Today our topic of discussion is ” Cardiac Muscle and Electrical Activity “. The cardiovascular system’s driving force lies within the heart, an intricate blend of muscle and electric phenomena. The harmonious relationship between the cardiac muscle and its inherent electrical activity ensures the heart’s relentless function, pumping life-giving blood to every cell in our body. This article unpacks the complex interplay between the cardiac muscle and its electrical symphony.
Cardiac Muscle and Electrical Activity – The Cardiovascular System: The Heart
1. Cardiac Muscle: Not Just Another Muscle Type
The heart’s muscle, or myocardium, is a specialized tissue distinct from skeletal and smooth muscle.
a. Structure:
- Composed of short, branched cells called cardiomyocytes.
- These cells contain a single nucleus and are interconnected by intercalated discs, which facilitate rapid electrical and mechanical connections between cells.
b. Functional Characteristics:
- Automaticity: Cardiomyocytes possess an innate ability to contract without external nervous stimuli.
- Rhythmicity: The heart muscle contracts in a rhythmic manner, ensuring consistent blood flow.
- Extended Contraction Time: Unlike rapid skeletal muscle contractions, cardiac muscle contracts and relaxes over a more extended period, preventing muscle fatigue.
2. The Heart’s Intrinsic Electrical System
The heart’s rhythmic contractions are governed by its built-in electrical conduction system.
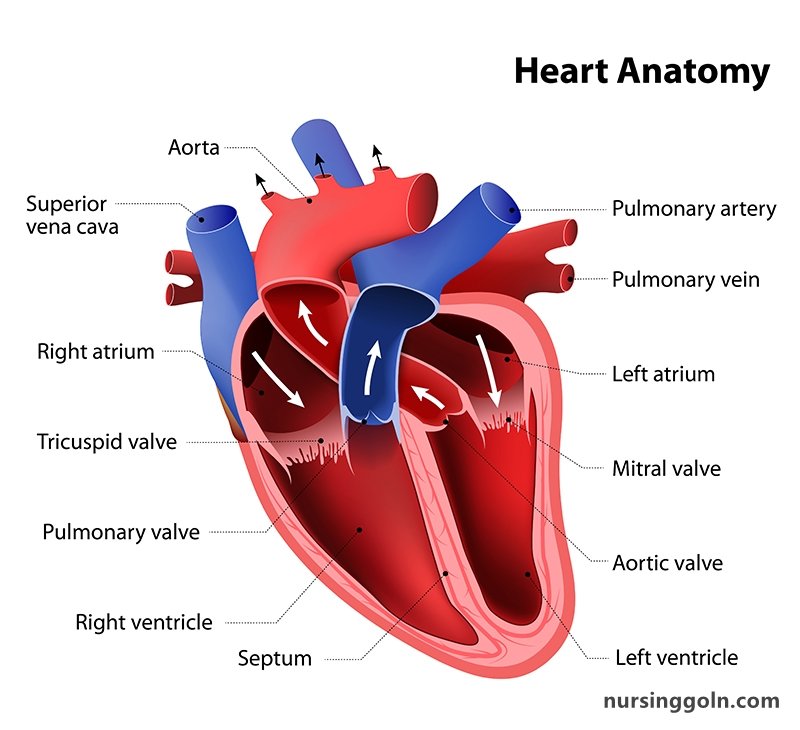
a. Sinoatrial (SA) Node: Dubbed the heart’s natural pacemaker, the SA node initiates electrical impulses. Located in the right atrium, it sets the heart rate by spontaneously generating electrical signals.
b. Atrioventricular (AV) Node: Acts as a relay station. Positioned between the atria and ventricles, it briefly delays the impulse, ensuring the atria contract fully before the ventricles.
c. Bundle of His and Bundle Branches: These pathways transmit impulses from the AV node to the heart’s apex.
d. Purkinje Fibers: Ending the electrical journey, these fibers distribute the impulse to the ventricular myocardium, triggering a coordinated contraction.
3. The Cardiac Action Potential
The heart’s electrical signals, or action potentials, are a series of ion exchange events across cardiomyocyte membranes.
a. Resting Membrane Potential: Cardiomyocytes, at rest, have a negative internal charge due to an uneven distribution of ions.
b. Depolarization: Triggered by the SA node, sodium channels open, allowing sodium ions to flood in, making the cell’s inside more positive.
c. Plateau Phase: A unique characteristic of cardiac muscle. As sodium channels close, calcium channels open, allowing calcium influx and maintaining depolarization.
d. Repolarization: Potassium channels open, letting potassium out, restoring the negative internal charge.
4. The Electrocardiogram (ECG/EKG)
The heart’s electrical activity can be visualized using an ECG.
a. P Wave: Represents atrial depolarization. b. QRS Complex: Signifies ventricular depolarization (and atrial repolarization, although it’s obscured by the QRS). c. T Wave: Corresponds to ventricular repolarization.
ECGs are indispensable diagnostic tools, helping detect arrhythmias, ischemia, and other cardiac abnormalities.
5. The Refractory Periods
A vital feature of cardiac muscle cells is their extended refractory period, preventing them from receiving another impulse immediately. This mechanism ensures that heartbeats are distinct events, preventing tetanic contractions.
a. Absolute Refractory Period: A period during which no new action potential can be initiated. b. Relative Refractory Period: Here, a stronger-than-normal impulse can stimulate another contraction.
6. Cardiac Excitation-Contraction Coupling
For each electrical impulse, there’s a corresponding muscle contraction. This phenomenon is mediated by calcium ions.
a. Calcium’s Role: Calcium influx during the plateau phase triggers calcium release from the sarcoplasmic reticulum within cardiomyocytes. b. Cross-Bridge Cycling: Calcium binds to troponin, causing a shift in tropomyosin and exposing binding sites on actin for myosin attachment. This process leads to muscle contraction.
7. Factors Influencing Heart’s Electrical Activity
Several factors modulate the heart’s electrical and contractile function:
a. Autonomic Nervous System:
- Sympathetic Stimulation: Increases heart rate and force of contraction.
- Parasympathetic Stimulation: Decreases heart rate.
b. Hormones: Adrenaline and thyroid hormones can increase the heart rate and force of contraction. c. Electrolytes: Particularly calcium, potassium, and sodium influence action potential generation and propagation.
8. Pathologies and Electrical Abnormalities
Various conditions can disturb the heart’s electrical function:
a. Arrhythmias: Abnormal heart rhythms due to malfunctioning in the conduction system. b. Ischemia: Reduced blood flow can impair electrical function, leading to arrhythmias. c. Heart Block: Impaired conduction, often at the AV node or Bundle of His, causing asynchronous atrial and ventricular contractions.

Conclusion
The synchronization between the cardiac muscle and its inherent electrical activity symbolizes nature’s precision engineering. The perpetual dance between ions, cells, and signals ensures our heart’s enduring rhythm, resonating with the very essence of life. Understanding this intricate relationship is pivotal, both for appreciating the marvel that is our heart and for pioneering interventions when its rhythm falters.
