B2-Adrenoceptor Agonists – This book covers the entire syllabus of “Pharmacology” prescribed by BNMC- for diploma in nursing science & midwifery students. We tried to accommodate the latest information and topics. This book is an examination setup according to the teachers’ lectures and examination questions.
At the end of the book, previous questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourish. The unique way of presentation may make your reading of the book a pleasurable experience.
B2-Adrenoceptor Agonists
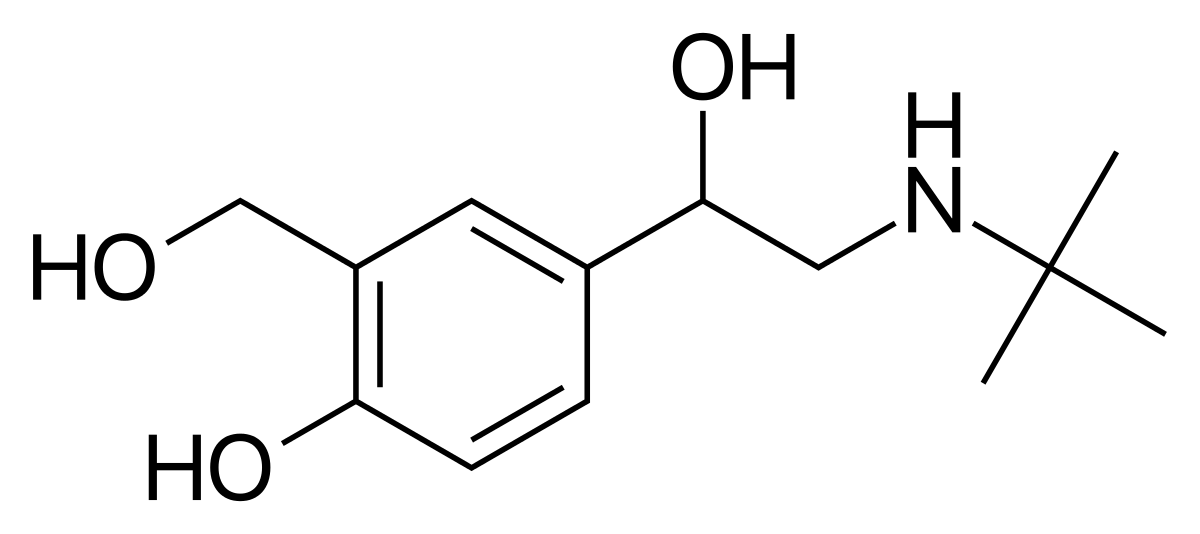
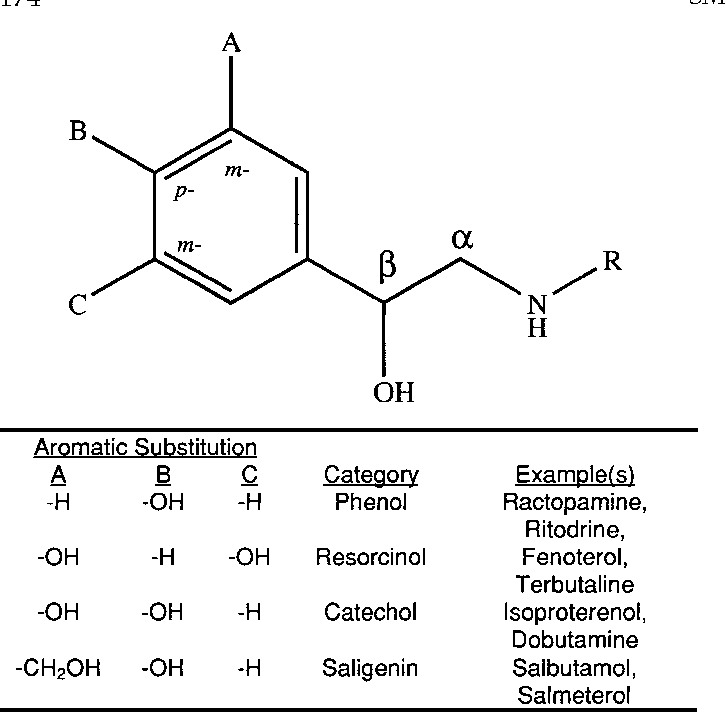
Examples of ẞ2-adrenoceptor agonists include salbutamol (short acting) and salmeterol (long acting).
Mechanism of action
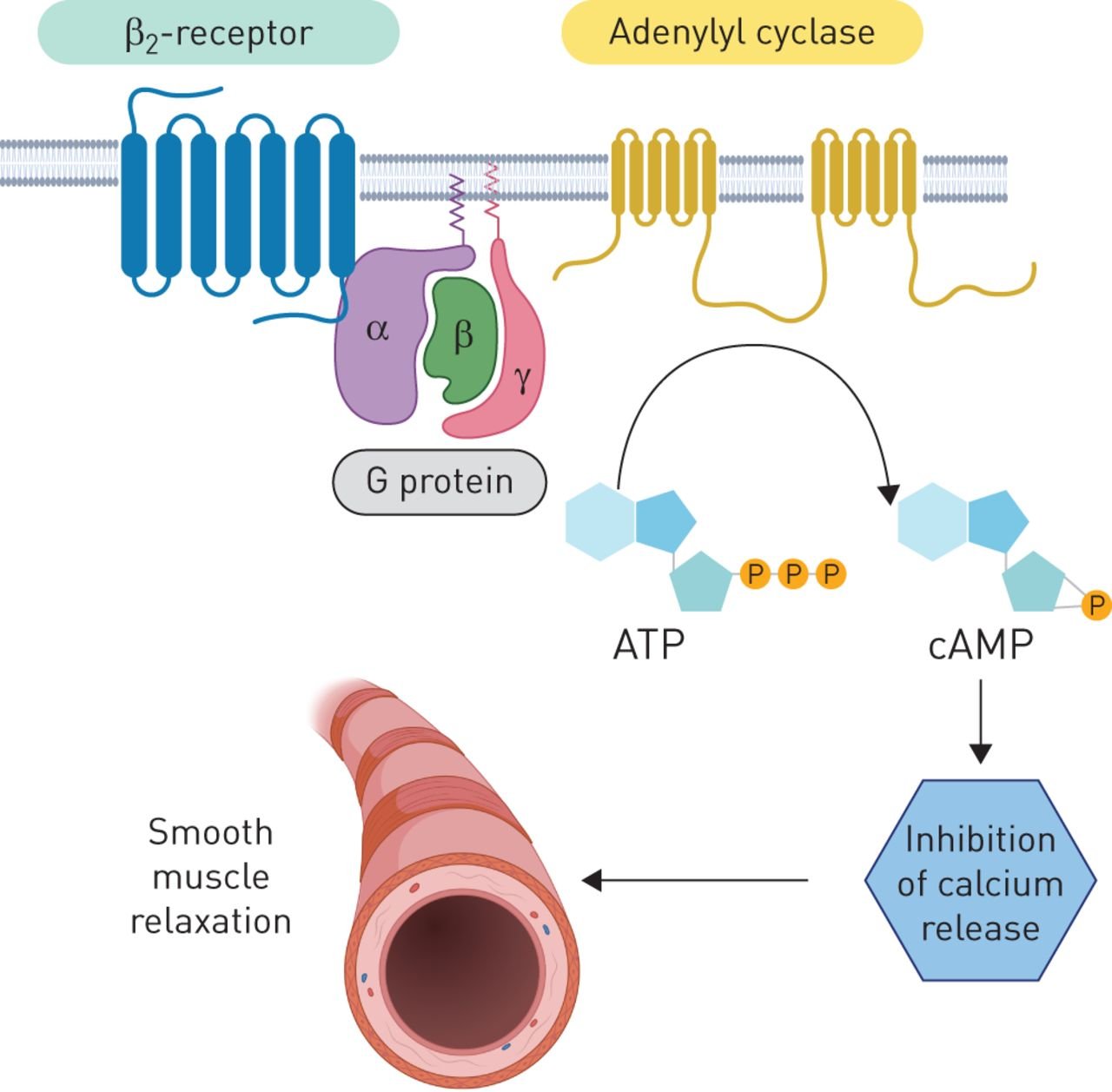
Airway smooth muscle does not have a sympathetic nervous supply, but it does containẞ2- adrenoceptors that respond to circulating adrenaline. The stimulation of ẞ2-adrenoceptors leads to a rise in intracellular cAMP levels and subsequent smooth muscle relaxation and bronchodilation.
- B2-Adrenoceptor agonists may also help prevent the activation of mast cells, as a minor effect.
- Modern selective ẞ2-adrenoceptor agonists are potent bronchodilators and have very few B1-stimulating properties (i.e. they do not affect the heart).
Route of administration
1. Inhaled.
2. Oral administration is reserved for children and people unable to use inhalers; intravenous administration for status asthmaticus.
Indications
B2-Adrenoceptor agonists are used to relieve bronchospasm. They may be used alone in mild, occasional asthma, but are more commonly used in conjunction with other drugs, e.g. corticosteroids.
Contraindications
Caution in hyperthyroidism, cardiovascular disease, arrhythmias.
Adverse effects
Fine tremor, tachycardia, hypokalaemia after high doses.
Therapeutic notes
B2-Adrenoceptor agonists treat the symptoms of asthma but not the underlying disease process. Salmeterol is a long-acting drug that can be administered twice daily. It is not suitable for relief of an acute attack.
Anticholinergics
Ipratropium bromide: (short acting) and tiotropium (long acting) are examples of anticholinergic (antimuscarinic) drugs.
Mechanism of action
Parasympathetic vagal fibres provide a bronchoconstrictor tone to the smooth muscle of the walls. airways. They are activated by reflex on stimulation of sensory (irritant) receptors in the airway Muscarinic antagonists act by blocking muscarinic receptors, especially the M3 subtype, which responds to this parasympathetic bronchoconstrictor tone.
Route of administration: Inhaled.
Indications: Anticholinergics are used as adjuncts to ẞ2-adrenoceptor agonists in the treatment of asthma.
Contraindications: Glaucoma, prostatic hypertrophy, pregnancy.
Adverse effects: Dry mouth may occur. Systemic anticholinergic effects are rare.
Therapeutic ‘notes: Anticholinergics have a synergistic effect when administered with 32- adrenoreceptor agonists in asthma.
Xanthines
Theophylline is an example of a xanthine.
Mechanism of action
The xanthines appear to increase cAMP levels in the bronchial smooth muscle cells by inhibiting phosphodiesterase, an enzyme which catalyses the hydrolysis of cAMP to AMP. Increased CAMP relaxes smooth muscle, causing bronchodilation.
Route of administration
1. Oral.
2. Aminophylline is the intravenous xanthine used in severe asthma attacks.
Indications
Xanthines are used in asthmatic children unable to use inhalers, and adults with predominantly nocturnal symptoms. They are administered intravenously in status asthmaticus.
Contraindications
Cardiac disease, hypertension, hepatic impairment.
Adverse effects
Nausea, vomiting, tremor, insomnia, tachycardia.
Therapeutic notes
Oral xanthines are formulated as sustained-release preparations. Xanthines often cause adverse effects, having a narrow therapeutic window, but are useful as oral drugs in preventing attacks for up to 12 hours. Infants with asthma who are very young can have difficulty using inhalers or nebulizers, and it is therefore more effective to give them theophylline, as this can be given in tablet form. Theophylline has a very narrow therapeutic range and so small increases above the therapeutic dose can be toxic and even fatal.
Leukotriene Receptor Antagonists
Montelukast and Zafirlukast are examples of leukotriene receptor antagonists.
Mechanism of action
The leukotriene receptor antagonists are believed to act at leukotriene receptors in the bronchiolar muscle, antagonising endogenous leukotrienes, thus causing bronchodilation. Leukotrienes are thought to be partly responsible for airway narrowing which is sometimes observed with the use of non-steroidal anti-inflammatory drugs (NSAIDs) in asthmatic people. The NSAIDs inhibit cyclooxygenase, and divert arachidonic acid breakdown via the lipoxygenase pathway, liberating leukotrienes among other mediators.
Route of administration: Oral.
Indications: Prophylaxis of asthma.
Contraindications: Elderly, pregnancy, Churg-Strauss syndrome.
Adverse effects: Gastrointestinal disturbance, dry mouth, headache.
Therapeutic notes: The leukotriene receptor antagonists are not yet widely used, though their potential as an agent in the combination therapy of asthma is becoming more widely accepted.
Hints and Tips: In an asthmatic emergency, when thinking what drugs to use, don’t forget oxygen.
Prophylactic and Anti-Inflammatory Drugs
Mast-Cell Stabilizers
Sodium cromoglycate and nedocromil sodium are examples of mast-cell stabilizers.
Mechanism of action
The exact modes of action of mast-cell stabilizers are unclear. These drugs appear to stabilize antigen-sensitized mast cells by reducing calcium influx and subsequent release of inflammatory mediators.
Route of administration
Inhaled.
Indications
Mast-cell stabilizers are useful in young patients (< 20 years old) with marked allergic disease and moderate asthma.
Adverse effects
Cough, transient bronchospasm, throat irritation.
Therapeutic notes
Mast-cell stabilizers have a prophylactic action; they must be taken regularly for several weeks before any beneficial effects are noted. These drugs are therefore not of use in acute asthma attacks.
Glucocorticoids
Anti-inflammatory glucocorticoids include beclometasone, fluticasone, budesonide and prednisolone.
Mechanism of action
Corticosteroids depress the inflammatory response in bronchial mucosa and so diminish
bronchial hyper responsiveness. The specific effects include:
➤ Reduced mucosal oedema and mucus production
➤ Decreased local generation of prostaglandins and leukotrienes, with less inflammatory-cell activation
➤ Adrenoceptor up-regulation
➤ Long-term reduced T-cell cytokine production, and reduced eosinophil and mast-cell infiltration of bronchial mucosa.
For the intracellular events involved in corticosteroid action see respective chapter
Route of administration
Corticosteroids are usually delivered by metered-dose inhaler. Oral and intravenous administration is reserved for severe asthma and status asthmaticus.
Indications
Corticosteroids are used in patients with more than minimal symptoms, often in combination with 32-agonists or drugs that block allergies.
Contraindications
Caution in growing children and in those with systemic and local respiratory/ear, nose and throat (ENT) infections.
Adverse effects
Dysphonia, oral thrush and systemic distribution in high dosage. If given orally, cushingoid effects may occur.
Therapeutic notes
The initial treatment of severe or refractory asthma may require oral corticosteroids. If possible, maintenance should be achieved with inhaled corticosteroids via a metered dose, to minimize side-effects. Inhaled corticosteroids are usually effective in 3-7 days, but must be taken regularly.
Use of Inhalers, Nebulizers and Oxygen
In the treatment of asthma, inhalers and nebulizers are used to deliver drugs directly to the airways. This allows higher drug concentrations to be achieved locally, while minimizing systemic effects. Whatever device is used, less than 15% of the dose is deposited on the bronchial mucosa.
Inhalers
There are several types of inhaler: metered dose, breath-activated spray, breath-activated powder. They vary in cost, delivery efficiency and ease of use. Spacer devices, used in conjunction with inhalers, improve drug delivery and are easy to use. Spacers are particularly effective in children. inbong
Nebulizers
Nebulizers convert a solution of drug into an aerosol for inhalation. They are more efficient than inhalers and are used to deliver higher doses of drug. They are useful in status asthmaticus and for the acute hospital treatment of severe asthma.The long-term use of nebulizers is limited by cost, convenience and the danger of patient over- reliance.
Oxygen
High-flow oxygen should be given to any patient in respiratory distress unless they have COPD and a ‘hypoxic drive’. In this situation, oxygen can be administered, but at a lower concentration. Oxygen increases alveolar oxygen tension and decreases the work of breathing necessary to maintain arterial oxygen tension.
Allergic Rhinitis
‘Rhinitis’ means an inflammatory response of the membrane lining the nose. “Allergic rhinitis’ means that the inflammatory response is due to specific allergens causing a type 1 hypersensitivity reaction. Based on symptoms, it may be further classified as seasonal or perennial (throughout the year). The inflammation can cause swelling, blockages to airflow and overactivity of the mucous membrane glands, causing excessive mucus production. Allergic rhinitis is treated with antihistamine drugs or local steroid sprays. Decongestants can sometimes be helpful.
Decongestants
Nasal decongestion can occur acutely, or be a chronic disorder. Decongestion relies on administration of agents which ultimately have sympathomimetic effects. This results in vasoconstriction of the mucosal blood vessels of the nose, and a reduction in oedema and secretions.
Ephedrine
This drug is the most commonly used decongestant.
Mechanism of action: Ephedrine’s sympathomimetic activity results in vasoconstriction of nasal blood vessels, limiting oedema and nasal secretions.
Route of administration: Topical or oral.
Indications: Nasal congestion.
Contraindications: Caution in children.
Adverse effects: Local irritation, nausea, headache. Re-bound nasal congestion on withdrawal.
Therapeutic notes
Oral preparations are less effective than topical, and are contraindicated in diabetes, hypertension and hyperthyroidism.
Respiratory Stimulants and Pulmonary Surfactants
Respiratory Stimulants
Respiratory stimulants, or analeptic drugs, have a very limited place in the treatment of ventilatory failure in patients with chronic obstructive airways disease. They have largely been replaced by the use of ventilatory support. Example drugs are naloxone, flumazil and Doxapram.
Doxapram
Mechanism of action
Doxapram is used to improve both rate and depth of breathing. Doxapram is a central stimulant drug that acts on both carotid chemoreceptors and the respiratory centre in the brainstem to increase respiration.
Route of administration: Intravenous.
Indications: Acute respiratory failure.
Adverse effects: Perineal warmth, dizziness, sweating, increase in blood pressure and heart rate.
Pulmonary Surfactants
Pulmonary surfactants are used in the management of respiratory distress syndrome, which is most common amongst premature babies. Pulmonary surfactants act to decrease the surface tension of the alveoli, and allow ventilation to occur more easily. They are usually administered via endotracheal tubes directly into the pulmonary tree.
