Compartment Syndrome – An orthopedic nurse is a nurse who specializes in treating patients with bone, limb, or musculoskeletal disorders. Nonetheless, because orthopedics and trauma typically follow one another, head injuries and infected wounds are frequently treated by orthopedic nurses.
Ensuring that patients receive the proper pre-and post-operative care following surgery is the responsibility of an orthopedic nurse. They play a critical role in the effort to return patients to baseline before admission. Early detection of complications following surgery, including sepsis, compartment syndrome, and site infections, falls under the purview of orthopedic nurses.
Compartment Syndrome
Definition of Compartment Syndrome:
High rise of pressure within a closed osteofacial compartment leading to neurovascular compromise results from trauma or inadvertently applied pressure bandage or from burn, is called compartmental syndrome.
[Ref- Baily & love’s 24/90/355]
Or
Compartment syndrome occurs when increased tissue pressure within a limited anatomic space compromises perfusion. The forearm and lower leg are common locations encountered in trauma patients, most often following vascular or orthopedic injury. If left untreated, this syndrome leads to myoneural necrosis and permanent loss of function or amputation. The degree of damage depends on the degree of compartmental pressure elevation as well as the length of time that pressure is elevated. Concomitant shock increases the degree of damage for any given pressure and time.
[Trauma Manual, The: Trauma and Acute Care Surgery, 3rd Edition Page, 350]
Or
Mubarak defined Compartmental syndrome as an elevation of interstitial pressure in a closed osseofascial compartment that results in microvascular compromise and may cause irreversible damage to the contents of the space.
[Ref-John Ebnezar’s “Textbook of Orthopedics” 4 edition page-32]
Or
A compartment is an area in the body when muscles nerves and blood vessels are encompassed with in tissue. A Compartmental syndrome is a condition in which high pressure with in a closed fascial space or muscle compartment reduces capillary blood perfusion below the level necessary for. tissue viability.
Etiology of a compartmental syndrome:
Any injury leading to severe tissue edema within the fascial compartments can cause compartment syndrome

1. Vascular injury: Vascular injury with limb ischemia leads to tissue edema. Reperfusion generates toxic oxygen metabolites and increases capillary permeability, which worsens the swelling. Bleeding within a closed space from disrupted vessels can also cause the syndrome.
2. Crush injury: Direct injury of tissues by crushing leads to edema and subsequent compartment syndrome.
3. Fractures: Fractures account for 50% of compartment syndromes.
- Tibial fractures are the most common fracture causing the syndrome, but any extremity fracture can lead to increased compartment pressure.
- Open fractures do not preclude the development of compartment syndrome. Compartment syndrome can occur in the absence of fracture with soft-tissue injury, ischemia and reperfusion, prolonged compression (i.e., patients with altered level of consciousness), burns, and operative osteotomies.

4. Trauma: Trauma situations with high risk for the development of compartment syndrome include reperfusion after >4 to 6 hours of ischemia, significant crush injury, and combined venous and arterial injury to a limb.
Or
1. Extrinsic:
- Mechanical constriction (casts, dressings, pneumatic trousers)
- Surgical closure of fascial defects
- Environmental injuries (frostbite, burns)
2. Intrinsic:
- Edema
- Ischemia-reperfusion (vascular injury, thrombosis/embolism, tourniquet)
- Limb compression-immobilization (drug overdose, positioning during general anesthesia)
- Hemorrhage
- Trauma (vessel, bone, soft tissue injuries)
- Bleeding disorders
- Anticoagulant therapy.
Diagnose a case of compartmental syndrome:
Diagnosis of compartment syndrome can be difficult. It has no pathog-nomonic signs or symptoms, and a high index of suspicion must be present in the face of risk factors. Diagnosis is usually established by a collection of symptoms, serial physical examination, and measurement of compartment pressure.
1. Symptoms.
- Pain: Pain out of proportion to physical findings is a classic symptom and is usually elicited in conscious patients with compartment syndrome.
- Paraes-thesias develop with continued hypoperfusion.
- Paralysis is a late finding.
2. Signs: Sign include:
- A swollen,
- Tense compartment and pain on passive stretching.
- Conscious patients may manifest sensory deficit and progressive motor weakness of the involved neuromuscular structures.
- Loss of function may be the earliest sign.
- Loss of peripheral pulses is a late finding usually accompanied by irreversible damage.
- A palpable distal pulse does not exclude compartment syndrome.
Common sites of compartmental syndrome:
A) Compartment syndrome occurs most frequently in the lower leg but can also occur in the forearm, thigh, foot, upper arm, and hand. The lower leg is composed of four compartments containing the following structures:
1. Anterior compartment: tibialis anterior and great toe extensor muscles and the deep peroneal nerve.
2. Ateral (peroneal) compartment: peroneus longus and brevis muscles and the superficial peroneal nerve
3. Superficial posterior compartment: gastrocnemius and soleus muscles and the sural nerve
4. Deep posterior compartment: tibialis posterior and great toe flexor muscles and the tibial nerve
B) The forearm is composed of three compartments containing the following structures:
1. Volar compartment: wrist and finger flexor muscles and the ulnar and median nerves
2. Dorsal compartment: wrist and finger extensor muscles and the posterior interosseous nerve
3. Mobile wad: extensor carpi radialis longus, extensor carpi radialis brevis, and brachioradialis muscles

Compartment pressures:
Compartment pressures: Elevation of compartment pressure precedes the development of symptoms. For this reason, pressure measurement is an important adjunct to diagnosis, particularly in patients with impaired consciousness in whom subjective information is limited and physical examination is unreliable. Although disagreement exists about the cutoff between normal and abnormal compartment pressure, most clinicians consider compartment pressure >30 mmHg an indication for fasciotomy. Compartment pressure between 20 and 30 mmHg in the symptomatic patient or in the face of prolonged hypotension also warrants fasciotomy. Delay in performing fasciotomy worsens outcome. Therefore, if doubt exists regarding the diagnosis, fasciotomy should be performed.
a. Measurement devices commonly available include the needle catheter or Stryker handheld monitor. Needle catheters can produce falsely elevated pressures if used incorrectly, but are universally available. This type of measurement system can be constructed by attaching an 18-gauge needle to a length of saline-filled pressure tubing. This tubing is connected to a pressure transducer similar to that used for arterial pressure measurement. The Stryker monitor is portable and easy to use. Accuracy is comparable between the two devices when used correctly
b. Technique. The skin overlying the compartment to be measured is prepared in a sterile fashion and infiltrated with local anesthetic, if necessary. The needle is advanced through the skin until it pops through the fascia and into the muscular compartment. A small amount of saline is flushed to eliminate interference from catheter plugging, and the pressure is recorded, Correct needle position can be confirmed by noting a brief increase in pressure with compression of the compartment being measured. Measurements should be repeated to confirm elevated pressures.

Treatment of compartmental syndrome patient:
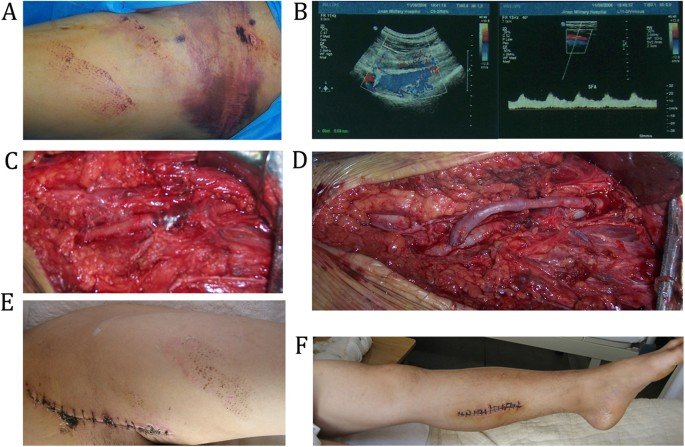
Treatment of compartment syndrome is based on normalizing compartmental pressures to restore adequate tissue perfusion. It is accomplished through wide decompressive fasciotomy of the affected limb. At the time of fasciotomy, debride-ment should be performed only for frankly necrotic tissue. If tissue viability is questionable, the compartment should be reexamined to assess viability.
A) Lower leg fasciotomy: Fasciotomy of the leg should release all four compartments (anterior, lateral, A superficial, and deep posterior). This is easily accomplished with a double incision technique:
1. Make an incision on the lateral leg from just below the head of the fibula to just above the ankle, approximately 1 cm anterior to the fibula.
2. Identify the septum dividing the anterior and lateral compartments and open the fascia on either side of this septum to release these compartments, taking care to avoid the superficial peroneal nerve located along the intercompartmental septum in the lateral compartment.
3. Make a second incision of similar length on the medial side of the leg, 2 cm posterior to the tibia,
4. Open the fascia here to release the superficial posterior compartment. Here, partially detach the proximal soleus from the back of the tibia and incise the fascia, which releases the deep posterior compartment.
B) Thigh fasciotomy: involves the release of three compartments (quadriceps, hamstrings, and adductors). Access and release the quadriceps compartment through an anterolateral incision on the thigh. Then, decompress the hamstring compartment by dividing the intermuscular septum posteriorly. Release the adductor compartment through a separate incision medially along the length of the compartment.
C) Forearm fasciotomy :(Fig. 34-2). Release the volar compartment through an incision along the volar aspect of the forearm, curving across joint spaces to avoid contracture with healing. Most authors advocate performing a carpal tunnel release with this procedure. At this point, measure the dorsal compartmentpreasures and, if they remain elevated, perform dorsal fasciotomy. Release the dorsal compartment through single straight incision on the back of the forearm from the lateral epicondyle to the wrist. a
D) Closure: These wounds are usually closed 5 to 10 days later with either primary closure or skin grafting Alternatively, gradual closure with progressive tension using vessel loops has been described. The goal is to avoid closing the wound under undue tension.
Complications of compartmental syndrams
The major complications of compartment syndrome include infection and rhabdomyolysis.
1. Infection occurs secondary to the presence of necrotic muscle. Control of sepsis requires aggressive debridement of all nonviable tissue, which can lead to significant limitation of function in the affected limb.
2. Rhabdomyolysis may be seen as the sequela of compartment syndrome and is discussed in detail in the following text.
Read more:
