Classification of Meningocelt / myelomeningocele- This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Classification of Meningocelt / myelomeningocele
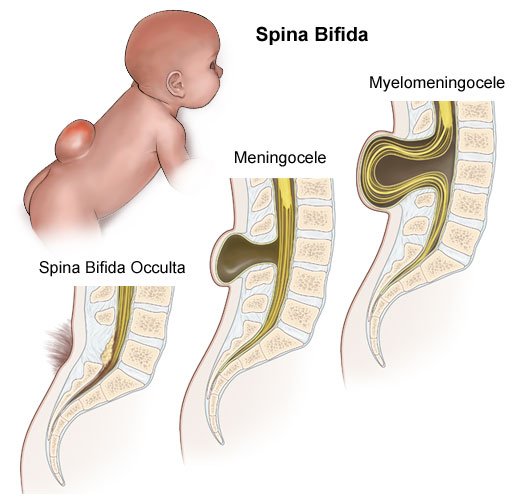
Myelomeningocele
It is a midline cystic sac of meninges with spinal tissue and CSF which herniates through a ha defect in the posterior vertebral arch.
Or
Protrusion of the membranes that cover the spine and part of the spinal cord through a bone defect in the vertebral column.
Causes of meningocele
Maternal risk factors:
1. Exposure to drugs (anti-convulsants: valproate and carbamazepine; oxytetracycline, oral contraceptive drugs, trimethoprim and anti- metabolites)
2. Alcohol or radiation.,
3. Insulin dependent diabetes mellitus (IDDM). Zinc or folate deficiency.
4. Chromosomal abnormalities including trisomy 13 and 15.
Clinical features of meningomyelocele
1. Flaccid paralysis
2. Absence of sensation and drop reflex.
3. Postural abnormalities like club foot
4. Subluxation of hips may be present.
5. Spasticity and hyperactive reflexes may present in thoracic or cervical myelomeningocele.
6. Hydrocephalus is usually associated with this anomaly.
7. Musculoskeletal deformity and hydrosyringomyelia may occur in neonates.
8. Late, in older children, contractures of joints, scoliosis and kyphosis may develop.

Fig: Meningocele
Management of meningocele
A. Surgery:
Early closure of the defect prevents neurological deterioration. Open lesions draining CSF should be closed within 24 hours and closed lesions within 48 hours of birth. If the lesion is infected, administer parenteral and intrathecal antibiotics. Surgery is not done if there is –
- Severe paraplegia at or above L3 level.
- Kyphosis or scoliosis.
- Gross hydrocephalus.
- Associated gross congenital anomalies.
- Intracerebral birth injuries.
- Pre-existing ventriculitis.
B. Supportive nursing management:
1. Prevent infection:
- Position infant to prevent urinary-fecal contamination.
- Clean the defect carefully with sterile saline, apply sterile dressings.
- Avoid uretheral contamination with stool.
- Ensure good perineal hygiene.
- Administer antibiotics/ urinary tract antiseptics if prescribed.
- Ensure adequate fluid intake.
2. Prevent trauma related to delicate spinal lesion:
- Careful handling of infant.
- Place in prone/side lying position.
- Apply protective devices around sac.
- Modify routine nursing activities (feeding, comforting).
3. Prevent skin disintegration due to continual dribbling or urine and feces:
- Keep perianal area clean and dry.
- Diapering is contraindicated until the defect has been repaired and healing is advanced or epithelialization has taken place.
- Change diapers as soon as soiled, if diapered.
4. Prevent increased intracranial pressure (ICP):
- Measure head circumference daily.
- Observe for signs of increased intracranial pressure.
- Prevent or minimize lower extremity deformity
- Carry out passive range of motion exercises.
- Carry out muscle stretching when indicated.
- Maintain hips in slight to moderate abduction and feet in neutral position.
C. Family support:
Parents are encouraged to become involved in care of the child. Such as-
1. They need to learn how to continue the care at home that has been initiated in the hospital positioning
2. Feeding.
3. Skin care
4. Range of motion exercises when appropriate.
5. Parents are taught clean catheterization technique when advised.
6. The family needs to know the symptoms of anticipated complications and how to reach assistance when needed.
7. In cases where the defect has not been repaired, parents are taught to care of the lesion.
8. As the child grows and develops, it is important that the parents encourager and stimulate the infant to accomplish age-appropriate developmental tasks within the limits imposed by the disabilities.
Complications of meningocele
Delay in intervention may result in worsening of neurologic deficit, infection (local or ventriculitis). Late complications include-
1. Hydrocephalus (80-90%).
2. Urinary tract problems.
3. Fecal incontinence or constipation.
4. Developmental dysplasia of hip.
5. Sexual dysfunctions (erection and ejaculation).
6. Epilepsy in 10-30%
7. Ocular problems in 30%
8. Shunt infection in 25%
9. Psychosocial problems.
Prevention of meningocele / neural tube defect
Two major interventional strategies have been accepted for prevention of neural tube defects:
1. Antenatal screening with subsequent termination of affected pregnancies.
2. Folic acid supplementation.
Role of folic acid in primary and secondary prevention of neural tube defects is the most important discovery in the recent past.

Primary prevention: It includes
1. Folate supplementation (400 µg per day) to month before and 3 months after conception prospective mothers
2. A mother with a previous child with neural tube defects should be advised 4 mg per day of folate supplementation in the periconceptional period. Folate supplementation reduces recurrence risk by 70%.
3. Additionally, prenatal diagnosis should be offered.
4. Counseling of family with a previous child with NTD is essential. The risk of recurrence is 47% with 1 affected child, 10% with 2 affected children and 25% with 3 affected children.
5. Food fortification is another possible approach.
Secondary prevention: It includes –
1. Prenatal screening and selective termination of affected fetuses.
2. The condition diagnosed by-
- Ultrasonography (pickup rate 100%)
- Elevated maternal blood alpha-fetoprotein level at 16-18 weeks (accuracy 60-70%) or Elevated amniotic fluid alpha-fetoprotein and acetylcholinesterase levels (accuracy 97%)