BED SORE – Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialisms with differing levels of prescriber authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurses are permitted by most jurisdictions to practice independently in a variety of settings depending on training level. In the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient’s family, and other team members, that focus on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of an interdisciplinary healthcare team such as therapists, medical practitioners, and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
BED SORE
Definition of Bed Sore
Bed sore or pressure sore is an ulcer occurring on the skin of any bed ridden patient, particularly over the bonny prominence due to pressure, circulation become slowly and finally the death occurs into the tissues

Bed sores also called pressure sores or pressure ulcers are injuries to skin and underlying tissue resulting from prolonged pressure on the skin. Bedsores most often develop on skin that covers bony areas of the body, such as the heels, ankles, hips and tailbone.
or
A bed sore or pressure sore or decubitus ulcer is an ulcer occurring on the skin of any bed ridden patient, particularly over bony prominences or where two skin surfaces press against each other. Due to pressure, circulation becomes slow and finally death of tissues occurs.
Causes of Bed Sore:
A. Direct or immediate causes:
a) Pressure-pressure is the basic cause of the bed sore.
- The weight of the body continuously remaining in one position.
- Splints
- Casts
- Bandage
b) Friction-friction of the skin with rough bedding causes injury to the skin.
- Wrinkles in the draw sheet or other bed cloths.
- Chipped or rough bedpan and its careless handling.
- Hard surfaces of plaster casts and splints.
c) Moisture-
- Leaving patient lying on wet bedding.
- Patients with incontinence of urine and stool.
- Severe perspiration.
- Body discharges.
d) Pressure of pathogenic organisms: Due to unhygienic condition pathogenic organism multiples and infection settles on the skin.
B. Indirect or predisposing causes;
a) Paralysis and limitation of movement.
b) Emaciated and malnourished patients.
c) Edematous patients.
d) Very old with sluggish circulation.
e) Obese patients.
f) Patient with spinal injury.
g) Incontinent patient.
h) Patient with long term illness, fracture etc.
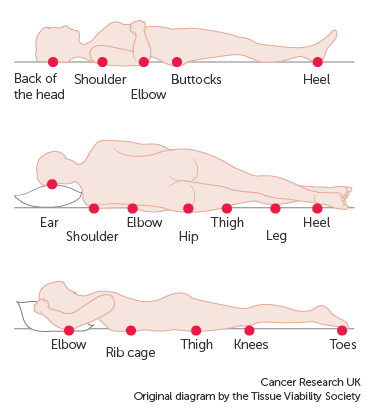
Common Sites of Bed Sore:
A. In the supine position
1. Occiput
2. Scapula
3. Sacral region
4. Hips
5. Elbow
6. Heels
B. In prone position
1. Ears
2. Cheeks
3. Acromian process
4. Breast in females
5. Genitelia
6. Knees and toes
C. In side-lying position
1. Ears
2. Acromian process of shoulder.
3. Ribs
4. Greater trochanter of hipe
5. Medial and lateral condyles of knee
6. Maleolus of ankle joint.
Stages of Bed Sores:
There are mainly four stages of bed/pressure soresnie
1. Stage 1
The beginning stage of a pressure sore has the following characteristics:
➤ The skin is not broken.
➤ The skin appears red on people with lighter skin color, and the skin doesn’t briefly lighten (blanch) when touched.
➤ On people with darker skin, the skin may show discoloration, and it doesn’t blanch when touched.
➤ The site may be tender, painful, firm, soft, warm or cool compared with the surrounding skin.
2. Stage 2
➤ The outer layer of skin (epidermis) and part of the underlying layer of skin (dermis) is damaged or lost.
➤ The wound may be shallow and pinkish or red.
➤ The wound may look like a fluid-filled blister or a ruptured blister.
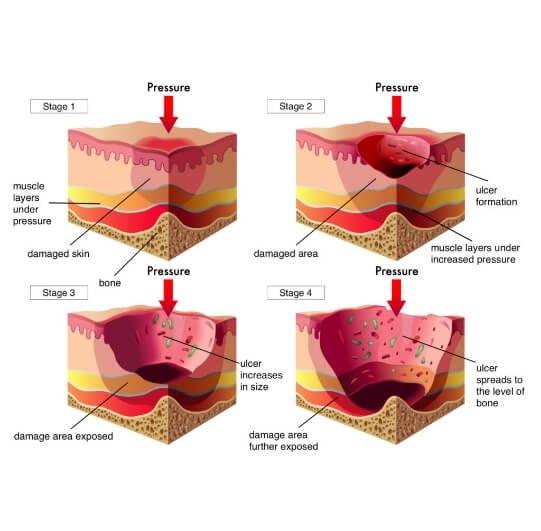
3. Stage 3
➤ The loss of skin usually exposes some fat.
➤ The ulcer looks crater-like.
➤ The bottom of the wound may have some yellowish dead tissue.
➤ The damage may extend beyond the primary wound below layers of healthy skin.
4. Stage 4
A stage IV ulcer shows large-scale loss of tissue:
➤ The wound may expose muscle, bone or tendons
➤ The bottom of the wound likely contains dead tissue that’s yellowish or dark and crusty.
➤ The damage often extends beyond the primary wound below layers of healthy skin.
Preventive Measures of Bed Sore:
1. Find out and detect the patients who are prone to the development of bed sores.
2. Daily observation of the pressure points and prompt reporting in case of suspicion.
3. Stimulate circulation by regular cleaning and back care, especially to pressure areas.
4. Relieve pressure by-
a) Moving the patient in the bed, change the position 2 hourly.
b) Use the comfort devices to take off the pressure from the pressure points e.g. air cushions, air rings etc.
c) Avoid the use of rubber rings
d) Use a bed cradle to take the weight off the linen, especially in children having rheumatic fever.
e) Use pillows between the legs. Do not allow two bony prominences to meet together.
f) Allow the patient to get up and walk about as soon as the doctor gives permission.
g) Take help while giving bed pans, and while removing bed pans.

Figure: Position in bed to prevent the development of bed sores
5. Avoid Friction by-
a) Well-made beds free from crumbs and wrinkles and with the bottom bedding tightly tucked in.
b) Proper and immediate changing the wet linen.
c) Give back care after each urination and defecation.
d) Do not use badly chipped or rough bedr.ans.
e) Use adequate amount of cotton under splints and plaster casts to avoid friction.
f) Special care should be taken during patient’s urination and defecation to prevent soiling of bed linens
6. Prevent injury by:
a) Cutting nails short of both nurses and patients.
b) Taking special care while giving and removing bed pan to avoid scratching skin. Better to use steel bed pans.
c) Help should be taken while moving the heavy and difficult patients.
d) If splints are used, these should be well padded
7. Diet:
a) Give a well-balanced diet with plenty of vitamins and proteins.
b) Plenty of fluids should be given to patient, restricted according to disease condition only.
Nursing Management of a Patient with Bed Sore:
1. Detect early sign and symptoms of bed sore and report them to the ward sister and physicians.
2. Prevent the ulcerated area from infection.
3. Use normal saline for cleaning the area.
4. if sioughing is more, use hyarogen peroxide solution also for cleaning and cut of the slough.
5. Apply heat for healing of the wound. Use a 100-watt electric bulb for 10 minutes.
6. Apply zinc oxide ointment on the surface of the ointment.
7. If infection is present, apply soframycine ointment locally and give systematic antibiotics after culture and sensitivity. Test of the pus swab, prescribed by the physician.
8. If there is delay in wound healing, skin grafting can be done.
9. Provision of nourishing food and supplementary vitamins for wound healing should be made.
