Anaemia in pregnancy – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Anaemia in pregnancy
Anaemia:
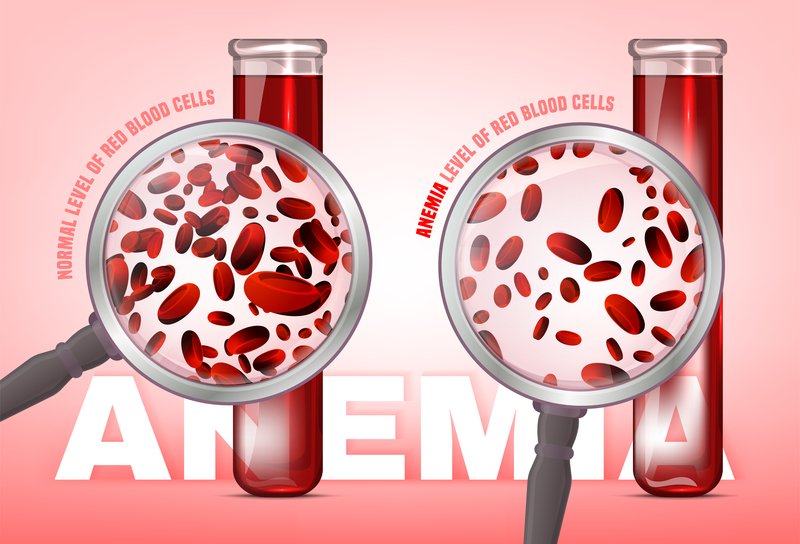
Anaemia is defined as reduce concentration of haemoglobin in the blood in respect of age and sex of a person.
According to WHO:
When the haemoglobin concentration in peripheral blood is <11 gm/dl it is termed as anaemia of pregnancy.
Causes of anaemia in pregnancy:
A. Physiological anaemia of pregnancy.
B. Pathological anaemia:
1. Decreased intake/deficiency anaemia:
➤ Iron deficiency.
➤ Folic acid deficiency.
➤ Vitamin B12 deficiency.
➤ Protein deficiency.
2. Increased loss / haemorrhagic:
➤ Acute: Following bleeding in early months or APH.
➤ Chronic: Hookworm infestation, bleeding PUD, bleeding haemorrhoids etc.
3. Hereditary:
➤ Thalassaemia
➤ Sickle cell anaemia
➤ Hereditary haemolytic anaemia.
➤ Other haemoglobinopathies,
4. Bone marrow insufficiency: Hypoplasia or aplasia due to radiation, drugs (Indomethacin, aspirin etc.)
5. Anaemia due to chronic disease: Chronic renal failure
6. Anaemia due to infection: Malaria, TB
Physiological anaemia:
During pregnancy there is disproportionate increase in plasma volume, RBC volume & Hb%. On the other hand there is marked demand of extra iron during pregnancy especially 2nd half witch cause further reduction in the iron conc. & ultimately physiological iron deficiency anaemia.
Criteria of physiological anaemia:
➤ Haemoglobin concentration: 10 gm/dl
➤ Total count of RBC: 3.2 million/mm3
➤ PCV: 30%
➤ Peripheral blood film: Normal morphology of the RBC with central pallor.

Cause / factors responsible for physiological anaemia during pregnancy:
➤ Increased demand of iron during pregnancy including:
✓ Multiple pregnancies
✓ Short interval between two conceptions
➤ Diminished intake of iron:
✓ Faulty dietary habit
✓ Nausea, vomiting
✓ Low socioeconomic condition.
➤ Disturbed metabolism: Faulty absorption, diminished erythropoiesis
➤ Pre-pregnant poor health status.
Common anaemia in our country:
Physiological anaemia is common in our country.
Etiological factors: Please see above.
Management of anaemia:
Clinical features:
Symptoms:
➤ Weakness.
➤ Lassitude & a feeling of exhaustion.
➤ Palpitation
➤ Anorexia
➤ Indigestion
Signs:
➤ Pallor of varying degree.
➤ Evidence of glossitis & stomatitis.
➤ Koilonychia.
➤ Oedema (may be due to hypoproteinaemia or associated pre-eclampsia).
➤ Precordium examination: A soft systolic murmur may be heard in the mitral area due to physiological mitral incompetence.
Investigations:
Iron deficiency anaemia:
➤ Blood picture:
✓ Reduced Hb%, MCV, MCH & MCHC
✓ PBF findings: Microcytic & hypochromic RBC with anisocytosis & poikilocytosis.
➤ Biochemical findings:
✓ Serum iron, ferritin & percent saturation-& ↑serum total iron binding capacity.
Folate deficiency anaemia:
➤ Blood picture:
✓ Hb% is reduced, but MCV is increased (macrocyte).
✓ PBF findings: RBCs are macro-ovalocyte, normochromic or hypochromic with anisocytosis & poikilocytosis.
✓ Howel-Jolly bodies & megaloblast may be found.
➤ Bone mafrow examination: Megaloblasts are found
➤ Special test: Serum & red cell folate assay
Treatment of anaemia:
In severe anaemia irrespective of the cause:
➤ First according to the patients’ blood group transfuse 2 units of fresh human blood after proper grouping and cross matching.
➤ Then again estimate the Hb% of the person.
➤ If it is not corrected then give blood again.
➤ If it is corrected then find out the cause and treat accordingly.
Treatment of iron deficiency anaemia:
General treatment:
➤ Diet: A realistic balanced diet rich in protein, iron & vitamins.
➤ Effective therapy to cure the disease contributing to the cause of anaemia
Specific treatment:
➤ Oral iron therapy: Ferrous sulfate 200mg-lgm/day intab or cap form. A maintenance dose 200-400 mg/day should be continued for at least 100 days to replenish iron store.
➤ Parenteral (I/V or I/M) iron therapy: In case of severe iron deficiency anaemia.
➤ Intra-venous route / total dose infusion (TDI): Given the total iron deficit after calculation as a single bolus dose with infusion as I/V drip in the form of iron dextran.
➤ Intra-muscular: Iron dextran or iron-sorbitol complex.
➤ Blood transfusion: In some selected cases.
Management during puerperium:
➤ Prophylactic antibiotic to prevent infection.
➤ Iron therapy should be continued for at least 100 days to replenish the iron store.
Treatment of folate deficiency anaemia
Specific folic acid therapy:
➤ 4 mg daily per-oral which should be continued for at least 4 weeks following delivery.
➤ Supplementary I/M vitamin B12 100 µgm (daily or in alternate days) may be added when response to folic acid alone is not adequate.
➤ Ascorbic acid 100 mg tablet 3 times daily; enhances the action of folic acid by converting it into folic acid.