Acid fast bacilli – Basic microbiology, parasitology, and immunology; nature, reproduction, growth, and transmission of common microorganisms and parasites in Bangladesh; prevention including universal precaution and immunization, control, sterilization, and disinfection; and specimen collections and examination. Students will have an understanding of common organisms and parasites caused human diseases and acquire knowledge about the prevention and control of those organisms.
Acid fast bacilli
Acid-Fast Bacteria:
➤ Mycobacteria:
- Mycobacterium tuberculosis
- Mycobacterium leprae
- Mycobacterium bovis
- Atypical mycobacteria (e g., Mycobacterium avium-intracellulare complex)
➤ Nocardia asteroids: Causes ‘nocardiasis’
Medical Classification of Mycobacteria:
Mycobacteria can be classified into 3 major groups for the purpose of diagnosis and treatment, zum They are namely-
➤ Mycobacterium tuberculosis complex: (Cause tuberculosis)
- Mycobacterium tuberculosis
- Mycobacterium bovis
- Mycobacterium africanum
- Mycobacterium microti
➤ Mycobacterium leprae: (Causes leprosy)
➤ Non-tuberculous / atypical mycobacteria: (Can cause pulmonary disease) resembling tuberculosis, lymphadenitis, skin disease or disseminated disease.
- Group-1. Photochromogens: M. kansasii, M. marinum
- Group-II. Scotochromogens: M. scrofulaceum
- Group-III. Nonchromogens: M. avium-intracellulare complex
- Group-IV. Rapid grower: M. fortuitum-chelonei complex.
Mycobacterium Tuberculosis (Tubercle Bacilli)
Definition of Pulmonary Tuberculosis
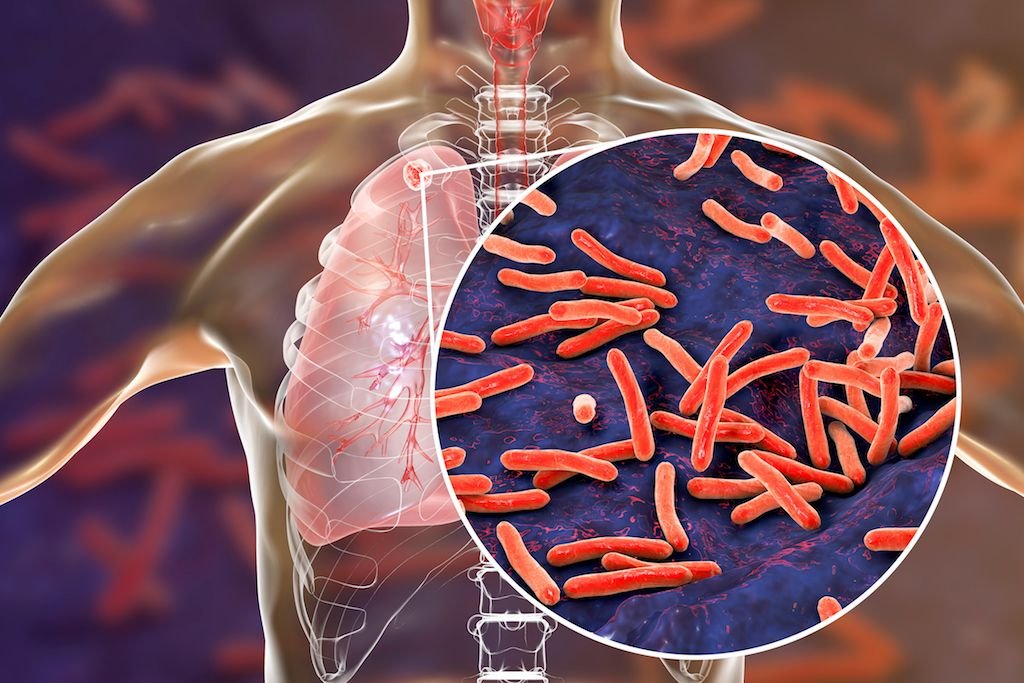
Tuberculosis is a specific infectious disease caused by M. Tuberculosis. The disease primarily affects lungs and causes pulmonary tuberculosis.
Or
Tuberculosis is a chronic infectious and communicable granulomatous disease caused by mycobacterium tuberculosis and rarely M. bovis which primarily affects lungs and causes pulmonary tuberculosis.
Organisms that responsible for TB
- Mycobacterium tuberculosis
- Mycobacterium bovis
- Mycobacterium africanum
Causes of Tuberculosis
Causes of acquiring tuberculosis include the following
Organisms that responsible for TB
a) Mycobacterium tuberculosis
b) Mycobacterium bovis
c) Mycobacterium africanum
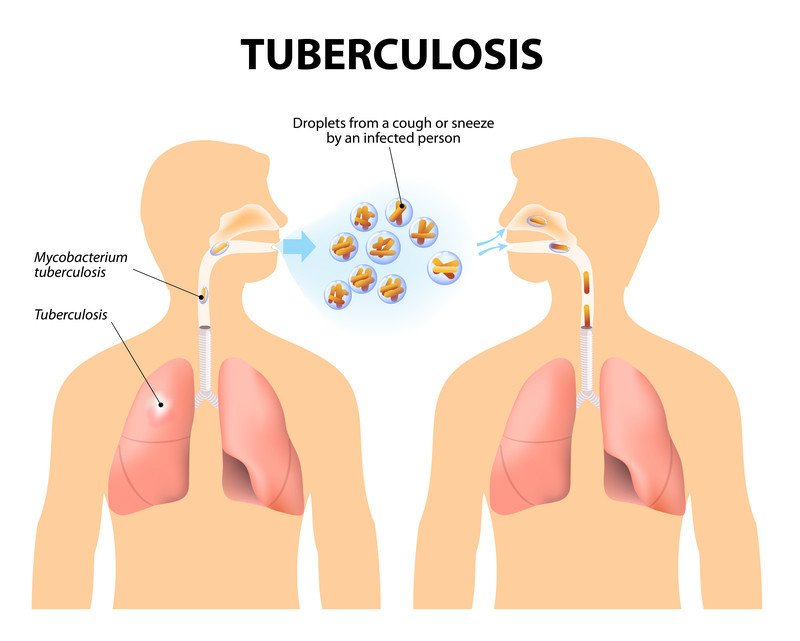
A. Close contact. Having close contact with someone who has an active TB.
B. Low immunity. Immuno-compromised status like those with HIV, cancer, or transplanted organs increases the risk of acquiring tuberculosis.
C. Substance abuse. People who are IV/injection drug users and alcoholics have a greater
chance of acquiring tuberculosis.
D. Inadequate health care. Any person without adequate health care like the homeless, impoverished, and the minorities often develop active TB.
E. Immigration. Immigration from countries with a high prevalence of TB could affect the patient.
F. Overcrowding. Living in an overcrowded, substandard housing increases the spreading of the infection.
Common Sites of Body are Affected
TB may affect any organ or tissue these are-
1. Pulmonary TB-Lung parenchyma
2. Extra pulmonary TB
- Kidney
- Pericardium
- Intestine
- Mediastinal lymphnodes
- Larynx
- Cervical lymphnodes
- Pleura
- Meninges
- CNS
- Spines
- Bones & joints
- Peritoneum
- Skin
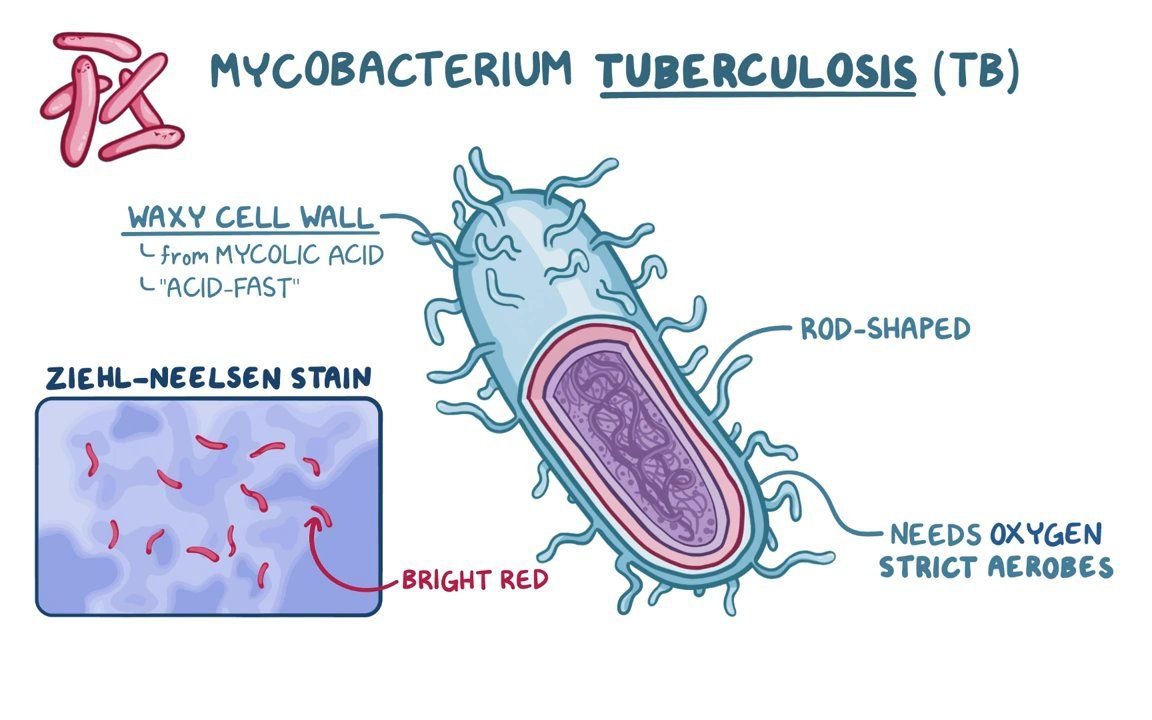
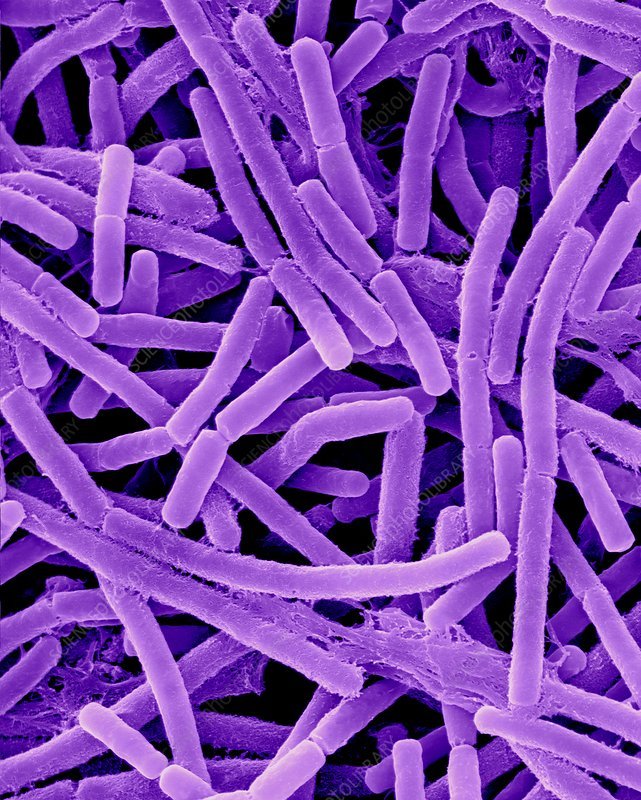
Morphology of Mycobacterium Tuberculosis:
- Aerobic, acid-fast bacilli (rods).
- They are neither Gram-positive nor Gram-negative
- Growth is slow. (Doubling time: 18 hours. So, cultures of clinical specimen must be h for 6-8 weeks)
- Non-spore forming and non-motile.
- Non-capsulated.
- Delicate straight or curved rods with rounded ends.
- Arranged either singly or in small groups.
Factors Increasing the Risk of Tuberculosis
Patient related
- Age (Children >young adult<elder)
- First generation immigrants from high Prevalence countries
- Close contacts of patients with smear positive pulmonary
- Overcrowding (Prisons, collective dormitories): Homelessness (doss houses and hostels)
- Chest radiographic evidence of self-healed tuberculosis
- Primary infection < 1 year previously
- Smoking: cigarettes, and bidis
Associate disease:
- Type 1 diabetes mellitus (DM)
- Malignancy (especially, leukemia, Lymphoma)
- Immune-suppression: HIV, high dose corticosteroids, cytotoxic agents.
- Chronic renal failure
- Silicosis
- Gastrointestinal disease associated with malnutrition (Gastrectomy, jejuno-ileal)
- Deficiency of vitamin A or D
- Recent measles: Increases risk of child contracting
Complications of Pulmonary Tuberculosis
A. Pulmonary
- Massive haemoptysis
- Corpulmonale
- Fibrosis/emphysema
- Atypical mycobacterial infection
- Aspergilloma
- Lung/pleural calcification
- Obstructive airways disease
- Bronchiectasis
- Bronchopleural fistula
B. Non-pulmonary
- Empyema necessitans
- Laryngitis
- Enteritis
- Anorectal disease
- Amyloidosis
- Poncet’s polyarthritis
Pathogenesis of Tuberculosis
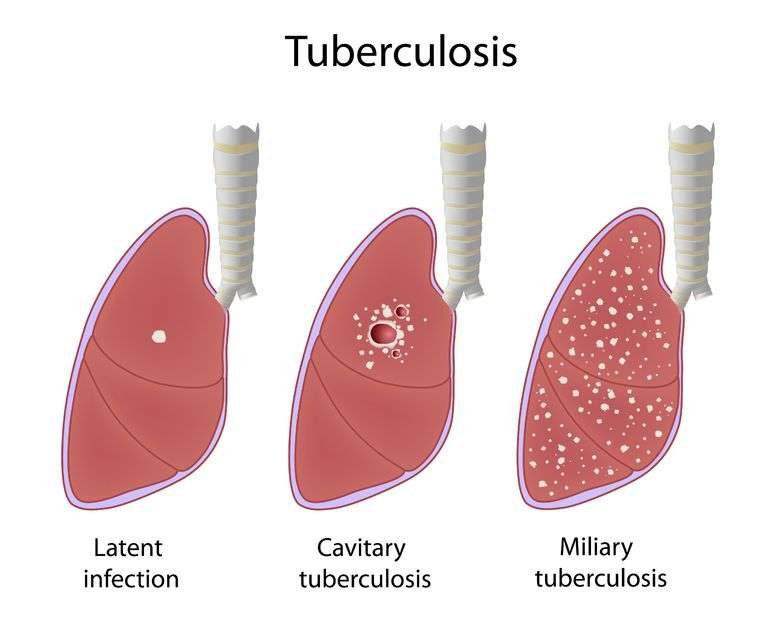
A. Primary infection:
Bacilli (Mycobacterium tuberculosis) enters by inhalation or ingestion of milk contaminated with M. bovis.
↓
Neutrophils come and try to engulf the bacilli and many of them are killed
↓
After 24 hours macrophage comes
↓
Try to destroy organism by phagocytosis
↓
Multiply within it
↓
Spread to regional lymphnode (hilar lymphnode)
↓
Lymphangitis Hilarlymphnode enlargement
↓
Primary Ghons complex Healed up and calcified
↓
Spread
↓
Ghons body
↓
Gives rise to military tuberculosis affecting various organs of body
B. Secondary or reinfection
Endogenous- Ghon’s complex (common) and exogenous (less common)
↓
Sensitized T cell secretes lymphokine
↓
Lymphokine actives macrophage
↓
Anoxia- phage secretes cytokines
↓
Vigorous pus formation
↓
Macrophage modified to epithelial cell
↓
Aggregation of epithelial cells from giant cell (Langhans) and fibrosis
↓
Formation of tubercle
Differences Between Human & Bovine Type of Mycobacteria:
| Traits | Human mycobacteria (M tuberculosis) | Bovine mycobacteria (M. bovis) |
| Source | Infected person. | Contaminated cow’s milk. |
| Route and portal of infection | Primarily by inhalation | Drinking of infected milk |
| Lesion | Pulmonary and extra- pulmonary TB. | Extra-pulmonary TB (eg. Intestinal TB) are prevalent. |
| Culture in Lowenstein- Jensen media | Eugenic. | Dysgenic. |
| O2 requirement | Strict aerobe | Micro-aerophilic. |
| Niacin test | Positive | Negative. |
| Action of glycerol | Glycerol enhances growth. | Glycerol inhibits growth. |
| Action of pyruvate | Growth is not enhanced | Enhanced. |
Differences between primary TB and secondary TB:
| Traits | Primary TB | Secondary TB (Re-infection) |
| Definition | Infection of an individual lacking previous contact with or immune- responsive to tubercle bacilli. | Usually lower part of upper lobe or upper part of lobe. Bilateral or multiple foci are very infrequent |
| Source of infection | Exogenous | Endogenous or exogenous |
| Affected site | Usually lower part of upper lobe or upper part of lobe. Bilateral or multiple foci are very infrequent | Apical or posterior segment of one or both upper lobes |
| Age incidence | Usually in children | Usually in adults |
| Characteristic lesion | Ghon’s focus and Ghon’s complex | Tubercle formation without involvement of regional lymph |
| Hilar lymph node | Enlarged caseous lymph node draining the Ghon’s focus, | Not involved |
| Fate | 95% cases heal by calcified scar or 92 Progressive spread. | Fibro-calcific scar or Progressive pulmonary TB. |
Diagnosis of Pulmonary Tuberculosis:
Principle: Diagnosis of pulmonary tuberculosis is based on-
- Demonstration of the acid-fast bacilli by Ziehl-Neelsen stained smear and other stained smear.
- Detection of antibody and antigen by immunological test.
- Detection of genes by NA based technique is used
Steps:
➤ Specimen collection:
- 3 sputum samples (now-a-days 2 samples are recommended).
- Bronchial aspirates.
- Blood
- Swab
➤ Microscopic examination:
- Ziehl-Neelsen staining: Finding- M. tuberculosis appears as straight or slight curved rods.
- Dark ground illumination (DGI): Finding- Yellow-orange bacilli.
- Fluorescence microscopy: Auramine / Rhodamine stain (For rapid screening purpose)
➤ Isolation & identification from culture: Culture is done in
- Lowenstein-Jensen medium: Incubation at 37°C for 6-8 weeks aerobically (most commonly done)
- Dubo’s solid medium
- Middle brook medium
➤ Immunological tests:
- Tuberculin test (Mantoux test).
- ICT, ELISA for Ab for cell mediated immunity.
➤ Nucleic acid based technique: Polymerase chain reaction (PCR).
Management of Tuberculosis
1. Clinical Features
A. Symptoms
a) Systemic effects: – Anorexia, Weight loss, Lassitude, Sleep sweat, evening pyrexia.
b) Local effects: –
- Lungs: Persistent cough, Sputum, Haemoptysis,
- Pleura: Pleural pain, Pleural effusion, breathlessness
- Pericardium/heart: Pain, arrhythmias, constrictive pericarditis, cardiac failure.
- Intestine: Diarrhea, Mal-absorption, obstruction
- GIT: Renal failure, Hematuria, epididimis, salpingitis, erythema nodosum.
- Skin: Lupus valgaris, iritis, phlyctennular keratoconjunctivitis.
- Bones/joints: Osteomyelitis, arthritis
- Lymphatic’s: cold abcesses, lymph adenopathy, sinuses.
B. Signs:
a) Early signs: – Crepitation’s usually heard at one or other lung apex posteriorly.
b) Sign of consolidation, cavitation’s, fibrosis, pleural effusion, and spontaneous pneumothorax may be present.
2. Investigations
A. Specimen for Pulmonary TB.
a) 3 samples of sputum or 3early morning samples of sputum
- On the spot specimen
- Early morning specimen
- A second spot specimen
b) Gastric washing for children
B. Diagnostic test
a) Chest x-ray P/A view: Showing patchy opacity with or without cavitation, pneumothorax, fibrosis, pleural effusion & milliary shadow.
b) Blood for TC, DC, ESR & CRP:
- TC – normal
- DC-lymophocyte
- ESR – High.
- CRP-High
- HB% Reduced
c) Sputum for AFB staining and C/S.
- Stain: Ziehl Neelson or Auramine staining
- Culture media: Lowenstein Jensen / Middle brook / BACTEK liquid media
d) Tuberculin test (Mantoux test)
e) PCR
f) Biopsy – Tubercle (Hall mark) of pleura, lymphnode.
g) Others –
- If pl. effusion – pleural fluid study
- Closed case – Broncho alveolar lavage/ Bronchial brushing.
- Antimicrobial Ab test-ELISA
3. Treatment of pulmonary TB
A. Rest-not required unless patient is very ill.
B. Diet normal
C. Isolation not required only very young children should be kept away from the patient
D. Anti TB drugs are the mainstay of therapy
a) Six month regimen
Initial phase: 2 month (four drugs): Patient will come daily to take the drugs (DOTS)
| Children | Adults | ||
| 50 kg | >50 kg | ||
| Rifampicin | 10-20 mg/kg | 450 mg | 600mg |
| Isoniazid | 10 mg/kg | 225 mg | 300 mg |
| Pyrazinamide | 20-35 mg/kg | 1200 mg | 1600 mg |
| Ethambutol | 25 mg/kg | 825 mg | 1100 mg |
| Pyridoxine | 10 mg after meal | ||
Continuation phase 4 month: Patient will be given drugs for 30 days each visit. Thrice daily
| Children | Adults | ||
| 50 kg | >50 kg | ||
| Rifampicin | 10-20 mg/kg | 450 mg | 600mg |
| Isoniazid | 10 mg/kg | 225 mg | 300 mg |
| Pyridoxine | 10 mg after meal | ||
b) Nine month regimen
Initial phase 2month (3 drugs): Patient will come daily to take the drugs (DOTs)
| Children | Adults | ||
| <50 kg | >50 kg | ||
| Rifampicin | 10-20 mg/kg | 450 mg | 600 mg |
| Isoniazid | 10 mg/kg | 225 mg | 300 mg |
| Pyrazinamide or | 20-35 mg/kg | 1200 mg | 1600 mg |
Ethambutol or Streptomycin | 25 mg/kg | 825 mg | 1100 mg |
| 30 mg/kg | 750 mg | 1000 mg | |
Continuation phage 7 month: Patient comes each alternative day to take the drugs (DOTs)
| Children | Adults | ||
| <50 kg | >50 kg | ||
| Rifampicin | 10-20 mg/kg | 450 mg | 600 mg |
| Isoniazid | 10 mg/kg | 225 mg | 300 mg |
Advice
- Yellowish coloration of urine & sweating nothing to be worried about it and not to discontinue drug
- Chest pain, abdominal pain, jaundice may occurs in that cases consult with the doctors.
- Not to discontinue the drug without the permission of the doctor.
- If any problem with vision then consult with doctor
Adverse Effect of Anti-Tubercular Drugs
A. Isoniazid
a) Common adverse effect:
- Peripheral neuropathy
- Hepatitis
- Rash
b) Less common adverse effect:
- Lipoid reactions
- Seizures
- Psychosis
- B. Rifampicin
a) Common adverse effect:
- Febrile reaction
- Hepatitis
- Rash
- Gastrointestinal disturbance
b) Less common adverse effect:
- Interstitial nephritis
- Thrombocytopenia
- Haemolytic anaemia
C. Pyrazinamide
a) Common adverse effect:
- Hepatitis
- Gastrointestinal disturbance
- Hyperuricaemia
b) Less common adverse effect
- Rash
- Photosensitizations
- Gout
c) Streptomycin
d) Common adverse effect:
- 8th nerve damage
- Rash
e) Less common adverse effect:
- nephrotoxicity
- Agranulocytosisi
f) Ethambutol
g) Common adverse effect:
- Retro bulbar neuritis
- Arthralgia
h) Less common adverse effect:
- Peripheral neuropathy
- Rash
Nursing Management of Tuberculosis
Nursing management includes the following
A. Nursing Assessment
The nurse may assess the following:
- Complete history. Past and present medical history is assessed as well as both of
the parents’ histories. - Physical examination. A TB patient loses weight dramatically and may show the loss in physical appearance.
B. Nursing Diagnosis
- Based on the assessment data, the major nursing diagnoses for the patient include:
- Risk for infection related to inadequate primary defenses and lowered resistance.
- Ineffective airway clearance related to thick, viscous, or bloody secretions.
- Risk for impaired gas exchange related to decrease in effective lung surface.
- Activity intolerance related to imbalance between oxygen supply and demand.
- Imbalanced nutrition: less than body requirements related to inability to ingest adequate nutrients.
C. Nursing Care Planning & Goals
The major goals for the patient include:
- Promote airway clearance.
- Adhere to treatment regimen.
- Promote activity and adequate nutrition.
- Prevent spread of tuberculosis infection.
D. Nursing Interventions
Nursing interventions for the patient include:
- Promoting airway clearance. The nurse instructs the patient about correct positioning to facilitate drainage and to increase fluid intake to promote systemic hydration.
- Adherence to the treatment regimen. The nurse should teach the patient that TB is a communicable disease and taking medications is the most effective means of preventing transmission.
- Promoting activity and adequate nutrition. The nurse plans a progressive activity.schedule that focuses on increasing activity tolerance and muscle strength and a nutritional plan that allows for small, frequent meals.
- Preventing spreading of tuberculosis infection. The nurse carefully instructs the patient about important hygienic measures including mouth care, covering the mouth and nose when coughing and sneezing, proper disposal of tissues, and hand washing
- Acid-fast bacillus isolation. Initiate AFB isolation immediately, including the use of a private room with negative pressure in relation to surrounding areas and a minimum of six air changes per hour.
- Disposal. Place a covered trash can nearby or tape a lined bag to the side of the bed to dispose of used tissues,
- Monitor adverse effects. Be alert for adverse effects of medications
E. Evaluation
Expected patient outcomes include:
- Promoted airway clearance.
- Adhered to treatment regimen.
- Promoted activity and adequate nutrition.
- Prevented spread of tuberculosis infection
F. Discharge and Home Care Guidelines
- Before the discharge, the nurse should instruct the patient to:
- Disposal of secretions. Cough and sneeze into tissues and to dispose of all secretions in a separate trash can.
- Isolation. Wear a mask when going outside of the room.
- Activity and nutrition. Remind the patient to take a lot of rest and to eat balanced meals to aid recovery.
- Adverse effects. Advise the patient to watch out for adverse effects of medications and to report them to the physician immediately.