Abnormal hydramnios – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Abnormal hydramnios
Abnormal hydramnios means polyhydramnios and oligo hydramnios.. It is arbitarily defined as more than 2000 ml of liquor amni (polyhydramnios) or amniotic fluid being less than 300 ml (oligohydramnios) during the third trimester of pregnancy.
Polyhydromnios
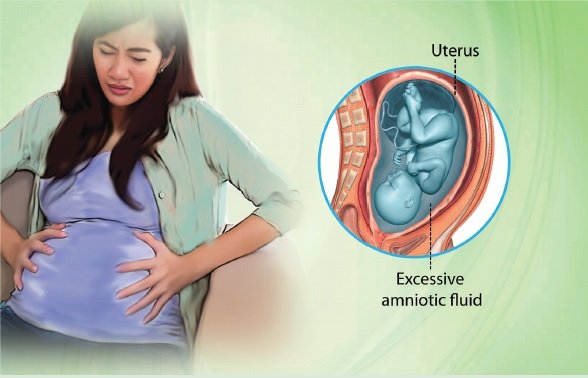
An excess of liquor amni termed as polyhydramnios or hydramnios. It is arbitarily defined as more than 2000 ml of liquor amni, because it becomes clinically obvious beyond this limit. Normal amniotic fluid volume is 500-1500ml.
Causes of polyhydramnios:
A. Fetal Causes:
➤ Fetal Abnormalities: Fetal anomalies such as hydrocephaly, anencephaly, esophageal atresia, fetal kidney problems, duodenal atresia, tracheoesophageal fistula, skeletal dysplasias, spina bifida and diaphragmatic hernia that can hamper the baby’s ability of swallowing and processing the amniotic fluid properly.
➤ Fetal Anemia: RBC (red blood cells) deficiency in the baby.
➤ Hydrops Fetalis (fluid accumulation or edema in two or more fetal compartments).
➤ Chromosomal Abnormalities: Inheriting abnormal chromosomes responsible for genetic disorders like Down’s syndrome and Edwards’ syndrome.
➤ Fetal macrosomia (having a baby too large for the gestational age).
B. Placental Causes:
➤ Twin-to-Twin Transfusion: An abnormal condition occurring when carrying identical twins, in which one twin receives excessive amounts of amniotic fluid while the other has little.
➤ Placental Blood Vessel Abnormality: Abnormal blood vessel growth on the placenta (chorioangioma).
C. Maternal Causes:
➤ Infectious Conditions: Toxoplasmosis, parvovirus, herpes simplex, rubella or cytomegalovirus infections affecting the mother may also reach the fetus, causing various abnormalities.
➤ Maternal Diabetes Mellitus (gestational or pre-existing): Abnormal blood sugar levels in the mother may lead the baby to produce excessive urine that increases the amniotic fluid volume.
➤ Maternal Rhesus Disease: Rhesus disease causes the mother’s antibodies to cross the placenta, often resulting in fetal anemia – one of the principal causes of Polyhydramnios.
➤ Blood incompatibilities between the mother and the baby.
➤ Hypertension
➤ Pre-eclampsia
Or (another answer)
Causes of polyhydramnios:
1. Fetal factors:
a) Fetal malformation.
➤ Neural tube defects: anencephaly, open spina bifida,
➤ Esophageal or duodenal atresia.
➤ Hydrops fetalis.
b) Chorioangioma of the placenta.
c) Multiple pregnancies.
2. Maternal diseases:
a) Diabetes mellitus.
b) Renal diseases, preeclampsia.
c) Cardiac diseases.

Types of polyhydramnios:
Clinical type
A) Chronic polyhydramnios – onset is insidious taking few weeks. Characterized by gradual accumulation of amniotic fluid.
B) Acute polyhydramnios- onset is sudden taking few days. Characterized by sudden and rapid accumulation of amniotic fluid.
Clinical features of polyhydramnios:
Symptoms:
1. Undue enlargement of the abdomen.
2. Feeling of tense abdomen.
3. Excessive movement of the fetus.
4. Respiratory distress, palpitation, flatulence, dyspepsia.
5. Edema, varicosities in legs.
Signs:
1. Patient is dysphonic in lying position.
2. Abdomen is hugely enlarged with tense shiny skin.
3. Features of preeclampsia may present.
4. Fundal height is more than the period of amenorrhoea.
5. Girth of the abdomen at the level of umbilicus is more than 100 cm before term.
6. Fluid thrill is present, ballottment of the fetus is easy.
7. Fetal part are not well defined.
8. FHS is not distinct.
9. Cervix is partially taken up or dilated.
Or (Another answer)
Mild cases of polyhydramnios may not cause any noticeable signs in the mother. However, severe cases can lead to the following symptoms:
➤ Difficulty breathing unless standing or sitting in an upright position.
➤ Difficulty climbing stairs.
➤ Decreased urine production.
➤ Larger belly size for one’s gestational age.
➤ Swelling of the abdominal wall, vulva and legs.
➤ Excessive weight gain.
Polyhydramnios may be suspected by the doctor in case it seems difficult to assess the body contours and heartbeat of the baby despite an enlarged size of the uterus. Excessive amounts of amniotic fluid in the uterus tend to worsen certain pregnancy symptoms, such as:
➤ Indigestion
➤ Constipation
➤ Abdominal pain
➤ Heartburn
➤ Stretch marks
➤ Varicose veins (when the valves within the veins stop working, causing the venous walls to become weak, leading to blood accumulation in the weak spots).

Diagnosis/tests of polyhydramnios:
a) Fetal Ultrasound: A fetal ultrasound is also useful for making the differential diagnosis by ruling out certain complications and birth defects.
b) Amniocentesis: This diagnostic procedure involves collecting an amniotic fluid sample (containing fetal cells and fetus produced chemicals) and testing it in a laboratory for evidences of any infections or other abnormalities.
c) Glucose Challenge Test: This test is performed to find out if the mother is suffering from gestational diabetes, which can confirm the diagnosis of Polyhydramnios.
d) Karyotype: It is a screening test, often used for checking the chromosomesof the baby for abnormalities.
e) Non-Stress Test.
f) Biophysical Profile (diagnostic procedure that combines the non-stress test with an ultrasound).
g) Doppler Ultrasound.
h) Fetal Echocardiogram.
i) Contraction Stress Test (assessing the baby’s heart rate with contraction of the uterus).
j) Blood Tests (for monitoring the mother’s diabetes levels).
Differential Diagnosis:
➤ Twin
➤ Maternal ascites
➤ Pregnancy with huge ovarian cyst
➤ Abruptio placenta
➤ Chorioangioma
Management of Polyhydramnios:
➤ Mild to moderate degrees usually does not require treatment.
➤ Hospitalization if symptoms are severe dyspnea, abdominal pain and difficult ambulation.
➤ Maintain bed rest with sedation to make the situation endurable.
➤ Monitor the patient for signs and symptoms of premature labor.
➤ Monitor maternal vital signs and fetal heart rate frequently; report changes immediately.
➤ Prepare the patient for amniocentesis and possible labor induction, as appropriate; keep in mind that amniocentesis for fluid removals is only temporary and may need to be done repeatedly.
Pregnancy less than 37 weeks
➤ Amniocentesis: slow decompression is done at the rate of about 500 ml per hour.
➤ Amount should be sufficient enough to relieve the mechanical distress.
➤ Amniotic fluid tested for fetal lung maturity.
Pregnancy more than 37 weeks
➤ Induction of labor is done.
➤ Amniocentesis
➤ Termination of pregnancy with congenital fetal anomaly.
During labour
➤ Usual management
Amniocentesis
Amniocentesis is a procedure in which amniotic fluid is removed from the uterus for testing or treatment. Amniotic fluid is the fluid that surrounds and protects a baby during pregnancy. This fluid contains fetal cells and various proteins.
Why amniocentesisis done in case of polyhydramnios?
Answer:
Amniocentesis can be done for various reasons:
- Genetic testing. Genetic amniocentesis involves taking a sample of amniotic fluid and testing it for certain conditions, such as Down syndrome.
- Fetal lung testing. Fetal lung maturity testing involves taking a sample of amniotic fluid and testing it to determine whether a baby’s lungs are mature enough for birth.
- Diagnosis of fetal infection. Occasionally, amniocentesis is used to evaluate a baby for infection or other illness. The procedure can also be done to evaluate the severity of anemia in babies who have Rh sensitization an uncommon condition in which a mother’s immune system produces antibodies against a specific protein on the surface of the baby’s blood cells.
- Treatment. If you accumulate too much amniotic fluid during pregnancy (polyhydramnios), amniocentesis might be done to drain excess amniotic fluid from your uterus.
- Paternity testing. Amniocentesis can collect DNA from the fetus that can then be compared to DNA from the potential father.
What Are the Complications Associated with Amniocentesis?
Answer:
Complications associated with amniocentesis include the following:
- The risk of miscarriage.
- Some women get cramps after the procedure.
- Some women have a small amount of vaginal bleeding after the procedure.
- Rarely, amniocentesis may cause amniotic fluid to leak out of the body.
- Another rare complication is a uterine infection.
- If you have an infection such as hepatitis C or HIV, amniocentesis can cause the infection to transfer to your unborn baby.

Prevention of polyhydramnios:
➤ Complete bed rest, especially towards the later pregnancy stages.
➤ Avoiding eating large meals.
➤ Avoiding any jerky movements.
➤ Using pillows and cushions for supporting the belly in bed.
➤ Avoiding spicy foods and any other foods that tend to worsen the heartburn.
➤ Avoiding lying down immediately after eating.
➤ Taking regular antenatal classes for polyhydramnios management guidelines.
Complications of polyhydramnios:
➤ Postpartum Hemorrhage: Extreme bleeding after delivery due to decreased uterine and muscle tone.
➤ High blood pressure (pregnancy-induced).
➤ Urinary tract infections in pregnancy.
➤ Umbilical cord prolapse (umbilical cord dropping into the vagina in front of the baby).
➤ Placental Abruption.
➤ Premature rupture of the membranes.
Consequences of polyhydramnios:
➤ Preterm Labor or Premature Birth: Delivery before completing the 37th week of pregnancy.
➤Placental Abruption: An abnormal condition characterized by partial or complete peeling away of placenta from the uterus wall before the baby is born.
➤ Premature Rupture of Membranes (PROM): Breakage or tearing of the amniotic sac after the 37th week of pregnancy but prior to the onset of labor.
➤ Birth Defects (Down’s syndrome, cleft palate).
➤ Stillbirth: Death of the baby in the uterus after the 20th week of pregnancy.
➤ Fetal Malposition: The baby lying in an atypical head-down position, often calling for a e-section delivery.
➤ Excessive fetal growth.