Chronie Obstructive Pulmonary Disease (COPD) – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.

Chronie Obstructive Pulmonary Disease (COPD)
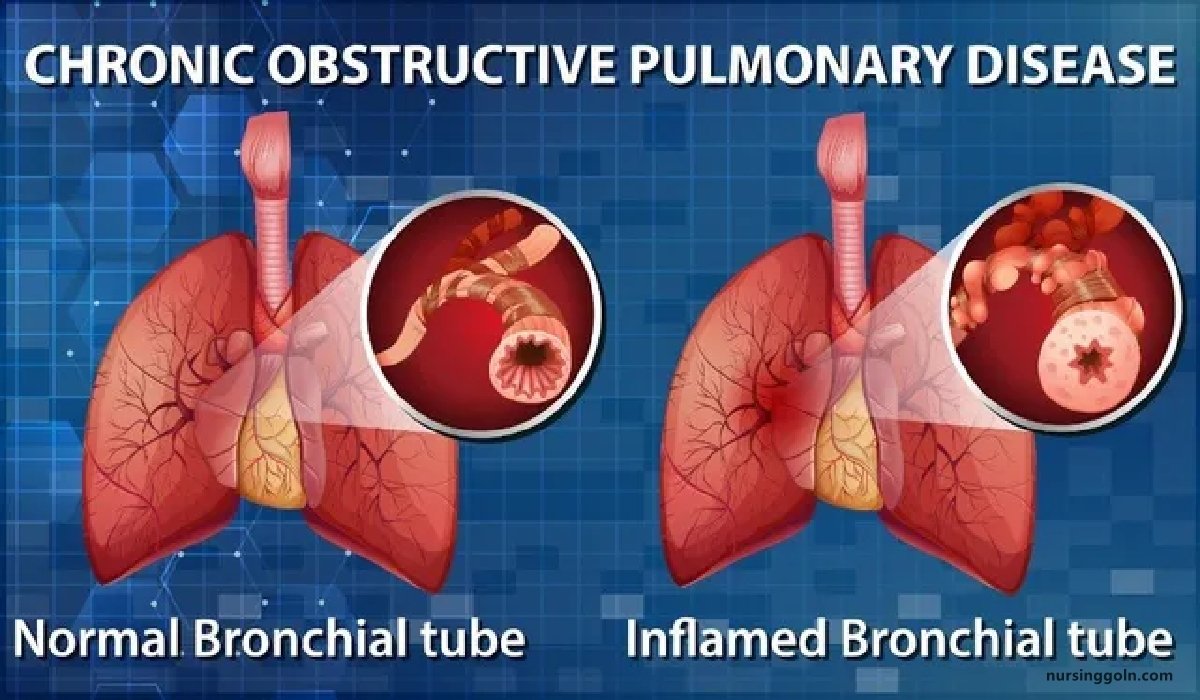
COPD is defined by the presence of airways obstruction, which does not change markedly over several months and, unlike asthma, is not fully reversible.
Or,
Chronic Obstructive Pulmonary Disease (COPD) is a condition of chronic dyspnea with expiratory airflow limitation that does not significantly fluctuate.
It consists of
- Chronic bronchitis
- Emphysema
Classification (According to Severity) of COPD:
| Stage | Severity | FEVI |
| I | Mild | FEV1/FVC<0.7 FEVI ≥80% predicted |
| I | Moderate | FEV1/FVC<0.7 50% ≤ FEV1 <80% predicted |
| III | Severe | FEV1/FVC<0.7 30% ≤ FEV1 <50% predicted |
| IV | Very Severe | FEV1/FVC<0.7 FEVI < 30% predicted or <50% predicted plus chronic respiratory failure |
(Ref by-Harrison’s internal medicine/17th+Davidson’s Medicine 675-19.29/22)
Causes/ Risk/Multiple factors may be responsible for COPD
A. Exposure to-
- Smoking- commonest. (Tobacco-10 pack years for COPD)
- Biomass solid fuel fires: Wood, animal dung, crop residues & coal
- Air pollution- cold, dust (centrilobular emphysema).
- Occupation- coal miners and those who work with cadmium.
- Low socio-economic status,
- Low birth weight.
- Low lung growth.
- Infections-recurrent lung infection, persistent adenovirus in lung tissue, HIV (associated with emphysema).
- Nutrition.
- Cannabis smoking (controversial).
B. Host factors-
- Genetic factors-a, antitrypsin deficiency
- Airway hyper-reactivity.
(Ref by-Davidson’s Medicine 674/22nd+Short case Abdullah Sir/157/5)
Management of COPD:
Clinical features
Symptoms/History
- Age of patient above 40 years & smoker,
- History of persistent cough and sputum production.
- Cough is usually the first symptom and is characteristically accompanied by small amounts mucoid
- Breathlessness
Physical signs
Inspection
- Pursed lip breathing, central cyanosis, prolonged expiration
- Reduced cricosternal distance.
- Intercostals indrawing during inspiration
- Inward movement of lower ribs on inspiration (low flat diaphragm)
- Use of accessory muscles
- Cardiac apex not palpable, loss of cardiac dullness on percussion
On auscultation
- Reduced breath sounds + wheeze
- Heart sound loudest in epigastrium
Investigation
X-Ray chest
- Hyper-translucency of both lung fields and loss of peripheral vascular markings.
- Bullae is pathognomic
- Prominent pulmonary arterial shadow in both hilum.
- Low flat diaphragm
- Tubular heart
- Widening of intercostal space and ribs appear horizontal.
Lung function test
- Spirometry-post bronchodilator FEVI:
- PEFR: Reduced.
- Lung volume: Increased.
Arterial blood gas analysis
- Raised PaCO2
- Fall Pa02
Blood count – To exclude anaemia or document polycythaemia.
Blood culture – To exclude pneumonia.
High resolution CT
ECG
- Low voltage ECG with poor progression of R-wave from VI to V6
- Tall P wave & feature of RVH if corpulmonale develops.
Treatment
1. Smoking cessation, avoidance of dust, fume, smoke
2. Bronchodilators-inhaled route is preferable
- Salbutamol
- Ipratropium bromide
- Theophylline
3. Conticosteroids: Reduce frequency and severity of exacerbation’s (2 or more exaerbations)
4. Pulmonary rehabilitation – Exercise
5. 02. therapy: Long term domiciliary 02 therapy
6. Surgery-Surgical ablation of bullae
7. Other measures:
- Antibiotic for Rx of RTI
- Vaccination of influenza & pneumococcus.
- Proper nutrition.
- Obesity, social isolation should be identify and if possible, improved.
- Mucolytic therapy (acetylcysteine 200 mg orally 8 hrly for 8 weeks.