Safety: Applying restraints & railing – Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialisms with differing levels of prescriber authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurses are permitted by most jurisdictions to practice independently in a variety of settings depending on training level. In the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient’s family, and other team members, that focus on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of an interdisciplinary healthcare team such as therapists, medical practitioners, and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
Safety: Applying restraints & railing
Definition of Restraint:
Restraint may be defined as mechanical devices used to immobilize and protect patient from injury or to facilitate examination, treatment and care.
or
Restraints are defined as any manual method or physical or mechanical device, material, or equipment attached to or adjacent to the resident’s body that the individual cannot remove easily and restricts freedom of movement or normal access to one’s body
or
Medical restraints are physical restraints used during certain medical procedures to restrain patients with the minimum of discomfort and pain and to prevent them from injuring themselves or others.
Purposes of Applying Restraints:
1. To provide safety
2. To facilitate examination.
3. Maintain the patients physical comfort.
4. To maintain medical asepsis
5. To assess the patient adequately.
6. To carry out diagnostic and therapeutic procedures.
7. To keep the child in desired position.
Types of Restraints:
There are many types of medical restraint:
1. Four-point restraints fabric body holders, straitjackets are typically only used temporarily during psychiatric emergencies.
2. Restraint masks to prevent patients from biting in retaliation to medical authority in situations where a patient is known to be violent.
3. Lap and wheelchair belts, or trays that clip across the front of a wheelchair so that the user can’t fall out easily, may be used regularly by patients with neurological disorders which affect balance and movement.
4. All four side rails being in the upright position on a bed can be considered a restraint,

figure: Different types of restraints
5. Safety vests and jackets can be placed on a patient like any other vest garment. They typically have a long strap at each end that can be tied behind a chair or to the sides of a bed to prevent injury or to settle patients for satisfying basic needs such as eating and sleeping. Posey vests are commonly used with elderly patients who are at risk of serious injury from falling.
6. Limb restraints to prevent unwanted activity in various limbs. They are wrapped around the wrists or ankles, and tied to the side of a bed, to prevent self-harm, harm to medical staff, or as punishment for physical resistance to medical authority.
7. Mittens to prevent scratching are common for newborns, but may also be used on psychiatric patients or patients who manage to use their hands to undo limb restraints.
8. A Papoose board can be used for babies and young children.
9. Chemical restraints are drugs that are administered to restrict the freedom of movement or to sedate a patient.
Procedure of Applying Restraints:
A. Articles Required for applying Restraints:
- Draw sheet or baby blanket for the babies(newborn).
- Elbow restraint cloth with 5-6 pockets in which spatulas are kept.
- Clove hitch-4″ bandage, cottonpads, knitted bandage.
- Pading to protect bony prominences.
B. Procedure
1. Ensure that enough personnel are available to properly control the patient and establish the restraints.
2. Explain the purpose of the restraints.
3. Physically control the patient and apply restraints.
4. Complete Primary and Secondary Assessments.
A. Restrained extremities should be evaluated for pulse quality, capillary refill time, color, sensory and motor function continuously
- a) Restraints must be adjusted if any of these functions are compromised.
- b) Restraints must not interfere with medical treatment.
5. Attempt to identify common physical causes for patient’s abnormal behavior. Hypoxia Hypoglycemia Head Trauma ETOH/ Substances use/ abuse
6. Patient should be secured to a backboard or stretcher only. Patients must never be secured directly to a vehicle or immovable object.
7. Transport patient.
8. Contact medical control.
9. Inform hospital that restraints are in place and assistance will be necessary to continue restraint of the patient
ISOLATION
It is defined as “separation, for the period of communicability of infected persons or animals from others in such places and under such conditions, as to prevent or limit the direct or indirect transmission of the infectious agent from those who are susceptible, or who may spread the agent to others.
Purposes/Important of Isolation:
1. To protect the community by preventing transfer of infection from the reservoir to the possible susceptible hosts.
2. Isolation has a distinctive value in the control of some infectious disease. E.g. Diphtheria, Cholera, streptococcal respiratory disease.
Types of Isolation:
1. Standard isolation
2. Strict isolation
3. Protective isolation
4. High security isolation
Definition of Isolation Technique:
Isolation technique, a medical aseptic practice, inhibits the spread and transfer of pathogenic organ by limiting the contacts of the patient and creating some kind of physical barrier between the patient and others.
Procedure of Isolation Techniques:
Isolation technique: The nurse follows isolation technique to prevent the transmission of infection from microorganisms by preventing pathogens from living the room of the infected patient from entering the room of a highly susceptible patient.
A. The supplies and equipment needed for isolation technique are as follow:
a) Isolation/grown, masks, gloves
b) Clean linen
c) single and double isolation bag
d) Paper towel
e) Running water
f) Soap with dispenser
g) Holder for isolation bag and laundry bag
B. Steps of isolation technique:
1. Determine causative organism or effectiveness of patients’ immune system
2. Recognize the mode of transmission and show microorganism exists in the body
3. Follow hospital policy for specific type of isolation used.
4. Provide environment with adequate equipment and supplies-
- Private room for isolation with anteroom
- Sign stating isolation category
- Adequate hand washing facility
- Special containers for trash, soiled linen and sharp instrument, such as needle
5. Plan time to explain isolation technique to patients family and visitors
6. Postcard on door of patient’s room or wall outside room stating the protective measure is use for patient care.
7. Supply the room with designated linen containers for soiled linen and for trash.
CLEANLINESS
Definition of Cleanliness:
Cleanliness is both the abstract state of being clean and free from dirt, and the process of achieving and maintaining that state. Washing is one way of achieving physical cleanliness, usually with water and often some kind of soap or detergent.
Purposes/Importance of Cleanliness:
1. To leave a clean polished surface where possible, so that dirt may be not be accumulated.
2. To remove all dust, dirt and breeding pieces of microorganism with the least disturbance to the patients
3. To prolong the life of the articles
4. To keep the articles in such a condition that they are ready for use at any time.
5. To maintain the aesthetic factors.
General Rules of Cleaning Method:
1. Dry dusting is never advisable. It spreads disease easily.
2. Dusting should be done after sweeping only
3. Use a dump duster to collect dust
4. Dust with clean duster
5. Collect dust at one place to avoid flying from place to place.
6. Dusting should be done without disturbing or removing the patients from bed.
7. Dusting should be done from top to bottom, i.e. from upward to downward direction
8. When dusting take care not to spoil the beds or walls or other fixers in room or hospital ward.
9. While dusting wounds or dressing should not be opened by other staff.
10. There should be a definite time for dusting daily.
Cleaning Procedure of Hospital Ward
The methods of cleaning described are essentially based on the common practice of manual cleaning using brooms and mops. Cleaning using mechanical equipment has made great in roads in the health facilities across the world. However it is capital intensive and trained manpower is required to handle the equipment, but cleaning is more efficient and a bigger area can be cleaned in lesser time. It will be worth procuring mechanical cleaning equipment especially in the larger facilities.
Preparation for cleaning
Different areas require different levels of cleanliness, e.g. the OPD and waiting areas do not require a very high level of cleanliness as compared to that of the Operation theatre or the ICU.
As far as possible wet mopping is preferred over dry sweeping to avoid kicking up and circulation of dust and allergens.
Preparation:
1. Put gumboots or disposable shoe covers .
2. Hand-Gloves must always be borne by all personnel engaged in cleaning of Health Facility
3. Wear cap, mask, apron / gown
4. Prepare germicidal cleaner (phenyl) in clean water as per the dilution directions mentioned on the product label, both in the wringer bucket as well as plastic pail.
5. Move cots and furniture as per the directions of the supervisor to one side.
6. Use a blunt knife to remove any dried up or sticky soil on the floor.
7. Use a treated dry mop or nylon push broom and dust pan to clear the loose soiling on the floor.
Performance
1. Sweep the dust in case the quantity is large- to the door way and collect it in the dust pan and discard into the trash.
2. Wet the mop in the germicidal solution (phenyl) and wring it gently so that the mop holds enough solution for necessary disinfection of the floor.
3. Wet mop the floor in one direction and ideally from the centre outwards toward the door. Change of mopping water should be done frequently especially when it is noticed that it is noticed dirty
Direction of cleaning
1. The sweeping movement should be maidirectional
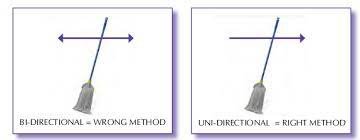
2. The direction of cleaning in healthcare facilities must be from the clean to the dirty area. In closed spaces like a ward the direction should be from within outwards,
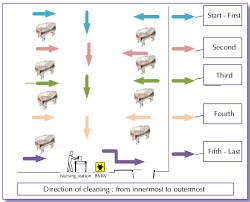
Direction of cleaning: from innermost to outermost
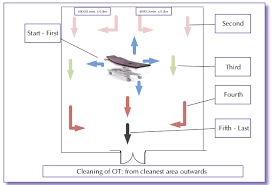
Cleaning of 07: from cleanest area outwards
3. Clean the furniture and cot castors with a clean duster using the germicidal solution prepared in the plastic pail, directly or with a spray bottle.
4. Put the tables and cots back in position.
5. Take out all your cleaning equipment and tools out of the door
6. Scan the room to ensure that cleaning is done thoroughly and none of personal belonging/ cleaning equipment left behind in the operation room.
7. Keep your equipment and tools to designated place, after rinsing in fresh germicidal solution.
8. Remember to clean the door stoppers and the door handles and latches which are usually left or not attended to.
Finishing
1. De-gown carefully, wash and let them dry.
2. Remove your cap and mask wash and let them dry.
3. Remove the gloves wash and let them dry.
4. Wash your hand as per standard procedure
Practical suggestions
2. All loose particles and litter should be removed before dealing with any stubborn stains/dirt.
3. Use lighter cleaning methods before attempting stronger methods.
4. Before any implement or cloth is used, make sure they are clean and dry.
5. If possible, use a double bucket system when mopping the floors so that dirty water is not reused while mopping. The first bucket contains clean water while the second bucket is used to squeeze out the water from the dirty mop following which the mop is dipped in the clean water and mopping done.
6. The Three bucket system should be ideally practised and that the first bucket contains wateralm with detergent used in the beginning. The mop is then rinsed in the second bucket and dipped in the third bucket which can also contain a disinfectant and the mopping done again..
7. Abrasives should be used as a last resort as they can damage the surface.
8. Use an agent that is least offensive in smell if alternatives are available.
9. When cleaning a surface, be cautious of marring the surroundings area, e.g. finger prints on walls, grazing other articles, etc.
10. Use methods that are least inconvenient to patients. Disturbance can be caused by noise or obstacles placed in public areas.
11. Be sure that during the process of cleaning areas do not become accident-prone,e.g. wet, slippery floors, etc. If required, cautionary sign can be put.
12. Cleaning should be carefully planned to make efficient use of time.
In a Health Facility, Chlorine Solution is used often for disinfection of surfaces, plastic waste, etc. Commonly, source of the Chlorine is either bleaching powder or commercially available Hypochlorite solution. Following points must be considered, whenever Chlorine Solution is being used
1. The solution should be freshly prepared.
2. Effectiveness of solution decreases with passage of time and presence of organic matter.
There is often spill of body fluids & mercury in Health Facilities. Such spillage requires careful cleaning and disinfection. Safety precautions are off wines. urporance for the staff and visitors.
Infection Control
Definition of Infection:
Infection may be defined as the invasion and multiplication of microorganisms such as bacteria, viruses, and parasites that are not normally present within the body. An infection may cause no symptoms and be subclinical, or it may cause symptoms and be clinically apparent.
or
Entry of a harmful microbe into the body and its multiplication in the tissues / bloodstream is called infection.
Define infection control
According to WHO infection control may be defined as “infection prevention and control measures aim to ensure the protection of those who might be vulnerable to acquiring an infection both in the general community and while receiving care due to health problems, in a range of settings. The basic principle of infection prevention and control is hygiene.”
or
Infection Control in a health care facility is the prevention of the spread of microorganisms from:
- Patient to patient
- Patient to Staff member
- Staff member to patient
General Measures of Infection Control:
A. Isolation
Assess the need for isolation. Screen all intensive care unit (ICU) patients for the following:
- Neutropenia and immunological disorder
- Diarrhea
- Skin rashes
- Known communicable disease
- Known carriers of an epidemic strain of bacterium
B. Observe hand hygiene
- World Health Organization’s five moments for hand hygiene
- Before touching a patient to protect the patient from harmful germs carried on your hands
- Before aseptic procedures to protect the patient against harmful germs, including the patient’s own germs
- After body fluid exposure/risk to protect yourself and the health care environment from the harmful patient’s germs
- After touching the patient – to protect yourself and the health care environment from the harmful patient’s germs
- After touching the patient’s surrounding – to protect yourself and the health care environment from the harmful patient’s germs.
D. Follow transmission-based precautions
a) Airborne precautions
- Isolate with negative-pressure ventilation
- Respiratory protection must be employed when entering the isolation room
b) Contact precautions
- Isolation is required
- Non-critical patient-care equipment should preferably be of single use. If unavoidable, then clean and disinfect them adequately before using to another patient
- Limit transport of the patient
- Droplet precautions
- Isolation is required
- Respiratory protection must be employed when entering the isolation room or within 6-10 ft of the patient. Limit transport of the patient
- Use specific strategies focused on prevention of specific nosocomial infections
E. Strategies to reduce VAP (ventilator-associated pneumonia)
- Avoid intubation whenever possible
- Consider noninvasive ventilation whenever possible
- Prefer oral intubations to nasal unless contraindicated
- Keep head elevated at 30-45° in the semi-recumbent body position
- Daily oral care with chlorhexidine solution of strength 0.12%
F. Strategies to reduce CRBSI (Catheter-related bloodstream infection)
- Prefer the upper extremity for catheter insertion. Avoid femoral route for central venous cannulation (CVC)
- Use maximal sterile barrier precautions (cap, mask, sterile gown and sterile gloves) and a sterile full-body drape while inserting CVCs, peripherally inserted central catheters, or guidewire exchange (IA)
G. Strategies to reduce UTI
- Insert catheters only for appropriate indications
- Follow aseptic insertion of the urinary catheter
- Maintain a closed drainage system
- Remove the catheter When it is no longer needed
H. Consider environmental factors
- • Cleaning and disinfection
- • Organizational and administrative measures
- Work with hospital administration for better patient to nurse ratio in the ICU
- Policies for controlling traffic flow to and from the unit to reduce sources of contamination from visitors, staff and equipment
- Waste and sharp disposal policy
- Education and training for ICU stafi about prevention of nosocomial infections