Cirrhosis of liver – This course is designed to understand the concept of community health nursing: nurses’ roles and interventions in family health, school health, occupational health, environmental health, elderly health care, gender issues, disaster management and principles and terminology of epidemiology. The aim of the course is to acquire knowledge and skills in community health nursing.
Cirrhosis of liver
Cirrhosis is a condition in which the liver does not function properly due to long-term damage. This damage is characterized by the replacement of normal liver tissue by scar tissue. Typically, the disease develops slowly over months or years.
Early on, there are often no symptoms. As the disease worsens, a person may become tired, weak, itchy, have swelling in the lower legs, develop yellow skin, bruise easily, have fluid buildup in the abdomen, or develop spider-like blood vessels on the skin. The fluid build-up in the abdomen may become spontaneously infected.
Other complications include hepatic encephalopathy, bleeding from dilated veins in the esophagus or dilated stomach veins, and liver cancer. Hepatic encephalopathy results in confusion and may lead to unconsciousness.

Cirrhosis is most commonly caused by alcohol, hepatitis B, hepatitis C, and non-alcoholic fatty liver disease. Typically, more than two or three alcoholic drinks per day over a number of years is required for alcoholic cirrhosis to occur. Non-alcoholic fatty liver disease has a number of causes, including being overweight, diabetes, high blood fats, and high blood pressure.
A number of less common causes of cirrhosis include autoimmune hepatitis, primary biliary cirrhosis, hemochromatosis, certain medications, and gallstones. Diagnosis is based on blood testing, medical imaging, and liver biopsy.
Definition of Cirrhosis of Liver
Liver cirrhosis, also known as hepatic cirrhosis, is a chronic hepatic disease characterized by diffuse destruction and fibrotic regeneration of hepatic cells.
Or,
Cirrhosis is a condition in which the liver does not function properly due to long-term damage. This damage is characterized by the replacement of normal liver tissue by scar tissue.
Causes of Liver Cirrhosis
1. Alcohol
2. Chronic viral hepatitis (HBV or HCV)
3. Nonalcoholic fatty liver disease
4. Immune:
- Primary sclerosing cholangitis
- Autoimmune liver disease.
5. Biliary:
- Primary biliary cirrhosis
- Secondary biliary cirrhosis
- Cystic fibrosis
6. Genetic:
- Haemochromatosis
- a-anti trypsin deficiency
- Wilson’s disease
7. Cryptogenic (unknown 15%)
8. Chronic venous outflow obstruction
9. Drugs: Methotrexate, a-methyldopa, INH, rifampicin
Classification of Liver Cirrhosis
These clinical types of cirrhosis reflect its diverse etiology:
1. Laennec’s cirrhosis. The most common type, this occurs in 30% to 50% of cirrhotic patients, up to 90% of whom have a history of alcoholism.
2. Biliary cirrhosis. Biliary cirrhosis results in injury or prolonged obstruction.
3. Postnecrotic cirrhosis. Postnecrotic cirrhosis stems from various types of hepatitis.
4. Pigment cirrhosis. Pigment cirrhosis may result from disorders such as hemochromatosis.
5. Cardiac cirrhosis. Cardiac cirrhosis refers to cirrhosis caused by right-sided heart failure.
6. Idiopathic cirrhosis. Idiopathic cirrhosis has no known cause
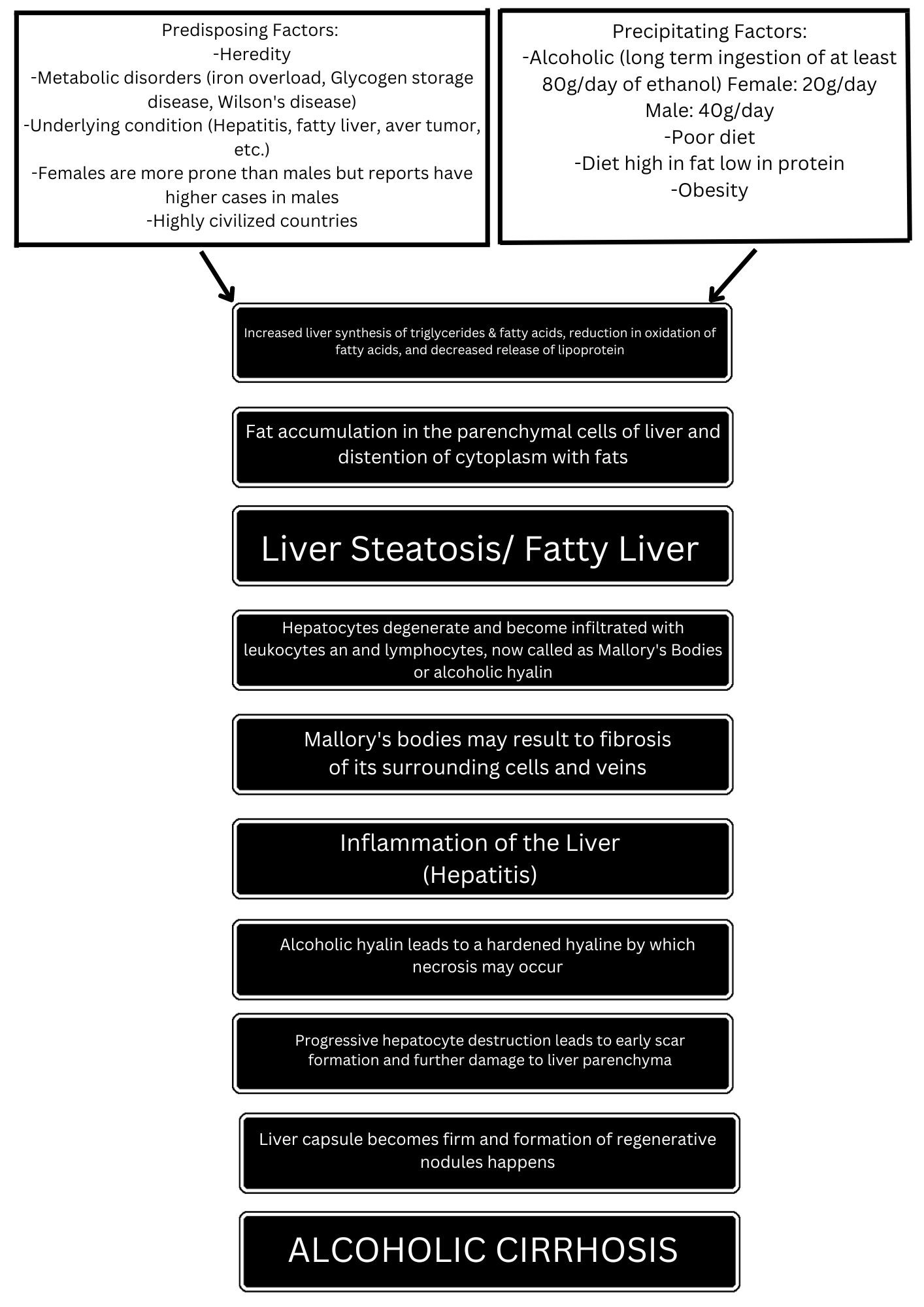
Pathophysiology of Liver Cirrhosis
Management of Liver Cirrhosis:
Clinical Features of Liver Cirrhosis
A. Symptoms
a) General symptoms
- Weakness,
- Fatigue,
- Muscle cramps,
- Weight loss.
b) Nonspecific digestive symptoms
- Anorexia,
- Nausea,
- Vomiting,
- Upper abdominal discomfort,
- Gaseous abdominal distension.
B. Signs
a) Face
- Hepatic faces-Sunken eyes, prominent zygoma, mild jaundice
- Fetor hepaticas – Foul smell from mouth
- Spider telangiectasia (above the nipple)
b) Hand
- Palmar erythema, digital clubbing
- Leukonychia
- Dupuytrens contracture
c) Trunk
- Men: Gynaecomastia
- Women: Breast atrophy
d) Abdomen
- Hepatomegaly: Non tender, hard, irregular, splenomegaly
- Ascites, caput medusa.
- Testicular atrophy, hair loss
- Jaundice
Investigation of Liver Cirrhosis
1. CBC: TC, DC, ESR, H6%, PBF,
2. X-ray chest P/A view
3. Urine for RME
4. Liver function test:
5. Viral markers: HBsAg, HBeAg, Anti – HbcAb
6. USG of whole abdomen
7. Endoscopy of upper GIT
8. Liver biopsy
Treatment of Liver Cirrhosis
Main objective of treatment
1. Detection of treatable causes
2. Prevention of correction of malnutrition
3. Management of chronic cholestasis
4. Treatment of complication
No Rx can reverse cirrhosis or even ensure that no further progression occurs. Rx is symptomatic and supportive.
a. Withdrawal or Rx of etiological factors eg. Alcohol consumption, drugs, haemochromatosis, Wilson’s disease etc.
b. Diet
1. High energy (3000 kcal/d), protein rich (80 – 100 g/d)
2. Fat restriction (if cholestasis)
3. Alcohol must be forbidden
4. Vit. and other supplements may be required
c. To prevent constipation: Lactulose is ginven if required
d. Rx of complication if present (eg. Portal HTN, ascites etc.)
e. Liver transplantation if there is no contra indication
Nursing Management of Liver Cirrhosis:
- Observe stools and emesis for color, consistency, and amount, and test each one for occult blood.
- Monitor fluid intake and output and serum electrolyte levels to prevent dehydration and hypokalemia, which may precipitate hepatic encephalopathy.
- Maintain some periods of rest with legs elevated to mobilize edema and ascites. Alternate rest periods with ambulation.
- Encourage and assist with gradually increasing periods of exercise.
- Encourage the patient to eat high-calorie, moderate protein meals and supplementary feedings. Suggest small, frequent feedings.
- Encourage oral hygiene before meals.
- Administer or teach self-administration of medications for nausea, vomiting, diarrhea or constipation.
- Encourage frequent skin care, bathing with soap, and massage with emollient lotions.
- Keep the patient’s finger nails short to prevent scratching from pruritus.
- Keep the patient quiet and limit activity if signs of bleeding are evident.
- Encourage the patient to eat foods high vitamin C content.
- Use small gauge needles for injections and maintain pressure over injection site until bleeding stops.
- Protect from sepsis through good hand washing and prompt recognition and management of infection.
- Pad side rails and provide careful nursing surveillance to ensure the patient’s safety.
- Stress the importance of giving up alcohol completely.
- Involve the person closest to the patient, because recovery usually is not easy and relapses are common.
Complication of Liver Cirrhosis
The complications of hepatic cirrhosis include the following:
1. Portal hypertension. Portal hypertension is the elevation of pressure in the portal vein that occurs when blood flow meets increased resistance.
2. Esophageal varices. Esophageal varices are dilated tortuous veins in submucosa of the lower esophagus.
3. Hepatic encephalopathy. Hepatic encephalopathy may manifest as deteriorating mental status and dementia or as physical signs such as abnormal involuntary and voluntary movements.
4. Fluid volume excess. Fluid volume excess occurs due to an increased cardiac output and decreased peripheral vascular resistance.