Benign Enlargement of Prostate (BEP) – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Benign Enlargement of Prostate (BEP)
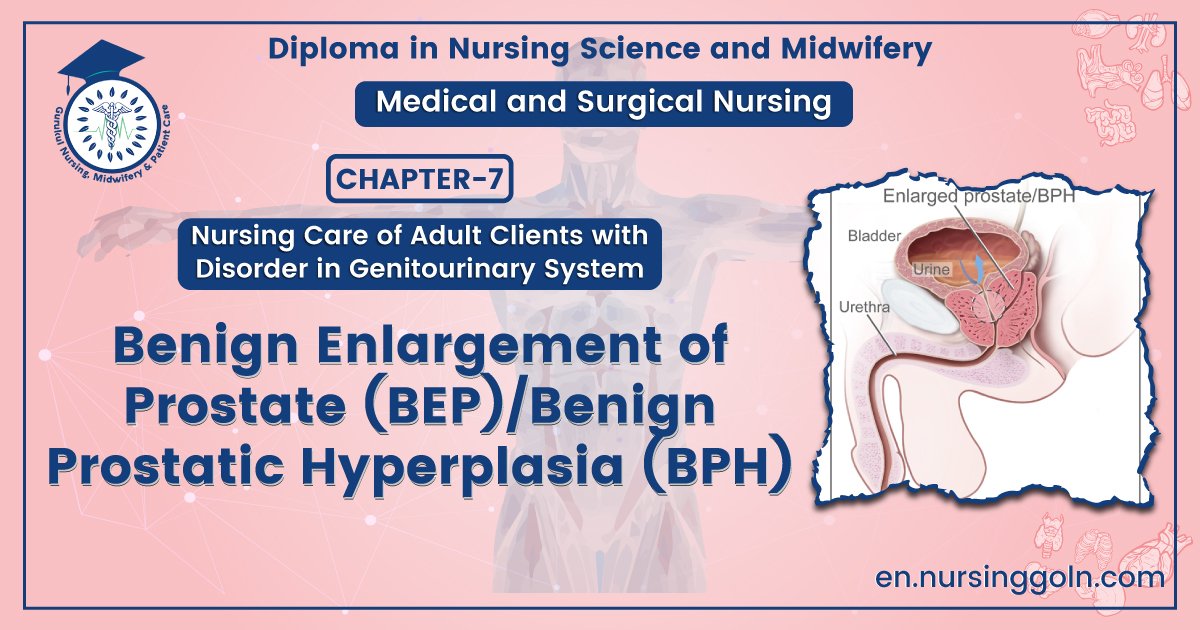
Definition of Benign Enlargement of Prostate (BEP)/Benign Prostatic Hyperplasia (BPH)
Benign prostatic hyperplasia (BPH) is a common urological condition caused by the non-cancerous enlargement of the prostate gland as men get older.
Management of BEP
Symptoms
- The need to frequently empty the bladder, especially at night.
- difficulty in beginning to urinate
- Dribbling after urination ends.
- decreased size and strength of the urine stream
- sensation that the bladder is not empty, even after a man is done urinating.
- inability to postpone urination once the urge to urinate begins
- Pushing or straining in order to urinate.
Sign’s
- Weak urinary stream
- Prolonged emptying of the bladder
- Abdominal straining
- Hesitancy
- Irregular need to urinate
- Incomplete bladder emptying
- Post-urination dribble
- Irritation during urination
- Frequent urination
- Nocturia (need to urinate during the night)
- Urgency
- Incontinence (involuntary leakage of urine)
- Bladder pain
- Dysuria (painful urination)
- Problems in ejaculation
Treatment of Benign Enlargement of Prostate (BEP)
A. General treatment:
a. Rest, reassurance, privacy, hot bath to diminish internal congestion
Advice: Fluid restriction and reduction of caffeine intake
Acute retention: By catheterization if fails supra-pubic cystostomy
Chronic retention:
- No need of catheterization (if good renal function)
- If uraemia, urgent catheterization
- IV fluid
- Blood transfusion
1. Medical treatment:
- a-blocker: Prazosine, terazosine
- 5-a reductase inhibitor (if prostate is large)
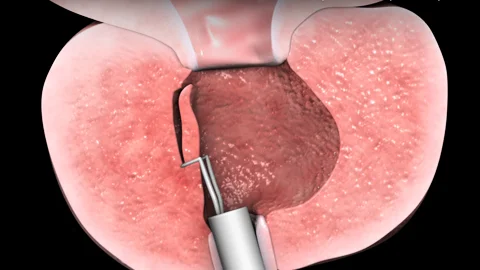
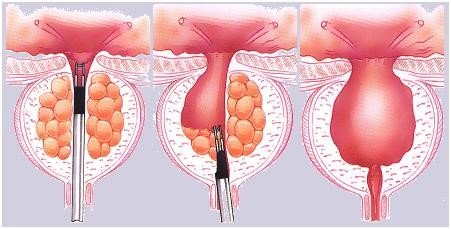
2. Surgical treatment:
- Trans-urethral resection of prostate (TURP) under spinal anesthesia
- Open prostatectomy
Complication of BEP or BPH
1. At prostatic level:
- Acute retention of urine
- Chronic retention of urine
- Haematuria
2. Bladder level:
- Diverticula
- Urinary infection
- Stone formation
3. Ureter and kidney level:
- Hydro-ureter
- Hydro-nephrosis
4. Effect on straining:
- Haemorrhoids
- Hernia
- Rectal prolapsed
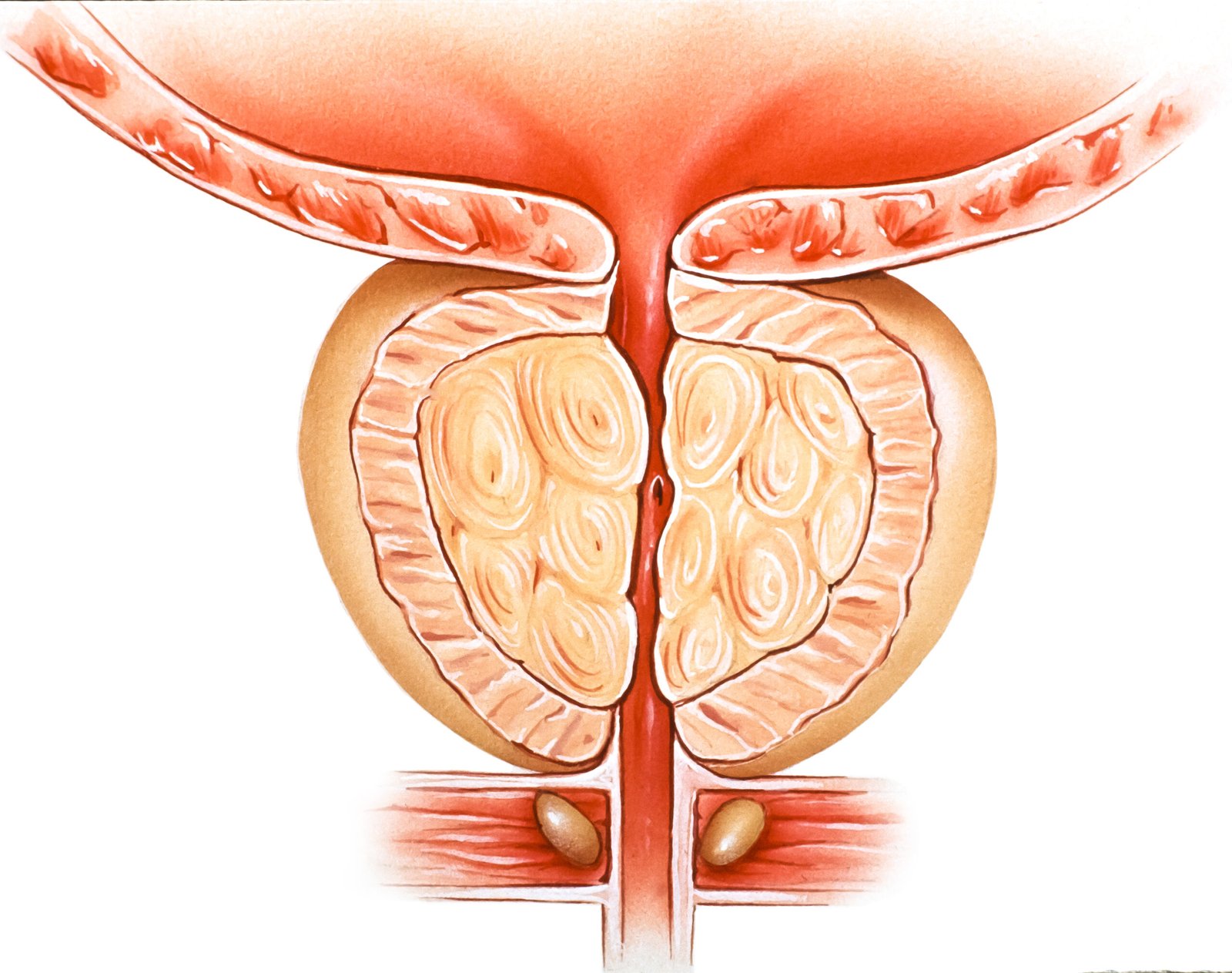
Pathophysiology
The pathophysiology of BPH is as follows:
- Resistance. BPH is a result of complex interactions involving resistance in the prostatic urethra to mechanical and spastic effects.
- Obstruction. The hypertrophied lobes of the prostate may obstruct the bladder neck or urethra, causing incomplete emptying of the bladder and urinary retention.
- Dilation. Gradual dilation of the ureters and kidneys can occur,
Definition of Prostatectomy
ctomy is the surgical removal of the prostate wherein the procedure could include all (radical) or part (simple). Prostatectomy is indicated in the treatment of benign prostatic hyperplasia while radical prostatectomy is indicated in the treatment of prostate cancer.
Advice Will Give To A Prostatectomy Patient During Discharge From The Hospital
- Diet: Stay hydrated with clear fluids rather than eating solid food until your bowel function and
appetite return to normal. Once that happens, follow a regular diet.
2. Incision care: Do not soak incision under water for two weeks. You may shower starting the second day after surgery.
3. Activity: No strenuous activity or lifting greater than 10 pounds for six weeks. Walking and climbing stairs are okay. Take several small walks each day. It is important to stand up and walk every one to two hours. This will help prevent blood clots in the legs. Stop any sexual activity until after you follow up with your doctor.
4. Foley catheter care: The Foley catheter is the tube that drains and collects urine.
- The catheter should have a curl in it and not be pulling on the penis. This is called “off
- tension.” A leg strap keeps the catheter in place so it doesn’t get tugged on and pulled out. Keep the drainage bag lower than the bladder. This allows gravity to drain the urine downward.
- The catheter should not be removed until 10-14 days after surgery. Only a urologist should remove it.
- Clean the catheter with soapy water once a day and apply either bacitracin ointment or
- vaseline to the tip of the penis as needed for comfort.
- If you are uncircumcised, remember to pull the foreskin back over the head or tip of your penis.
5. Pain Management: Take Tylenol® (acetaminophen) on a regular schedule to control your pain. Use oxycodone/ dilaudid for breakthrough pain. Do not take Tylenol in addition to Norco® or Percocet®, which also contain acetaminophen. Do not exceed 4000 mg of Tylenol in a 24-hour period.
6. Constipation: Constipation after surgery can lead to bleeding and other complications. It is important
to take a stool softener/laxative (such as Docusate Sodium and Senna) each day to prevent
constipation. Keep taking it until bowel function is regular and you are off pain medications.
7. Bladder Spasms: Bladder spasms can happen after surgery. They are not dangerous but may be
uncomfortable. These are signs of bladder spasms:
- Lower abdominal cramping pain
- A sudden or constant need to urinate despite the catheter draining urine
- Pain at the tip of the penis
Take Ditropan (oxybutynin) as needed for bladder spasms. Oxybutynin is for your comfort and to help prevent leakage of urine if the spasms are severe. The medicine can cause constipation and dry mouth.
8. Antibloties: An antibiotic has been prescribed to help prevent a bladder infection when the catheter is removed. You should take it for three days, starting the day before your foley catheter is removed. Take it as instructed and complete the entire prescribed course.
9. Call the doctor or nurse if you have any of these symptoms:
- Abdominal pain
- Bleeding
- Chest pain
- Fever of 101 degrees F or higher
- Nausea or vomiting
- Passing blood clots in urine
- Passing urine that looks like diluted ketchup
- Severe or uncontrolled pain Shortness of breath
- Swelling in arms or legs
Definition of Haemodialysis
Hemodialysis, also spelled haemodialysis, commonly called kidney dialysis or simply dialysis, is a process of purifying the blood of a person whose kidneys are not working normally. This type of dialysis achieves the extracorporeal removal of waste products such as creatinine and urea and free water from the blood when the kidneys are in a state of kidney failure.
Indication of Haemodialysis
| Indications of dialysis in acute renal failure (ARF) |
|
| Indications of dialysis in chronic renal failure (CRF) |
|