Cervical cancer screening – This book covers the entire syllabus of “Community Health Nursing” prescribed by the Universities of Bangladesh- for Basic and diploma nursing students. We tried to accommodate latest information and topics.
This book is examination friendly setup according to the teachers’ lectures and examination’s questions. At the end of the book previous university questions are given. We hope in touch with the book students’ knowledge will be upgraded and flourished. The unique way of presentation may make your reading of the book a pleasurable experience.
Cervical cancer screening
Cancer screening
Cancer screening may be defined as the “search for unrecognized malignancy by means of rapidly applied tests.”
Methods of cancer screening
- Mass screening by comprehensive cancer detection examination
- Mass screening at single sites.
- Selective screening: This refers to examination of those people thought to be at special risk, for example example, porous women of lower socio-economic strata upwards of 35 years of age for detection of cancer cervix.
Risk factors of cervical cancer
1. Unusual bleeding or discharge;
2. Early coitus,
3. Multiple sexual partner;
4. Multiple pregnancy;
5. Vaginal infection;
6. Low socio-economic status;
7. STD leading syphilis and herpes genetslia
8. Uncircumcised partner;
9. Poor genital hygiene:
10. Poor sanitation sanitation & water supply.
Stages of cervical cancer
A. Stage 0 :
The cancer cells are only in the cells on the surface of the cervix (the layer of cells lining the cervix), without growing into (invading) deeper tissues of the cervix. This stage is also called carcinoma in situ (CIS) which is part of cervical intraepithelial neoplasia grade 3 (CIN3), Stage 0 la not included in the FIGO system.
B. Stage 1 (TL. NO. MO) :
In this stage the cancer has grown into (invaded) the cervix, but it is not growing outside the uterus (T1). The cancer has not spread to nearby lymph nodes (NO) or distant sites (MO).
- a. Stage IA (Tla, NO, MO): This is the earliest form of stage 1. There is a very small amount of cancer, and it can be seen only under a microscope.
- b. Stage IB (Tib, NO, M0): This includes stage I cancers that can be seen without a microscope as well as cancers that can only be seen with a microscope if they have spread deeper than 5 mm (about 1/5 inch) into connective tissue of the cervix or are wider than 7 mm (T1b). These cancers have not spread to nearby lymph nodes (NO) or distant sites (MO).
C. Stage II (T2. NO. MO)
In this stage, the cancer has grown beyond the cervix and uterus, but hasn’t spread to the walls of the pelvis or the lower part of the vagina. It has not spread to nearby lymph nodes (NO) or distant sites (MO).
- a. Stage IIA (T2a, NO, MO): The cancer has not spread into the tissues next to the cervix (the parametria), but it. may have grown into the upper part of the vagina (T2a). It has not spread to nearby lymph nodes (NO) or distant sites (MO).
- b. Stage IIB (T2b, NO, MO): The cancer has spread into the tissues next to the cervix (the parametrin) (T2b). It has not spread to nearby lymph nodes (NO) or distant sites (MO).
D. Stage III (T3. NO. MO)
The cancer has spread to the lower part of the vagina or the walls of the pelvis, and it may be blocking the ureters (tubes that carry urine from the kidneys to the bladder) (T3). It has not spread to nearby lymph nodes (NO) or distant sites (MO).
a. Stage IIIA (T3A, NO, MO): The cancer has spread to the lower third of the vagina but not to walls of the pelvis (T3a). It h It has not spread to nearby lymph nodes (NO) or distant sites (MO).
b. Stage IIIB (T3b, NO, MO; OR T1-T3, N1, M0): The cancer has grown into the walls of the pelvis and/or has blocked one or both ureters causing kidney problems (hydronephrosis) (T3b),
E. Stage IV
This is the most advanced stage of cervical cancer. The cancer has spread to nearby organs or other parts of the body.
a. Stage IVA (T4, NO, MO): The cancer has spread to the bladder or rectum, which are organs close to the cervix (T4). It has not spread to nearby lymph nodes (NO) or distant sites (MO).
b. Stage IVB (any T, any N, M1): The cancer has spread to distant organs beyond the pelvic area, such as the lungs or liver. (M1)

Or (Another answer)
In short
Stage 0 : The cancer cells are only in the cells on the surface of the cervix (the layer of cells lining the cervix), without growing into (invading) deeper tissues of the cervix. This stage is also called carcinoma in situ (CIS) which is part of cervical intraepithelial neoplasia grade 3 (CIN3). Stage 0 is not included in the FIGO system.
Stage I (T1. NO. MO); In this stage the cancer has grown into (invaded) the cervix, but it is not growing outside the uterus (TI). The cancer has not spread to nearby lymph nodes (NO) or distant sites (MO).
1. Stage II (T2, N0, M0): In this stage, the cancer has grown beyond the cervix and uterus, but hasn’t spread to the walls of the pelvis or the lower part of the vagina. It has not spread to nearby lymph nodes (NO) or distant sites (MO).
2. Stage III (T3, N0, M0): The cancer has spread to the lower part of the vagina or the walls of the pelvis, and it may be blocking the ureters (tubes that carry urine from the kidneys to the bladder) (T3). It has not spread to nearby lymph nodes (NO) or distant sites (MO).
3. Stage IV: This is the most advanced stage of cervical cancer. The cancer has spread to nearby organs or other parts of the body.
The following tests are used for screening of the cervix:
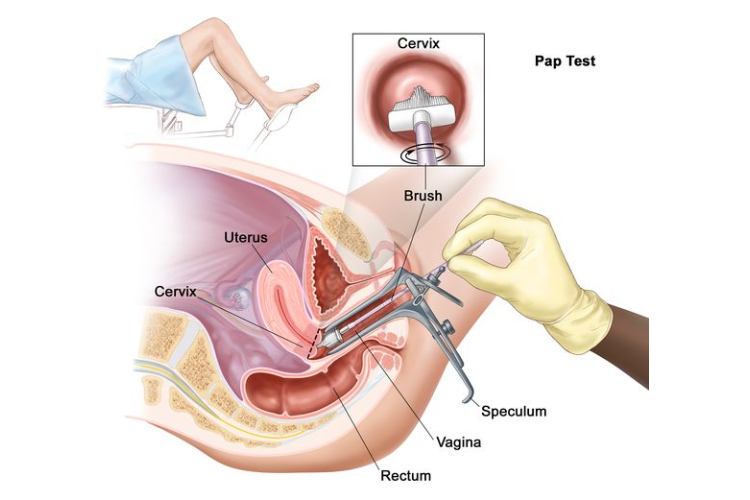
1. Papniolaous Smear (Pap smear): to detect abnormalities of cervical cell causes herpes chalamydia gonorrhea etc.
2. Endometrical biopsy: to study fertility or to detect cancer.
3. Cervical biopsy to detect cancer.
4. Coloscopy use a coloscope to inspect the cervix under magnification to identity abnormal tissue. Usually before cervical biopsy.
Screening of cancer cervix
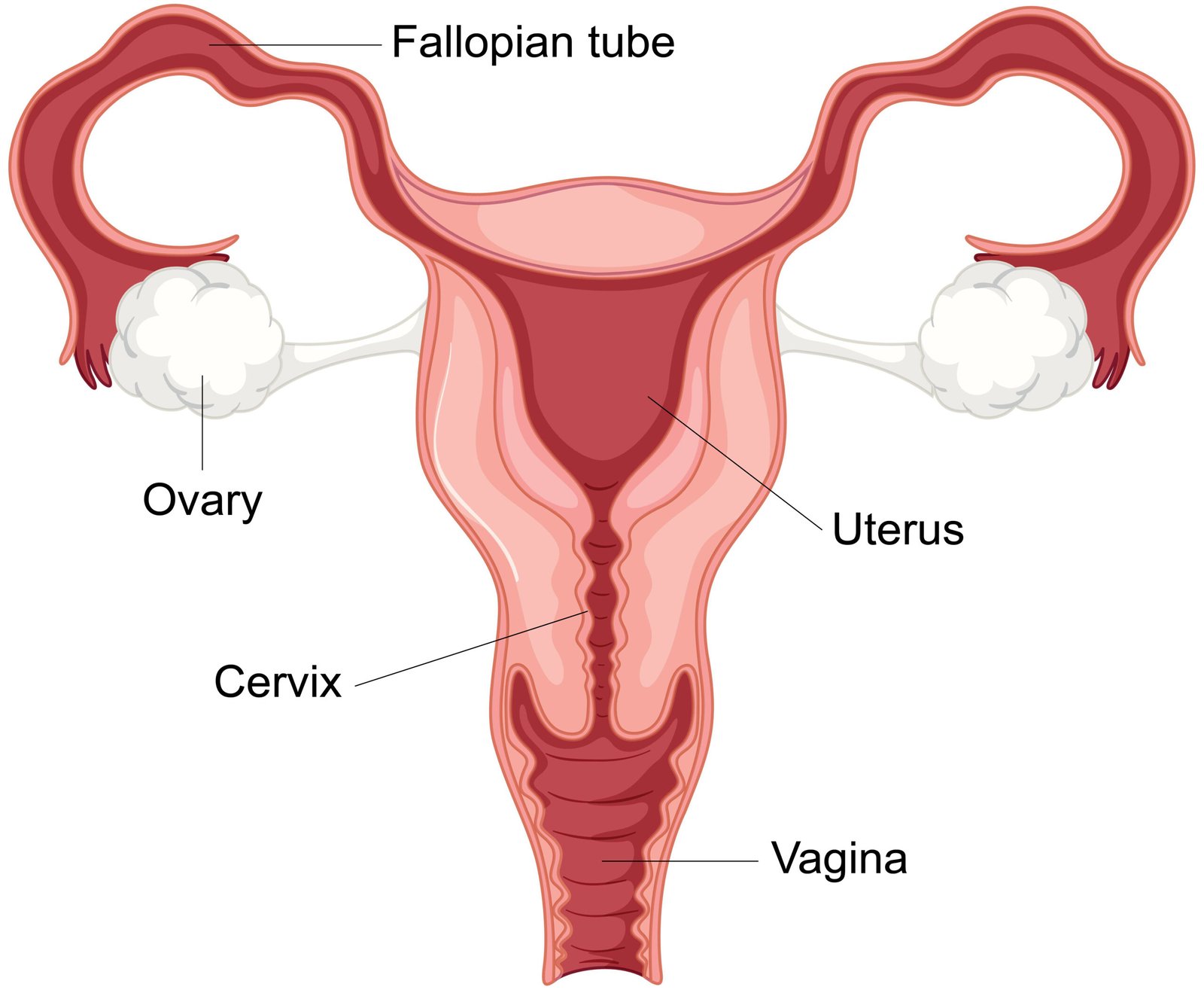
Screening for cervical cancer has become an accepted clinical practice. Cervical cancer can be detected through a Pap smear, that is, a procedure performed during a pelvic examination to obtain and examine cell from the uterine cervical os.
Current policy suggests that all women should have a pap test (cervical cancer), at the beginning of sexual activity, and then every 3 month thereafter. Sexually active girls should have a Pap test performed annually. The American college of obstetricians and Gynecologists recommends annuals examinations to begin by age 18 even when the young women is not sexually active. The incidence of invasive cervical cancer dramatically decreased since the implementation of early detection programs involving the Pap smear. The Guidelines for Pap smear testing the
include the following:
- Testing smear should be performed on all women aged 18 years and older, or earlier if sexually active, and those who have a cervix.
- Pap smear testing should be performed at least every three years. However, the health care provider, based on the risk factors noted earlier, should determine the interval for each person.
- There is insufficient evidence to recommend for or against an upper age limit for Pap testing, but recommendations can be made on other grounds to discontinue regular testing after age 65 in women who have had regular previous screening with normal.
See More:
