schizogony; Mosquito bite→Sporozoites injected
to host spreads to surrounding tissue→ Peripheral circulation→Enter into liver
parenchyma→ Sporozoites become schizonts→ Rupture of schizonts→Liberation of→merozoites →
- Micromerozoites→ Enter into circulation.
- Macromerozoites→ Re-enter into liver cells.
- Erythrocytic schizogony; Micromerozoite enters into RBC→ Trophozoites→Schizont →
Rupture of schizonts → Liberation of merozoite → Attacks healthy RBC→ Cycle is repeated.
This phage is responsible for clinical attack of malaria.
- Gametogony: Some merozoites inside the RBC of capillaries of internal organs (spleen, bone marrow) develop into gametes→ Peripheral blood.
- Exo-erythrocytic schizogony: Except P. falciparum, in other species of Plasmodium, there is exo- erythrocytic schizogony. Because the tissue phage persists in the form of merozoites life cycle, parasite remains dormant of potentially infective to give rise infection to time (relapse).
Mosquito cycle (sexual cycle):
Female anopheles mosquito→ Blood meal→Macrogametocytes and microgametocytes are taken up→ Fertilization of macrogametes (round) by microgametes (long)→ Fertilized macrogamete (ookinete) in intestinal wall of mosquito→ Oocyst→ Meiotic & mitotic division → Sporozoites (100-1000) within Oocyst→ Rupture of Oocyst→ Release of sporozoites in the body cavity→ Through the circulation, the sporozoites are distributed to various organs & tissues, specially salivary gland & duct→ Bite→ Infection.
Figure: Life cycle of malaria parasite
The factors those are responsible for difficulties of malaria eradication
programme in Bangladesh are –
- Administrative failure:
- Shortage of finance, manpower, drugs, insecticides transport
- Shortage of administrative personnel’s
- Technical failure: Development of insecticides in vector and parasitic resistance to drugs
- Operational failure: Due to inadequate surveillance, case detection and treatment
- General failure:
- Common border of Bangladesh and India
- Sleeping without mosquito net
- Poor standard of environmental sanitation
- Lack of health education
- Epidemiological factors:
- Presence of extra-lumax reservoir of infection
- Presence of human carrier state
- Presence of sub clinical cases.

History:
- a) Patient may give H/O travel of malarious locality
- b) Onset is insidious with malaise, headache, vomiting
- c)
- No particular pattern
- Cold, hot and sweating stages are seldom found
- Not so high temperatures
- d) Cough and mild diarrhea
- e) Weakness
- f) Patient may present with complication of the disease
Patient may present with complication of the disease
- Unconsciousness
- Acute renal failure
- Black water fever
- Acute renal respiratory syndrome
- Septicemia
On examination (O/E):
- Patient anemia
- Jaundice may present
- Increase Temperature
- Hepato splenomegaly
Lab. diagnosis of malaria:
- A) Direct evidences
- Thick film: To detect the presence of parasite
- Thin film: To detect the species of parasite
- B) Indirect evidences:
- Serological test
- Blood for TC, DC, ESR, Hb%
- Liver function test
- Examination of urine

Signs Symptoms of Malaria:
- Paroxysms with shaking chills
- Rapidly rising fever with severe headache
- Profuse sweating
- Myalgia, with feeling of well-being in between
- Splenomegaly, hepatomegaly
- Orthostatic hypotension
- Paroxysms may last for 12 hours, then, maybe repeated daily or after a day or two.
- In children:
- Fever maybe continuous
- Convulsions and gastrointestinal symptoms are prominent
- Splenomegaly
- In cerebral malaria
- Changes in sensorium, severe headache, and vomiting
- Jacksonian or grand mal seizure may occur
Mode of Transmission:
- Vector transmission: Infected female anopheles mosquito
- Direct transmission:
- Blood transmission
- Infected needles
- Congenital-very very rare
- Incubation period: Varies according to species –
- 12 (9-14) days for P. falciparum
- 14 (8-17) days for P. vivax
- 28 (18-40) days for P. malariae
Complications of Malaria:
➤ Pernicious malaria: 3 types-
- Cerebral
- Algid
- Septicaemic
➤ Black-water fever due to intra-vascular haemolysis.
➤ Hypoglycaemia especially with quinine treatment.
➤ Lactic acidosis.
➤ Prolonged hyperthermia.
➤ Shock-Hypotensive or secondary to septicaemia.
➤ Pulmonary, cardiac, hepatic or renal dysfunction.
➤ Seizures.
➤ Spontaneous bleeding.
➤ Rupture of spleen.
➤ In pregnancy-Abortion, Stillbirth, Low birth weight and intrauterine death.
➤ Immunological disorders:
- Hyper-reactive malarial splenomegaly.
- Malarial nephrosis.
Recurrent Fever Pattern in Malaria:
➤ Recrudescence.
➤ Relapse

Recrudescence:
- It is the clinical manifestation which results from persistence of infection in blood.
- In case of P. vivax and P. ovale – recrudescence may occur due to inadequate drug therapy.
- In case of P. falciparum and P. malariae – It occurs due to drug resistance when a person’s immunity is destroyed. It is recorded to occur upto 40 years after original attack in case of P. malariae.
Relapse:
- It is the clinical manifestation results from persistence of blood infection and or persistence of exoerythrocyric forms in the liver in which erythrocytic schizogony commences again.
Treatment of Malaria:
- A) Uncomplicated malaria:
| Day | Drug and dose | Tablet | |
| 1st | Chloroquine (150 mg) | 4 tab. single dose once after meal | 600 mg |
| 2nd | Chloroquine (150 mg) | 3 tab. single dose once after meal | 450 mg |
| 3rd | Chloroquine (150 mg) | 3 tab. single dose once after meal | 450 mg |
| 4th | Primaquine 15 mg | 3 tab. single dose | 45 mg |
- B) Treatment of Chloroquine resistant mal-aria/Treatment failure mal-aria: In most areas of the world P. falciparum is now resistant to chloroquine.
| day | Drug and dose | Tablet | Total dose |
| 1st | Quinine 300 mg base | 2 tab. (8 hourly 3 times daily) | 600 mg |
| 2nd | Quinine 300 mg base | 2 tab. (8 hourly 3 times daily) | 600 mg |
| 3rd | Quinine 300 mg base | 2 tab. (8 hourly 3 times daily) | 600 mg |
| 4th | Quinine 300 mg base + Fansider | 2 tab. (8 hourly 3 times daily) + 3 tab. single dose 2 time daily | 600 mg |
On 8th day primaquine 15 mg single dose 3 tablet
- C) Severe mal-aria/cerebral mala-ria:
- Loading dose: Quinine dihydrochloride 20 mg/kg body weight by IV infusion
- Maintenance dose: After 8 hours
- Quinine salt: 10 mg/kg body weight, over 4 hours by IV infusion
- Maintenance dose should be continued 8 hurly until the patient can swallow tab tocomplete the 7 day course
- Fansidar single dose on the 3rd day
- Primaquine single dose on the 4th day
Pathogenesis of Malaria:
➤ The parasite enters the mosquito’s stomach through the infected human blood obtained by biting or during blood meal.
➤ The parasite undergoes sexual conjugation.
>>After 10 to 14 days, a number of young parasites are released which work their way into the salivary gland of the mosquito.
The organisms are carried in the saliva into the victim when the mosquito bites again.
➤ The female alone plays the role of a vector and definitive host in conveying the disease from man to man (sexual propagation).
➤In humans, the organisms invade the RBC where they grow and undergo sexual. schizogony.
➤ Erythrocytic merozoites are produced leading to the rupture of RBC upon the release of the tiny organisms.
➤ Young merozoites invade a new batch of RBC, to start another schizonic cycle.

Prevention & Control of Malaria:
- Measures to be applied by the individual:
- screening of houses
- Destruction of adult mosquitoes: Use of domestic space spray
- Destruction of mosquito larvae: Peri-domestic sanitation intermittent during of water container
- Source reduction: Small scale drainage system
- Measures against mal-aria parasite: Chemoprophylaxis and chemotherapy
- Measures to be applied by the community:
- Prevent of man/vector contact: Site selection and screening of houses
- Destruction of mosquito larvae: Using larvicides
- Source reduction: Prevention of manmade mal-aria environment sanitation water management
- Measures against ma-laria parasite: Presumptive treatment radical treatment mass drug administration.
Nursing Management of Malaria:
- The patient must be closely monitored.
- Intake and output should be closely monitored to prevent pulmonary edema.
- Daily monitoring of patient’s serum bilirubin, BUN creatinine, and parasitic com
- If the patient exhibits respiratory and renal symptoms, determine the arterial blood gas and
plasma electrolyte 3. During the febrile stage, tepid sponges, alcohol rubs, and ice cap on the head will help bring the temperature down.
- Application of external heat and offering hot drinks during chilling stage is helpful.
- Provide comfort and psychological support.
- Encourage the patient to take plenty of fluids.
- As the temperature falls and sweating begins, warm sponge bath maybe given.
- The bed and clothing should be kept dry.
- Watch for neurologic toxicity (from quinine infusion) like muscular twitching, delirium, confusion, convulsion, and coma.
- Evaluate the degree of anemia.
- Watch for any signs especially abnormal bleeding.
- Consider severe ma-laria as medical emergency that requires close monitoring of vital signs.
Black Water Fever:

Definition: It is a manifestation of falciparum ma-laria occurring in previously infected subjects and is characterized by sudden intravascular haemolysis followed by fever and haemoglobinuria Etiology; It is associated with infection by P. falciparaum, most commonly observed among th non-immune individuals who have resided in endemic zone for 6 months to 1 year and have ha inadequate doses of quinine for both prophylaxis and treatment.
Pathogenesis: Intravascular haemolysis.
Mechanism:
Extensive intravascular haemolysis
↓
Breakdown of RBC and excessive release of Hb in blood.
↓
Saturation of haptoglobin (Hb binds with haptoglobin)
↓
Free Hb (unable to bind)
↓
Clinical manifestation.
Pathology:
➤ Kidney:
- Large and dark in colour.
- Degenerative changes in DCT and blocked with Hb casts.
➤ Liver: Enlarged, soft and stained intensely yellow.
➤ Gall bladder:
- Filled with dark green viscid bile.
➤ Spleen: Enlarged.
Clinical features:
- Fever and rigor, followed by aching pains in the loins.
- Haemoglobinuria.
- Icterus.
- Bilious vomiting.m man
- Circulatory collapse.
- Acute renal failure.
Complications:
- Renal failure (uremia).
- Acute liver failure.
- Circulatory collapse.
↓
Micro-thrombus formation
↓
Blockage of capillary blood vessels of brain
↓
Ischaemia
↓
Hypoxia
↓
Necrosis, hemorrhage and edema in brain
↓
Loss of consciousness.
Causes of Anaemia in Malaria:
- Mechanical lysis of infected RBC (Haemolysis).
- Immune mediated lysis of both normal and infected RBC due to production of antibody against RBC (Autoimmune haemolytic anaemia)
- Splenomegaly causes RBC sequestration and lysis.
- Dyserythropoiesis due to affected bone marrow.
- Depletion of folic acid.
- Phagocytosis of uninfected erythrocytes.
- Antimal-arial drug (primaquine) in gluose-6-phosphate dehydrogenase deficiency.
Read more:
