Medical Definition of Fracture -An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Medical Definition of Fracture
A fracture is a partial or complete disruptions of the normal continuity of bone.
[Ref-Luckmann and Sorensen, Medical and surgical nursing, 2nd edition,1684]
Or
Fracture is a break in the surface of a bone, either across its cortex or through its articular surface.
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4th edition page-15]
Or
A fracture is a break in the structural continuity of bone.
[Ref- Apley’s “System of Orthopaedics and Fractures” 9th edition page-688]
Or
A fracture is the partial or complete breakage of periosteum (bone).
[Ref-L.C. Gupta’s “Manual of First aid” 1″ edition page-147]
Or
Fracture may be defined as any structural breach in natural continuity of bone and cartilage.
[Ref-Baily & loves Short practice of surgery, 25th edition.page-455]
Or
A fracture is a break in the continuity of a bone.
[Ref- lippincott, Adult orthopedic nursing, 1st edition.page-86]
Classification of fracture:
A) Etiological classification:
1) Traumatic fracture – Due to sudden injury.
2) Pathological fracture- Bone is weakened by a diseases. e.g. TB, Osteomyelitis.
3) Stress fracture – Due to repeated minute trauma at the same site. e.g. Infantry soldiers may suffer from stress fracture due to long hikes.
B) Clinical classification (according to communication with exterior):
1. Simple or closed fracture: The fracture which is not communicated with exterior. (No risk of
infection or osteomyelitis).
2. Compound or open fracture: When the fracture fragment has communications with exterior and skin over the injured site is broken.
C) Radiological (according to the configuration of the fracture
or
according to direction of force/Shape of fracture):
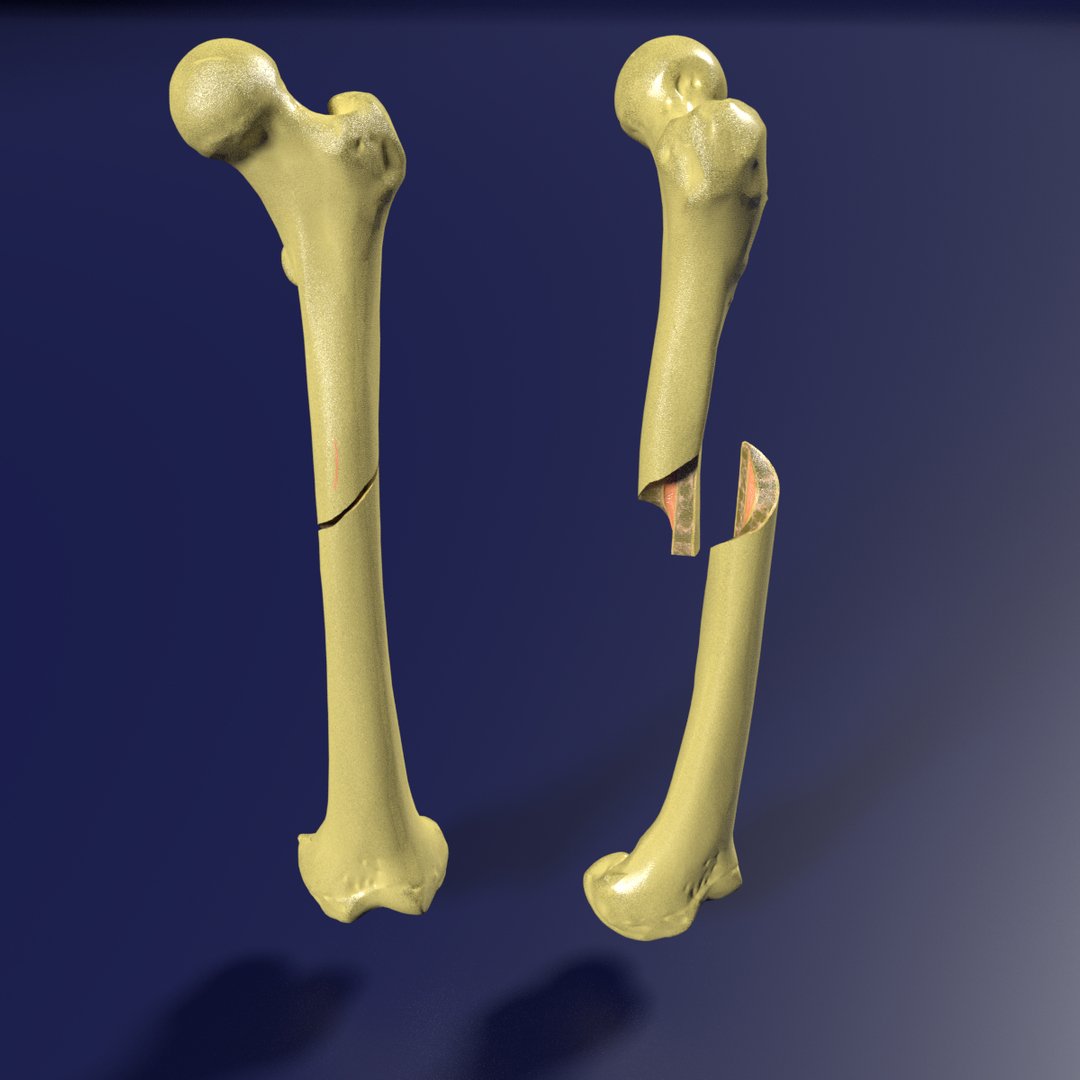
1. Transverse fracture – by angulations force. (An angle <30 degreee with horizontal line)
2. Oblique fracture – by twisting force. (An angle 30 Degree with horizontal line)
3. Spiral fracture – by twisting force.
4. Z-fracture by angulations plus resistance force.
5. Comminuted fracture – more than two fragments by angulations force or crushing force or direct force. Bone is broken in several place.
6. Wedge fracture – in vertebral body by vertical force.
7. Avulsion fracture – a small fracture fragment in pulled and shifted by the attached muscle, e.g. fracture epicondyle.
8. Depressed fracture – by direct violence e.g. skull bone.
9. Impacted fracture – by the force along the axis of bone, The end of the bone are pushed into one another. e.g. fracture neck.
10. Burst or shattered fracture – multiple small fragment, separation. In spongy bone e.g. body of vertebra, patella, talus and calcaneous.
D) According to involvement of joint capsule :
1 ) Intracapsular: Within the joint capsule.
2) Extracapsular: Outside the joint capsule.
E) According to extent of fracture:
1) Incomplete fracture: Only one portion of the bone is broken. It involves one surface or cortex of bone.
2) Complete fracture: Fracture involves entire bone.
F) According to involvement of vital structures.
1) Simple: Fracture is not involved with the injury to vital structures.
2) Complicated: The fracture involving the vessels, nerve & vital organs during the initial injury. E.g.: of the skull where broken bone may pierce the brain.
G) According to cortical involvement of bone:
1) Complete: Fracture of both sides of the cortex.
2) Green stick: Involvement of one side of cortex of bone, other side remains normal.
[Ref-Dr. Redhwan’s “Royal Surgical Handicraft”, 2nd edition page-392, 393]
Mechanisms of fracture:
Bone is relatively brittle, yet it has sufficient strength. Mechanisms of fractures depends on 3 way:
A. Injury.
B. Repetitive stress.
C. Pathological condition in bone(Pathological fracture).
A) Injury: Most fracture are caused by sudden and excessive force which may be direct or indirect.
1. Direct Force: When direct force is given at the point of impact. It decrease the bone strength. Then the periosteum and inner side of the bone breaks at the point of force. A direct force usually split the bone transversely. If crushing occurs, the fracture pattern will be comminuted with extensive soft tissue damage.
2. Indirect force: Some bone breaks some distance away from the areas where the force or violence has been applied. Due to indirect forces condition arises in bone such as-
a) Twisting causes- Spiral fracture.
b) Compression causes- Short oblique fracture.
c) Bending causes – Butterfly fragment.
d) Tension on bone transverse fracture.
B) Repetitive stress:
Bone will break down due to repetitive loading of the bone. Continuous loading of bone decrease bone strength causing fracture.
C) Pathological fracture:
Pathological fracture caused by weakening of bone due to pathological conditions of patients
|
Decrease bone strength.
|
Simple trauma or fall from height give pressure on the weakening site of bone.
|
Pathological fracture
[Ref- Apley’s “System of Orthopaedics and Fractures” 9th edition,page-687,688]
Causes of fracture:
A) Due to violence or forces :
1) Direct violence or force- Bone can be fractured directly at the point where the force or violence of a blow
is applied. For example:
- of the skull can occur if the person is hit directly on the head or
- of the bones of leg if the person is run over by a car and the car wheel passes directly over the leg.
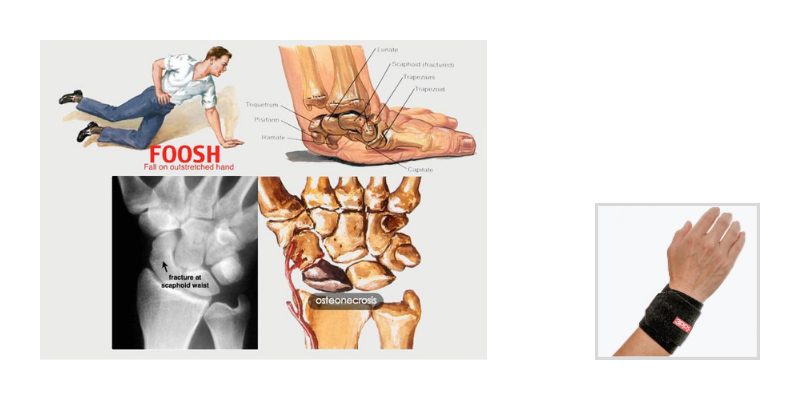
2) Indirectly violence or force- The bone breaks some distance away from the areas where the force or violence has been
applied. For example,
- of the humerus or
- of the clavicle may be caused by the patient falling on his outstretched hand.
3) Muscular violence (Violent contractions): forcible contraction of group of muscles may pull pieces of 3 bone away from the point where the muscle is attached. For example, sudden strong contraction of the quadriceps extensor group of muscles can pull sharply on the patella causing it to fracture.
4) Force of ligaments: Wrenching of a joint can cause its ligaments to pull so hard at the joint that causes fracture on one of the bones to which the ligaments are attached. For example, Force of lower leg bone at the ankle after stumbling.
B) Predisposing causes :
1) Extremes of age- It is found that in a very young or a very old person, very little violence is required to cause a bone to break.
2) Sex: stress fracture is mainly caused in athlet women or dancer,
3) Diseases of bone- If bones are not healthy then they are liable to break with a minimum amount of violence. For example, Osteomyelitis, Tuberculosis, Rickets, Cancer of the bone, Inflammation of the bone marrow etc.
4) Occupations:
- Nurse, police due to long standing.
- Soldiers, dancers, athlets due to long hike or marches.
Definitions
Pathological fracture is the fracture that occurs through a bone that is already weakened by a diseases.
Common causes of pathological fracture:
A) Local diseases of the bone:
1) Infections:
a) Chronic pyogenic osteomyelitis.
b) Tuberculosis
2) Benign tumors of the bone(more in children):
a) Chrondoma
b) Giant cell tumor
c) Haemangioma
3) Malignant tumors:
a) Osteosarcoma
b) Ewings tumors
c) Solitary myoma.
d) Metastatic carcinoma
B) General affection of the skeleton :
1) Congenital disorder: a) Osteogenis imperfecta.
2) Diffuse rarefaction of bone:
a) Cushing syndrome.
b) Rickets.
c) Nutritional osteomalacia
3) Disseminated tumors :
a) Multiple myeloma.
b) Metastatic carcinoma.
Common sites of pathological fracture:
1) Neck of humerous
2) Lower end of the radius.
3) Ribs.
4) Spine.tients
5) Pelvis.
6) Neck of femur.
[Ref-Adams.11th, 16page + BT. Basavanthappa, Orthopedics for nurses,38]

Avulsion fracture:
Forcible contraction of the group of muscle may pull pieces of bone away from the point where the muscle is attached known as avulsion fracture.
Sites of avulsion fracture:
1) Fracture of condule.
2) Fracture of epicondule.
3) Fracture of lesser trochanter.
4) Fracture of greater trochanter.
5) Fracture of patella.
Stress fracture/Fatigue fracture:
Any repetitive and chronic loading of bone leading to decrease the strength of the bone cause stress fracture.
Common sites for stress fracture:
1) Neck of 2nd metatarsal.
2) 3rd metatarsal.
3) Sesamoid of great toe.
4) Navicular bone in dancer & horse rider.
5) Tibia & fibula
Treatments of stress fracture.:
1) Complete bed rest.
2) Avoid causative activity at least 6-8 weeks.
3) Pain killers- if necessary.
4) Support to the affected part: Plaster, Back slab, Compression bandaging
Common fracture in children:
1) Supracondylar fracture.
2) Clavicle fracture.
3) Epiphyseal seperations.
4) Green stick fracture.
5) Buckle fracture,
6) Hair line fracture.
7) Crack or incomplete fracture.
Green stick fracture:
Green stick fracture involves a break in only part of the thickness of a bone.
[Ref-Lippincott, Adult orthopedic nursing, 1st edition,page-86]
i) It occurs during infancy and childhoods.
ii) Name is by analog with green wood which similarly breaks on the outside when bent.
Bone pain without fractures:
1) Metastatic bone disease or primary bone tumour.
2) Paget’s disease.
3) Osteomalacia.
4) Chronic infection (Osteomyelitis).
5) Osteonecrosis.
[Ref-Davidson’s “Principles & Practice of Medicine” 21″ edition page-1068]
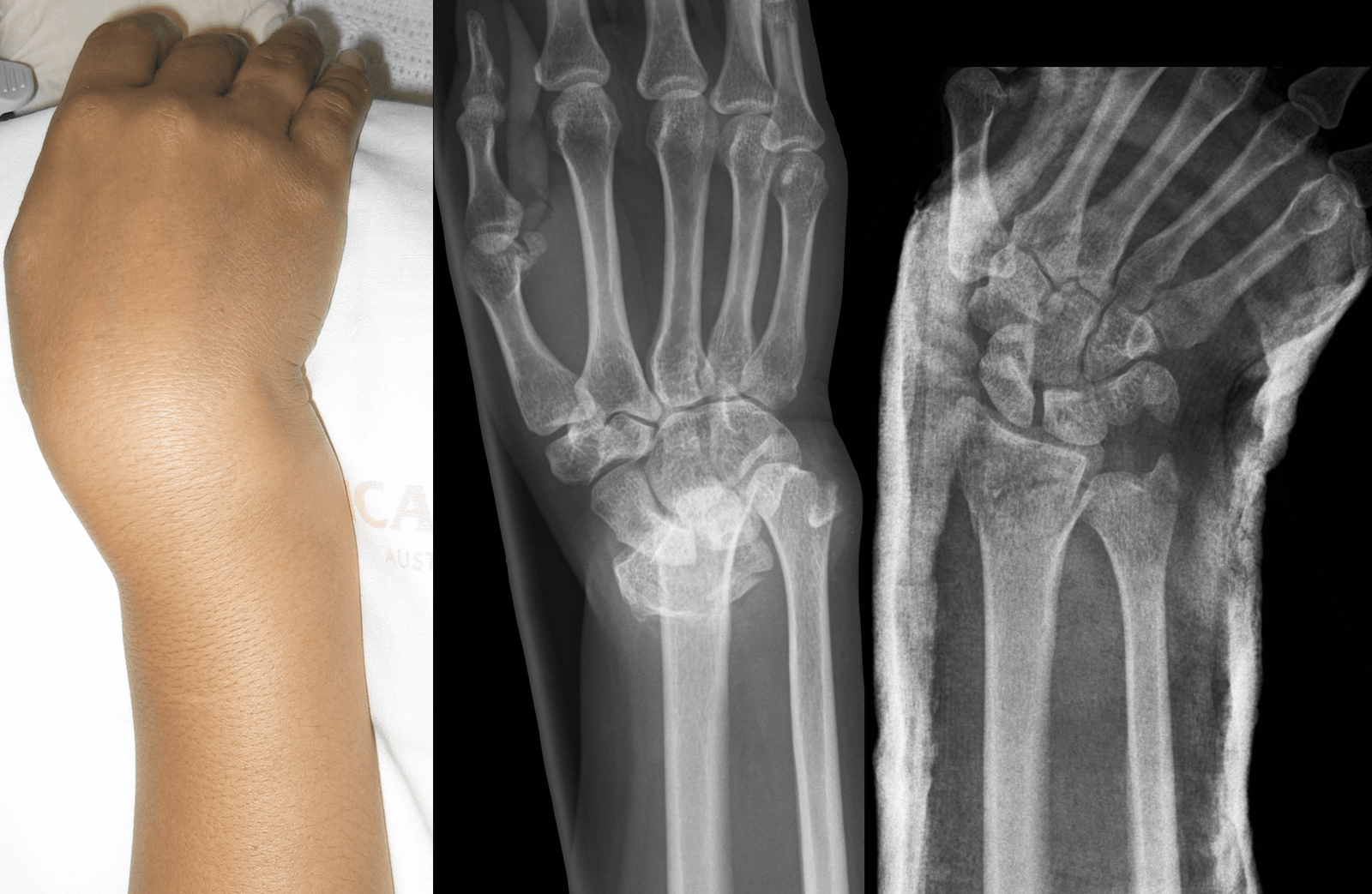
Signs & symptoms of fracture:
A) History of patients:
1. Patients give H/O direct or indirect trauma. E.g. fall, RTA, Physical assault.
2. In case of pathological or stress fracture there is no definitive history,
B) Symptoms:
1) Pain:
- Severe pain at the site of fracture.
- Pain increase on movement of injured part.
- Pain may absent immediately after shock or impaired nerve functions.
2) Swelling:
- Swelling may appear rapidly as a result of localizations of serous fluid.
- Swelling more in fracture than dislocations.
3) Deformity: Patient may unable to move affected part
- Loss of functions: Patient can not use the limbs as before.
C) Signs:
1 ) Inspection of the injured limb:
a) Compare with healthy side.
b) Position of the limb.
c) General condition of the patients.
d) Facial expression on pain scale.
e) Swelling-diffuse.
f) Anaemia of patients- due to blood loss (Open fracture)
g) Tongue-dry in case of blood loss fracture
h) Mental condition of the patients.
2) Palpation on the injured limb:
a) Local temperature-raised.
b) Tenderness-pain on touch of the injured limb.aoualan murt
c) Swelling- Size, shape, consistency, fluctuations.
d) Abnormal mobility- occurs in fracture but mobility only possible in the joint.
e) Bony crepitus – grating sound may be felt or heared due to movement at site of injury.
f) Echymosis bruising due to subcutaneous bleeding.
g) Palpate the vascular supply of the distal part:
- Palpate radial pulse in upper limb injury.
- Palpate posterior tibial artery in lower limb.
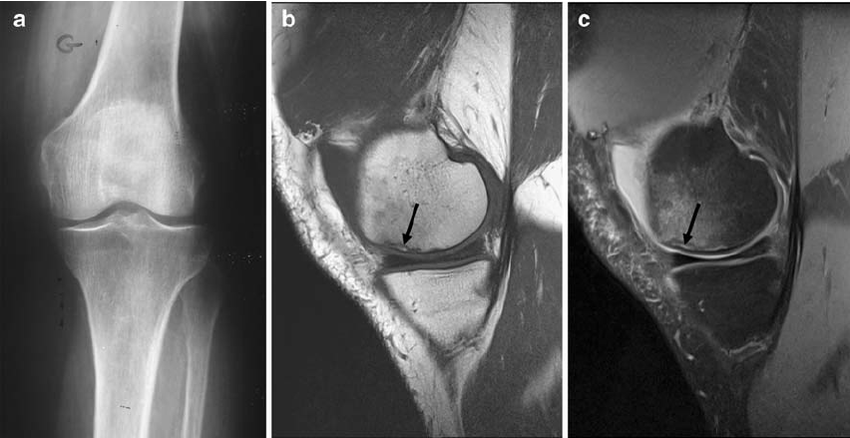
Confirmation the diagnosis of fracture:
A) Special investigations :
1) X-ray: Commonly used.
2) CT scan (Computed tomography): Clearly identify the exact positon number, size of fracture.
3) MRI (Magnetic resonance Imaging):can show image in any place with clear.
4) Arthrography: it is a technique in which X-ray contrast is directly injected into the joint to visualization of the joint structure.
5) Isotope Scanning
6) Ultrasound
B) General investigation:
1) Blood: TC,DC,ESR,C-RP (C-reactive protein).HB%, RBS, FBS etc.
2) ECG
3) Urine: BUN, Urine R/M/E, Albumin etc.
First aid management of fracture patients: A) At the scene of accidents:
1) Remove the victim from the accident spot.
2) Check vital signs quickly- pulse,BP,temperature, respirations.
3) Check the GCS level of the patients.
4) See that there is any bleeding point try to stop it immediately.
5) Seek the help of by standers.
6) Ensure that police and ambulance have been informed.
7) Consider the patients total condition. serious conditions such as shock. e.g. Do not focus only on the fracture site and look
B) Positioning of the patients:
1) Keep the patients in comfortable position while giving emergency care.
2) Elevate the injured extremity if possible.
C) Maintenance of airway:
1) Check the airway of patients for good breathing capability.
2) If there is any blood clots, vomits, dentures in mouth remove by clean cloths.
3) Extend the neck in Head tilt chin lift, jaw thurst to obtain pharynx and lungs in same line.
4) Check the breathing sounds and look at the chest for raises.
5) If no breathing give artificial respiration by mouth to mouth, or mouth to nose.
6) If the patients has facial injuries:
a) Keep patients in prone position.
b) Turn face in one side.
c) Apply pressure on the lower aspect of the chest.
D) Maintenance of circulation:
1) Check the radial, carotid pulse for detecting function of cardia.
2) If pulse is absent give CPR at the rate of 15:2.msg
3) Check for hypovolaemia due to blood loss.
E) Management of underlying features:
1) Control of external bleeding:
a) Elevation of injured site. Direct application of pressure bandage over the area.
b) Apply cold pack/ice pack over the bleeding point.
c) Never use torniquite.
2) Fracture & dislocations:
a) If you think fracture immobilize the injured part.
b) Move the patient carefully.
c) Never push the fracture fragement inside unknownly
d) Immobilize the injured part by using hard things.
3) Head injury:
F) Always avoid :
a) Look the injured area around the head.
b) Look for any vomiting which needs emergency care.
c) If any bleeding clean area and give bandage over the area.
1) Do not try to reduce fracture or dislocations.
2) Do not try to push back any portion of fracture fragements,
G) Transfer the patients to HOSPITAL as soon as possible for further management.
[Ref- BT. Basavanthappa, Orthopedics for nurses, Page-152]

Nursing assessment of a RTA patients:
1) Take H/O of-time, place, type(Bus, truck) accident from attendents.bgunean nog her wolt.p
2) Check consciousness level and neurological status by using GCS scale.
3) Check for vital signs.
4) Assess ABC (Airway Breathing, Circulations
5) Check any bleeding point in the body.
6) Take H/O DM, HTN, Visual problem, (If possible) atama tenero
7) Examination of vital structure:
a) If Head injury:
- Check for any bleeding from head.
- Take H/O any vomiting after accidents and how many.
- Examine the conditions of the pupils.
- Level of consciousness
- Assess neurological functions.
b) If chest injury:
- Any cuts or bleeding in the chest.
- Assess any impairment in the lungs due to accidents.
- Assess lungs sounds for detection of any impairment of the lungs cavity.
c) If limbs injured:
- Assess for any fracture and dislocations.
- Assess function of the limb.
- Assess for swellings,pain, tenderness in the injured limbs.
[Ref- BT. Basavanthappa, Orthopedics for nurses, Page-155]
Principles of management of fracture:
1) Immediate splinting and first aid
2) Safe transport.
3) Assessment of shock, associated injuries, vessel and nerve involvement, type of fracture.
4) Resuscitation with blood transfusion, antibiotics, IV fluids, analgesics, splinting, wound debridement.
5) X-ray of the part to. see fractures. Often MRI is required in spine, hip injuries.
6) Proper documentation and case sheet maintenance.
7) Reduction of fracture either by closed or by open method.
8) Immobilization.
9) Physiotherapy.
10) Rehabilitation.
11) Check X-ray to confirm the proper union of fracture segments.
[Ref-Sriram Bhat M “SRB’s Surgery for Nurses” 1″ edition page-431]
Common methods of immobilizations of fracture: A fracture can be immobilized by using:
1) Sling.
2) Splint.
3) Brace.
4) Cast.
5) Traction.
6) External & internal fixation.
Management of fracture patient:
A) Conservative management:
1) Complete bed rest.
2) Restoration of the normal anatomy by:
a) Reduction-it done by traction.
b) Immobilization- by plaster, cast, back slab.
3) Relief of pain by: Give suitable analgesics and sedatives.
4) Management of injuries by:-
b. Proper toileting of the wound,
c. Removal of the dead tissue.
d. Windows of the injured area and regular dressing (if necessary).
e. TT & TIG injections to prevent the development of tetanus,gas gangrene.
5) Prevention of infections: Giving proper antibiotics.
6) Nutritional diet: High protein, calcium, vitamin D containing diet.
7) Physiotherapy: Advising the patients active or passive exercise to prevent contracture of joint.
B) Operative method: When conservative methods are failed to correct deformity, operative methods are chosen:
1) Closed fracture: Skeletal traction, K-wire, external fixation.
2) Open fracture: Managed by Internal and external fixation fracture.
Nursing management of a fracture patients:
A) Assessment:
1) Take H/O of-time, place, type (Bus, truck) accident from attendants.
2) Check consciousness level and neurological status by using GCS scale.
3) Check for vital signs.
4) Assess ABC (Airway, Breathing, Circulations).
5) Check any bleeding point in the body.
6) Take H/O DM, HTN, Visual problem, (If possible).
7) Examination of vital structure.
8) Assess the level of pain -severity.
9) Check any swellings, tenderness of the injured area.tas
10) Assess for physical mobility especially for injured limbs.
B) Nursing diagnosis:
1) Acute pain due to disruption of normal anatomy of the bone.
2) Impaired physical mobility related to trauma.
3) Risk of infection related to cutting the skin (open fracture.)
4) Fluid volume deficit due to blood loss.
5) Knowledge deficit about care and treatment methods.
C) Nursing interventions:
1) Alleviation of pain:
a. Assess the level of pain according to pain scale.
b. Avoid unnecessary movement of the fractured limb.
c. Encourage to use relaxation technique.
d. Give analgesics according to doctors order.
e. Immobilization of injured limb also reduce pain. e.
2) Improve physical mobility:
a) Keep the patients in comfortable positions in the bed.
b) Elevate injured limb to reduce pain and swellings.
c) Apply cast/Tractions to immobilize the fracture part.
d) Encourage the patients to perform active exercise on unaffected limb.
e) Fingers exercise in cast applied patients.
f) Avoid weight bearing activity on injured limb until doctor’s order
3) Prevention of infections:
a) Regular monitoring of injured site.
b) Give dressing if it is open wound.
c) If cut injury wash with antiseptic solutions.
d) Give antibiotics according to doctors order.
e) Maintenance of sterile technique during dressing.
f) Give TT & TIG injection to prevent tetanus, gas gangrene.
4) Maintaining fluid balance:
a) Assess sign and symptoms of dehydration.
b) Opening I/V channel and immediately give saline to correct fluid deficiency.
c) Give Blood transfusion if severe blood loss from trauma.
d) Monitor intake and output of this patient.
5) Improving knowledge regarding care:
a) Explain the benefit of traction/cast in relation to his problem.
b) Explain the correct body positioning of injured limbs.
c) Advice to avoid weight bearing activity.
d) Taught to patients how to perform finger exercise in upper extremity fracture.
e) Encourage to take medication timely and regularly.
f) Keep the area of application (cast/traction/fixator) clean and dry.
Complications of fracture:
A. Immediate complication:
a) Local complication.
1) Skin laceration
2) Bleeding.
3) Injury to muscles, tendons, vessels, soft tissue and viscera.
b) General or remote complication:
1) Shock.
2) Multiple organ system failure (MOSF).
B. Early:
a) Local complication:
1) Skin-Infection, necrosis and gangrene.
2) Vessels- Volkmann’s ischemia, Volkmann’s ischemia contracture, venous thrombosis.
3) (Joint-Infection (Septic arthritis).
4) Bone-Infection at fracture site.
5) Acute compartment syndrome.
6) Gas gangrene.
b) General or remote complication:
1) Tetanus.
2) Pulmonary embolism.
3) Pneumonia.
4) Fat embolism.
5) Crush syndrome.
6) Delirium tremens.
C. Late complication:
a) Local complication:
1) Bone-Malunion, non-union, delayed union and avascular necrosis,
2) Growth retardation- From epiphyseal plate injury.
3) Post-traumatic osteoporosis (Osteopenia)
4 ) Sudeck’s painful atrophy.
5) Re-fracture,
6) Chronic osteomyelitis.
7) Osteoarthritis.
8) Persistent joint stiffness.
9) Deformity.
10) Ankylosis.
11) Post-traumatic myositis ossificans.
12) Tardy nerve palsy.
b) General or remote complication:
1) Renal calculi.
2) Accident neurosis.
[Ref-Dr. Jahir’s “Surgery 1″ Paper” 4th Edition, Page-534,435]
Prevention of immediate complications of fracture:
1. Careful removal of the offending agent.
2. Immediate step to control bleeding.
3. Immediate intravenous fluid and blood transfusion to prevent shock and multi organ system failure.
Methods of treatment of fracture:
1. Rest.
2. Traction.
3. Plaster immobilization.
4. Simple gravity / collar & cuff sling,
5. Close reduction & external fixation.
6. Open reduction & internal fixation.
7. Excision.
8. Prosthesis.
Bone healing:
Bone healing is a physiological process where by dead or damaged bone cells are regenerate and restore its original state.
Components of bone healing:
Healing involves a number of orderly process. But all the process do not occur in every healing. Components are:
1) Inflammation in response to injury. With removal of damaged tissue.
2) Proliferation and migration of parenchymal and connective tissue cells.
3) Formation of granulation tissue, scar and fibrous tissue.
4) Wound contraction.
5) Acquisition of wound strength.
[Ref-Khalek, Practical pathology and microbiology.page-33]
Methods of fracture healing: There are 3 methods of fracture healing.
1) Indirect fracture healing: This is the common method of fracture healing where both external and internal callus are formed
2) Direct bone healing: This type of bone repair is seen when bone fragments are anatomically reduced and rigidly fixed. Here ideally no external callus forms and there is no interposing fibrous tissue and cartilaginous tissue in between the fracture site.
3) Distraction histogenesis: Here bone repair is induced by gradual distraction of osteotomies and fracture.
[Ref-John Ebnezar’s “Orthopedics for Nurses”, 4th edition page-90,911]
Stages of fracture healing:
1) Haematoma stage: Bleeding occurs into the fracture site immediately following the fracture. Inflammatory exudates also appears. A haematoma formed surrounding the area of injured bone. and filling the cleft of fracture. After 24 hours the main blood supply increases to the fractured bone ends. Also new capillaries are starting to grow into the blood clot. The clot become bound together by fibroblast. And a fibrin mesh protectively enclose the damaged area.
2) Cellular proliferation stage: It is also known as granulation tissue formation stage. Within a few days the blood clot is replaced by granulation tissue. 2 days after the injury, red blood cell and tissue debris are removed by phagocytosis. Neovascularization and fibrogenesis occur from the periosteum and endosteum.
3) Callus formation stage: 6-10 days after the injury granulation tissue formed into pro callus. Newly formed cartilage and bone matrix disperse through the soft tissue callus and increase in number until the provisional callus (pro-callus) is established. The provisional callus extend beyond the fracture line. For some distances, these serving as the temporary splint to the injury. The provisional callus reaches maximum size at about 14-21 days. In an uncomplicated fracture.
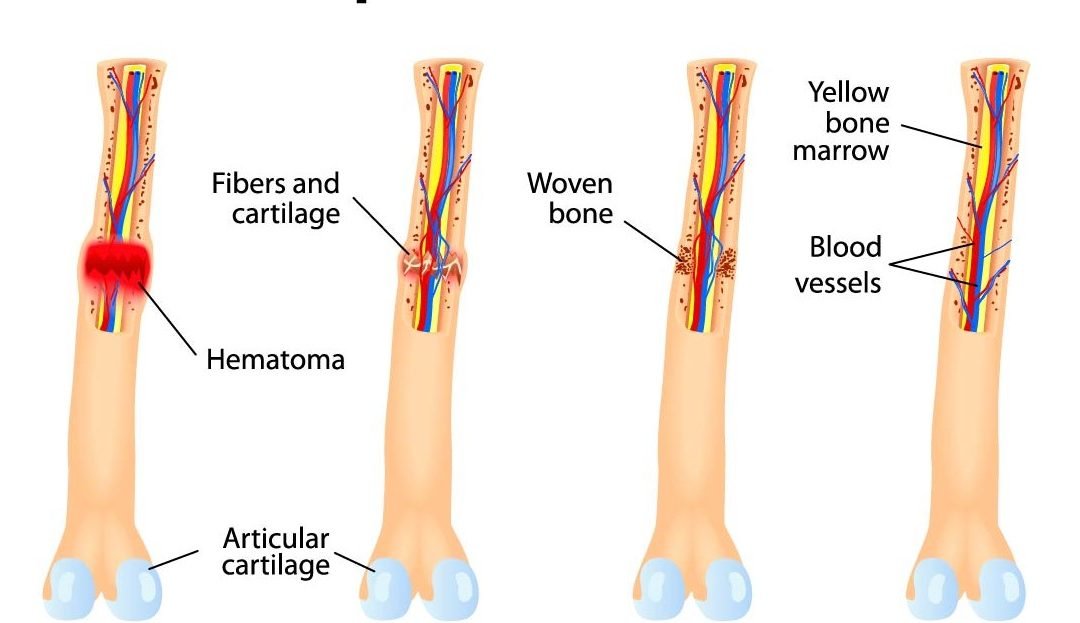
4) Callus ossification stage: With the deposition of calcium salts, a permanent callus of rigid bone is eventually formed.calcification first forms an:
- External callus between the periosteum and cortex. Next,
- Internal callus in the medullary plug. Finally,
- Intermediate callus between the cortical fragment.us
- During 3rd-10th week callus converted to bone.
5) Remodeling and consolidation stage: gradually provisional callus is increasingly strengthen by the formation of true bone as calcium salts are deposited The original structure of bone is formed by remodeling process and osteoclastic removal and osteoblastic lying down of bone. The intermediate bone is converted into compact bone, the external callus is removed & internal callus is hollowed out into a marrow cavity.
[Ref-Luckmann and Sorensen, Medical and Surgical nursing, 2nd edition, Page-1689]
Factors enhancing bone healing :
1. Age-healing is rapid in children.
2. Proper immobilization technique maintaining correct positioning,
3. Proper duration of immobilization (6-8 weeks).
4. Sufficient blood supply.
5. Maintaining proper nutrition improve bone healing passively.
6. Supplementation of calcium and vitamin D in diet.
7. Adequate hormones likes, growth hormones, parathormone, thyroxine supply in the bone.
8. Bioelectric fixation.
Factors inhibit bone healing :
A. Local cause:
1) Infection of bone.
2) Inadequate blood supply to one or both fragments.
3) Excessive shearing movement between the fragments.
4 ) Interposition of soft tissue between fragments.
5) Loss of apposition between the fragments.
6) Dissolution of fracture haematoma by synovial fluid.
7) Destruction of bone as by a tumor
8) Inadequate and improper immobilizations.
9) Intra-articular fracture.
B. General causes:
1) Use of immunosuppressive drugs-Steroids.
2) Immunosuppressive diseases- DM.
3) Age-in old age delayed fracture healing occur.
4) Nutritional deficiency: e.g. protein, vitamin C deficiency.
5) Generalized bone diseases: Osteoporosis, Osteomalacia, Osteogenesis imperfect.
Common sites of delayed union :
1. Fracture of neck of femur.
2. Fracture of shaft of femur.
3. Supracondylar fracture.
4. Colles fracture.
Adverse outcome of almost fracture:
1) Delayed union.
2) Non-union.
3) Malunion.
4) Pseudoarthosis.
5) Post traumatic arthritis.
6) Joint stiffness.
7) -Osteomyelitis.
8) Septic arthritis.
9) Nerve damage and nerve palsy.yam bag
10) Deformity.
11) Muscle damage including loss of strength.
Definition of Malunion: A malunion is when a fractured bone doesn’t heal properly. Some ways that it shows is by having the bone being twisted, shorter, or bent. Malunions can occur by having the bones improperly aligned when immobilized, having the cast taken off too early, or never seeking medical treatment after the break
Rules of bone healing :
1) Lower limb takes 2 times than upper limb to heal.
2) Fracture in elderly takes 2 times to heal than fracture in children or younger.
3) Transverse fracture takes longer time to heal than spiral or oblique fracture.
4) No fracture unites before 3 weeks.
| Limb | Children | Adult |
| Upper limb | 3 weeks | 6 weeks |
| Lower limb | 6weeks | 12 weeks |
E.g. Fracture of shaft of humerus 3 weeks in children and 6 weeks in adults.
[Ref-Dr.jahir, Surgery(p-1), 4th edition,page-546]