All about Tetanus – Basic microbiology, parasitology, and immunology; nature, reproduction, growth, and transmission of common microorganisms and parasites in Bangladesh; prevention including universal precaution and immunization, control, sterilization, and disinfection; and specimen collections and examination. Students will have an understanding of common organisms and parasites caused human diseases and acquire knowledge about the prevention and control of those organisms.
All about Tetanus
Morphology of Clostridium Tetani:
- Rod shaped with rounded ends.
- Produces a spherical, terminal spore which is larger than the bacillary body. This gives van A the organism the characteristic appearance of a ‘tennis racket
- Non-capsulated.
- Motile with peritrichous flagella (slow and steady movement).
- Gram positive and non-acid-fast.
Types of Tetanus:
- Otogenic tetanus
- Tetanus neonatorum
- Post-operative tetanus
- Cryptogenic tetanus
Definition of Tetanus
Tetanus is a wound infection caused by Cl. Tetani occurring usually in the deep, contused, soil contaminated injuries with pyogenic organism it containing foreign bodies.
or
Tetanus is wound, caused by exotoxin of clostridium tetani characterized by painful paroxysmal spasm of voluntary muscle and muscular rigidity.

Figure: A patient who has tetanus
A. Incubation period: 6-10 days
B. Agent factors:
- Agent: Clostridium tetani is a Gram positive, spore bearing and anaerobic bacteria.
- Reservoir of infection: Soil and dust, intestine of herbivorous animals (eg. cattle,
C. Patient factors:
- Occupation: Agricultural workers mostly affected
- Immunity: No age is immune unless protected by immunization
Route of Entry of Tetanus
The organism gains access to the body via various wounds, including –
- The organism gains access to the body via various wounds, including –
- Apparently trivial injuries (eg. Puncture wounds, including those caused by splinters and rose thorns)
- Animal bites
- Human bites
- Open fractures
- Burns
- Gangrene
- Frostbite
- Chronic decubitus ulcers
- Abscesses
- Parenteral drug abuse as a complication of intramuscular injection, especially of quinine.
In neonates, especially the infants of non-immune mothers, infection can occur via infected umbilical stumps. The risk is increased by unhygienic midwifery practices, such as applying animal dung to the umbilical stump.
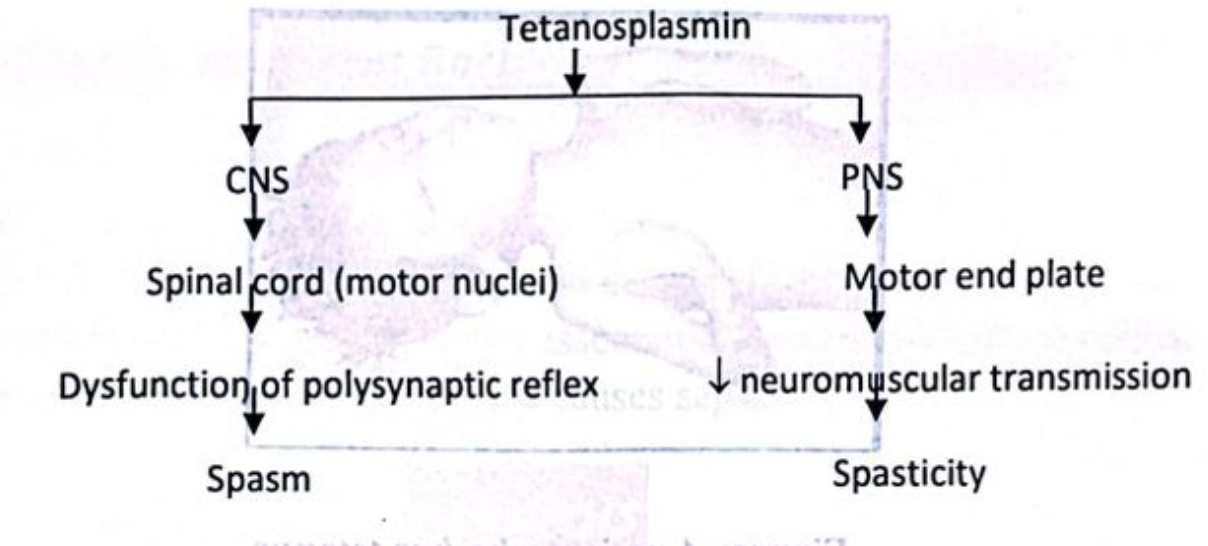
Pathogenesis of Tetanus
Clinical Features (C/F) of Tetanus
A. Prodromal stage:
- Dysphagia
- Severe neck pain, back pain and pain in abdomen
- Wound pain
B. Stage of tonic rigidity:
- Trismas/lock jaw
- Spasm of masseter muscle
- Earliest sign
- Muscle spasticity
- Risus sardonicus: Contraction of the muscles of angle of mouth and frontalis
- Opisthotonus: Spasm of muscle of back and limbs
C. Stage of clonic spasm:
- Laryngeal and pharyngeal spasm
- Respiratory fixation
Laboratory Diagnosis of Tetanus:
Principle:
Finding out of the causative organism confirms the diagnosis of tetanus.
Steps:
1. Specimen collection:
- Wound swab.
2. Microscopic examination:
- Gram staining: Finding – Gram-positive bacilli (tennis racket appearance)
3. Isolation & identification from culture:
- Robertson’s cooked meat media
- Finding – Turbidity of medium & blackening of meat
4. Other tests:
- Agglutination test.
- Toxigenicity test.
- Animal inoculation test
Treatment of Tetanus:
1. Administration of antitoxin: Immediate administration of TIG (Tetanus immunoglobulin): 3,000-10,000 units in intravenous route.
2. Wound care: Exploration, cleaning and debridement of wound
3. Antibiotic: Benzyl penicillin 600mg I.V. 6 hourly or Metronidazole if allergic to penicillin
4. Anticonvulsant therapy:
- Quiet room
- Muscle relaxants.
- Sedatives (Diazepam in IV route).
5. Respiratory support: Tracheostomy, if needed
6. General measures: Maintain nutrition by sufficient food and fluids
Prevention of Tetanus
Women of reproductive age (15-45 years)
| TT doses | Minimum interval between doses | Years protected |
| TT-1 | 0 | |
| TT-2 | 0 | 3 years (from 15 days after the administration of TT – 2) |
| TT-3 | 6 month after TT-2 | 5 years (from 15 days after the administration of TT-3) |
| TT-4 | 1 years after TT-3 | 10 years (from 15 days after the administration of TT-4) |
| TT-5 | 1 years after TT – 4 | lifelong protected |
Antenatal: Pregnant mother should be immunized with 2 doses of tetanus toxoid within 16-28 weeks of pregnancy
Postnatal:
- Vaccine DPT at 6th, 10th and 14th weeks of birth.
- Booster dose: After 1 year
Tetanus prophylaxis in an injured patient: It depends on immunization status of wound, eg
A) Clean wound:
a) Without previous immunization,
- 1st dose Inj. TT 5 cc IM stat
- 2nd dose 6-12 weeks later
- 3rd dose after 6-12 months
- And booster dose every 5 years interval
b) Previously immunized but no booster dose within 5 years –
- Inj. TT 5 cc IM stat single dose
B) Tetarius prone wounds/Dirty wound:
a) Non-immunized
- Passive immunization with: Inj. TIG 250 unit IM stat
- Active immunization with: Inj. TT 5 cc IM state and repeat at 126 month
b) Immunized
- Inj. TIG 250 unit IM stat
Complication of Tetanus:
1. Aspiration pneumonia
2. Atelectasis
3. Cyanosis
4. Asphyxia due to spasm of respiratory muscle and laryngospasm
5. Tongue bite
6. Intramuscular hematoma
7. Vertebral fracture
8. Peripheral neuropathy
9. Hyperhydrosis, cardiac arrhythmia
10. Dehydration and PEM in prolonged case

Toxins Produced by Clostridium Tetani
- Tetanoplasmin
- Tetanolysin
