Abnormal obstetrics – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Abnormal obstetrics
Definition of abnormal obstetrics:
Abnormal obstetrics mean a high risk in which the life or health of the mother or fetus jeopardized by a disorder coincidental with or unique to pregnancy.
Common abnormal obstetrics:
A. complications during pregnancy:-
➤ Bleeding disorder
➤ Bleeding in early pregnancy
➤ Abortion
➤ectopic pregnancy
➤ Gestational trophoblastic diseases
➤Bleeding in late pregnancy
➤ Placenta Previa
➤Blood incompatibility
➤ Cardiovascular disorder
➤ Gestational hypertension
➤ Thromboembolic diseases
➤ Heart diseases
➤ Anaemia
➤ Gastrointestinal disorder
➤ Hyperemesis gravidarum
➤ Endocrine disorder
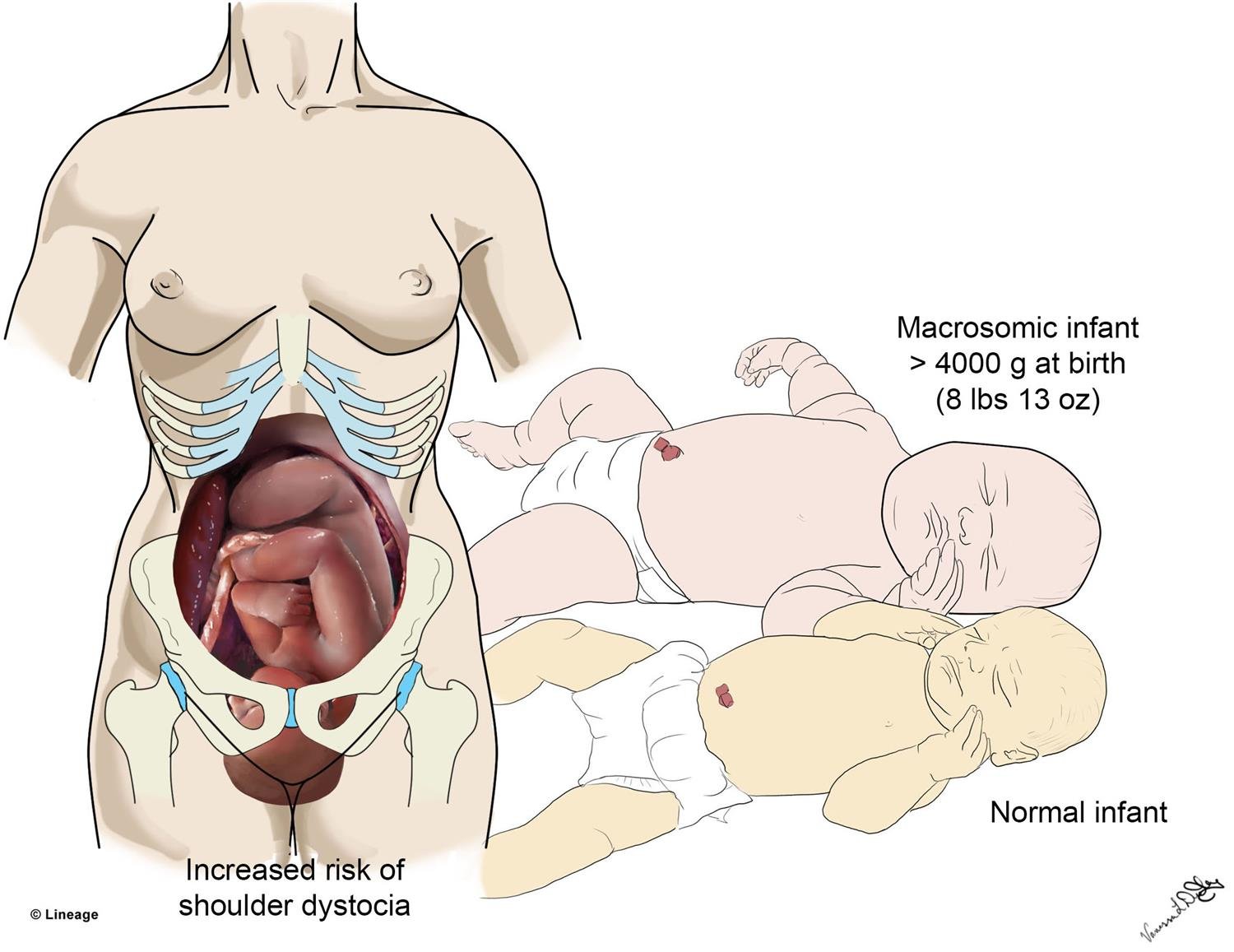
➤ Gestational Diabetes mellitus
➤ Urinary tract infection
➤ Abruptio placenta
➤ Disseminated intravascular coagulation
➤ Bacterial vaginosis
➤Substance abuse
➤ Pregnancy loss: grief and bereavement
B. Complications during intrapartum:
➤ Preterm labor
➤ Premature rupture of membrane
➤ Labor dystocia
➤ Induction of labor and augmentation
➤ Episiotomy
➤ Post term labor and birth
➤ Precipitate labor
➤ Uterine rupture
➤ Assisted vaginal delivery
➤ Forceps-assisted birth
➤ Vacuum extraction
➤ Polyhydramnios
➤ Oligohydramnios
➤ Prolapse umbilical cord
➤ Multifetal pregnancy
➤ Cesarean birth
C. Complications during postpartum:
➤ Puerperal pyrexia
➤ Sub involution of uterus
➤ Post-partum hemorrhage
➤ Genital tract infection
➤ Mental illness in the puerperium
D. Complications of the new born baby:
➤ Asphyxia neonatorum
➤ Respiratory problems
➤ Neonatal jaundice
➤ Convulsion in newborn
➤ birth trauma
➤ Infections of the newborn
➤ Metabolic problems
➤ Gastrointestinal problems
➤ Hematological problems
➤ Congenital malformation

Factors influencing complications in obstetrics: Several factors contribute to the experience of healthy and unhealthy outcomes. Clearly, not everyone exposed to the same event will have the same outcome (Stanhope and Lancaster, 2002). The following factors influencing complications in obstetrics:
1. Economic status: The poor are at greater risk of health problems. Economic risk is determined by the relationship between family financial resources and demand on these resources. Having adequate financial resources mean that a family is able to purchase the necessary commodities to health. These include: adequate housing, clothing, food, education, health/illness care.
2. Educational status: low education and lack of knowledge about pregnancy and pregnancy related childbirth education. In our country there is no proper facility on expectant parenting classes, antenatal and postnatal exercise, and easy childbirth exercise.
3. Women status: problems with the power, passenger, passages.
4. Social factors. early marriage and early pregnancy, illiteracy, poor socio-economic
condition, high crime neighborhood, communities without recreational or health
resources. Communities that have major chemical noise or other contaminants,
inadequate maternity services, underutilization of existing services.
5. Life style factors/ risk: personal health habits continue to contribute to the major cause to the maternal morbidity and mortality. Some don’t know their proper diet, personal hygiene, exercise and activity, sleep pattern and antenatal checkup.com
6. The age related factors: the optimum productive efficiency appears to be between 20 to 25.In the young adolescent pregnancy carries a higher risk due to preeclampsia, or above cephalopelvic disproportion and uterine inertia. In women aged over 35 years or the risk is 3-4 times higher.
7. Antenatal care: the most significant factor affecting maternal complication is the availability of antenatal care and its acceptance by the community. Unfortunately, those very groups, which have the highest mortality, like grand multipara or the patient of lower socio-economic status women who least often avail themselves of this facility.
8. Parity: the risk is slightly more in primi gravida but it is 3 times greater in Para 5 or above where postpartum hemorrhage, malpresentations and rupture uterus is more common. The risk is lowest in second pregnancy

Other risk factors include:
Factors affecting availability of care due to
➤ Lack of transport facilities
➤ Distance
➤ Roads
➤ Cost
➤ Quality of care
Factors of availability of care:
Availability of care depends on the following factors:
➤ Distance
➤ Lack of transport facilities
➤ Roads
➤ Cost
➤ Quality of care
Read More….