Acute appendicitis – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Acute appendicitis
Definition of Acute Appendicitis:
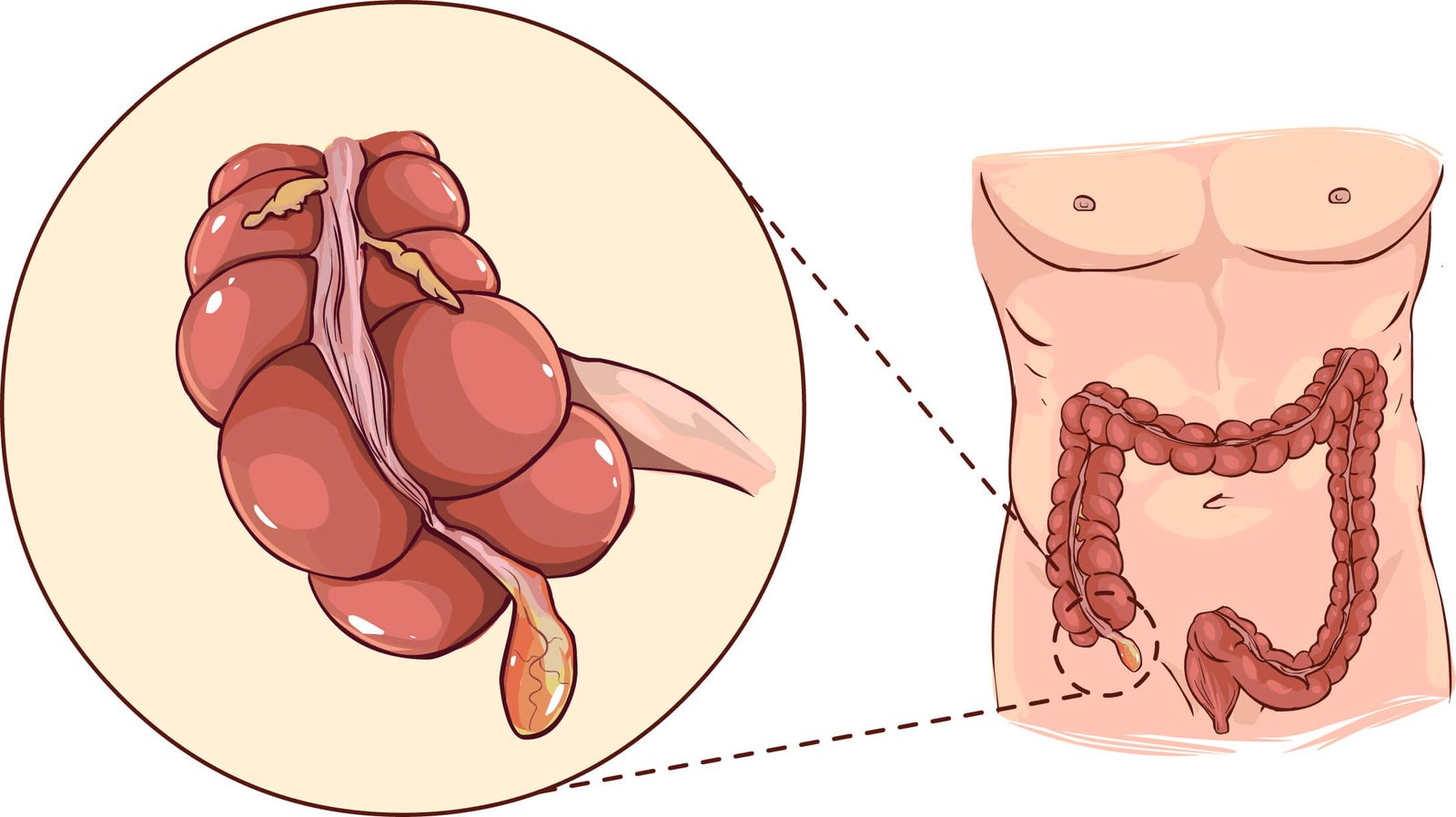
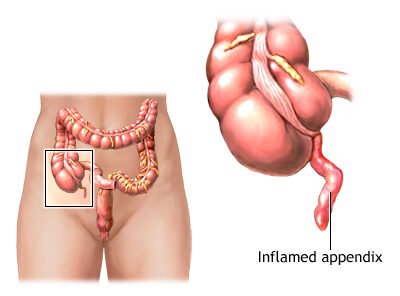
Acute appendicitis is an acute inflammation of the vermiform appendix, most likely due to obstruction of the lumen of the appendix (by fecalith, normal stool, infective agents, or lymphoid hyperplasia).
Or,
Appendicitis is inflammation of the appendix. Symptoms commonly include right lower abdominal pain, nausea, vomiting, and decreased appetite
Causes of Acute Appendicitis:
A. Obstructive of the lumen of appendix:
a. In the lumen:
- Facecloth
- Pin worm
- Round worm
- Seeds
- Undigested food particle
b. In the wall:
- Hyperplasia of the sub-mucosal lymphoid follicles
- Extension of carcinoma in caecum
- Carcinoid tumour
c. Outside the wall:
- Kinking of the appendix
- Compression by bands, adhesion
B. Other causes:
a. Decreased dietary fiber
b. Increase consumption of refined carbohydrate (fast foods)
c. Increase consumption of aerobic and anaerobic organism
- E. coli (85%)
- Enterococci (30%)
- Proteus
- Cl. welchii
- Anaerobic streptococci
Types of Appendicitis:
1. Acute appendicitis (commonest)
- Acute obstructive (commonest 80%)
- Acute non obstructive (acute catarrhal)
2. Recurrent appendicitis (more than one attack)
Management of Acute Appendicitis;
Clinical feature:
A. Symptoms:
- Dull pain near the navel or the upper abdomen
- Loss of appetite
- Nausea and/or vomiting soon after abdominal pain begins
- Abdominal swelling
- Fever of 99-102 degrees Fahrenheit
- Inability to pass gas
- Other symptoms:
✔ Dull or sharp pain anywhere in the upper or lower abdomen, back, or rectum
✔ Painful urination
✔ Vomiting that precedes the abdominal pain
✔ Severe cramps
✔ Constipation or diarrhea with gas
B. Sign of acute appendicitis:
- Pyrexia
- Localized tenderness in the right iliac fossa
- Muscle guarding
- Rebound tenderness
- Other sign:
✔ Pointing sign (positive)
✔ Rovsigns sign (positive)
✔ Psoas sign (positive in retrocaecal appendix)
✔ Obturator sign (positive in pelvic appendix)
Investigation:
A. Routine examination:
- Blood for TC, DC, ESR, Hb%
- Urine for RME
B. Selected cases:
- Pregnancy test
- Urea and electrolyte
- Plain X-ray KUB region to exclude ureteric stone
- USG of pelvic region
- Abdominal USG: Mainly for children
- X-ray abdomen to exclude ureteric stone and intestinal obstruction
Treatment:
- Emergency appendectomy (as early as possible)
- Preoperative antibiotic
- If peritonitis suspected, antibiotic in IV route
- If children with pyrexia – antibiotic, IV fluid and salicylates
Complication of Acute Appendicitis:
- Appendicular lump formation
- Local abscess
- Gangrene
- Perforation
- Peritonitis-Generalized or localized
- Septicemia
- Portal pyemia
- Liver abscess
- Pelvic abscess, subphrenic abscess
- Recurrent appendicitis
Fates of Acute Appendicitis:
A. Resolution: Spontaneously or by drug.
B. Complication of acute appendicitis.
- Appendicular lump formation (made of the appendix, caecum, greater omentum and coils of intestine)
- Local abscess (Appendicular abscess)
- Gangrene
- Perforation
- Peritonitis-Generalized or localized
- Septicemia
- Portal pyemia
- Liver abscess
- Pelvic abscess, subphrenic abscess
Risk factors of perforation of appendix:
- Extremes of age
- Immunosuppressant
- Diabetes mellitus (DM)
- Fecolith obstruction
- Pelvic appendix
- Previous abdominal surgery
Differential Diagnosis of Acute Appendicitis:
A. Children:
- Gastroenteritis
- Mesenteric adenitis
- Meckels adenitis
- Intussusceptions
- Henoch-scholein purpura
- Lobar pneumonia
B. Adult:
- Regional enteritis
- Right ureteric colic
- Perforation peptic ulcer
- Torsion testis
- Pancreatitis
- Rectus sheath haematoma
C. Adults female:
- Mittelschmerz
- Pelvic inflammatory disease
- Pylonephritis
- Ectopic pregnancy
- Torsion rupture of ovarian cyst
- Endometriosis
D. Elderly:
- Diverticulitis
- Intestinal obstruction
- Colonic carcinoma
- Torsion appendix epiploicae
- Mesenteric infarction
- Leaking aortic aneurysm
Management of Burst Appendix:
1. History: Extreme age, immunosuppressant, DM, pelvic appendix, previous abdominal surgery.
2. Clinical features:
- Severe pain in the right iliac fossa
- S/S of peritonitis-Sharp pain, vomiting, raised temperature, rigid abdomen, localized or generalized tenderness, rebound tenderness, Hippocratic facies.
3. Investigation: CBC, USG (whole abdomen), Plain X-ray (in rectal posture)
4. Treatment:
- NPO (Nothing per os)
- NG suction
- IV fluid, electrolyte, total perenteral nutrition
- IV antibiotics-Cefuroxime
- IV ranitidine
- Immediate laparotomy and emergency appendectomy followed by through peritoneal toileting
Pathophysiology of Appendicitis:
The simple pathophysiology of appendicitis follows the typical pathophysiology of infection.
1. Obstruction: The appendix becomes inflamed and edematous as a result of becoming kinked or occluded by a fecalith, tumor, or foreign body.
2. Inflammation: The inflammatory process increases intraluminal pressure, initiating a progressively severe, generalized, or periumbilical pain.
3. Pain: The pain becomes localized to the right lower quadrant of the abdomen within a few hours.
4. Pus formation: Eventually, the inflamed appendix fills with pus.
Nursing Management of Appendicitis:
Nursing Assessment
Assessment of a patient with appendicitis may be both objective and subjective.
- Assess the level of pain.
- Assess relevant laboratory findings.
- Assess patient’s vital signs in preparation for surgery.
Nursing Diagnosis
Based on the assessment data, the most appropriate diagnoses for a patient with appendicitis are:.
- Acute pain related to obstructed appendix.
- Risk for deficient fluid volume related to preoperative vomiting, postoperative restrictions.
- Risk for infection related to ruptured appendix.
Planning & Goals
Goals for a patient with appendicitis include:
- Relieving pain.
- Preventing fluid volume deficit.
- Reducing anxiety.
- Eliminating infection due to the potential or actual disruption of the GI tract.
- Maintaining skin integrity.
- Attaining optimal nutrition.
Nursing Interventions
The nurse prepares the patient for surgery.
- IV infusion. An IV infusion is made to replace fluid loss and promote adequate renal functioning.
- Antibiotic therapy. Antibiotic therapy is given to prevent infection.
- Positioning. After the surgery, the nurse places the patient on a High-fowler’s position to reduce the tension on the incision and abdominal organs, thereby reducing pain.
- Oral fluids. When tolerated, oral fluids could be administered.
Evaluation
- Relieved pain.
- Prevented fluid volume deficit.
- Reduced anxiety.
- Eliminated infection due to the potential or actual disruption of the GI tract.
- Maintained skin integrity.
- Attained optimal nutrition.
Discharge and Home Care Guidelines
Discharge teaching for patient and family is imperative.
- Removal of sutures. The nurse instructs the patient to make an appointment with the surgeon to remove the sutures between the 5th and 7 days after surgery.
- Activities. Heavy lifting is to be avoided postoperatively; however, normal activity can be resumed within 2 to 4 weeks.
- Home care. A home care nurse may be needed to assist with incision care and to monitor the patient for complications and wound healing.
Documentation Guidelines
The focus of documentation in patients with appendicitis should include:
- Client’s description of response to pain.
- Acceptable level of pain.
- Prior medication use.
- Results of laboratory tests.
- Surgical site,
- Signs and symptoms of infectious process.
- Recent or current antibiotic therapy.
- Plan of care.
- Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcomes.
- Modifications to plan of care.
- Long term needs.
Complication After Appendectomy:
A. Early:
Wound infection
Intra abdominal abscess
A period of a dynamic ileus
Respiratory complication
Venous thrombosis and embolism,
Portal pyaemia (pylophlebitis)
Faecal fistula
B. Late:
- Intestinal obstruction from adhesions
- Incisional hernia
- Right inguinal hernia following the grid iron incision
- Sterility in women from frozen pelvis
Preoperative and Postoperative Management for Appendicitis
Preoperative Management
1. Keep patients on NPO (withhold from oral foods and fluids).
2. Establish IV access and administer parenteral analgesic.
3. Administer parenteral prophylactic antibiotic.
- Start at least 60 minutes prior to appendectomy
- Significantly reduces wound infection
- Use antibiotics with broad coverage of gram-negative and anaerobic bacteria
Postoperative Management
1. Administer analgesic and antiemetic if needed for pain and vomiting.
2. Encourage early ambulation.
3. Administer postoperative antibiotics.
- Not recommended as a routine use
- Only recommended for complicated perforated appendicitis: postoperative intravenous antibiotics for 3 to 5 days. Antibiotic treatment will be stopped when core temperature is <38°C for 24 hours, patient tolerates two meals consecutively, mobilize independently, and WBC (white blood cell) count normalizes.