Concept about AIDS – Health of the children has been considered as the vital importance to all societies because children are the basic resource for the future of humankind. Nursing care of children is concerned for both the health of the children and for the illnesses that affect their growth and development. The increasing complexity of medical and nursing science has created a need for special area of child care, i.e. pediatric nursing.
Pediatric nursing is the specialized area of nursing practice concerning the care of children during wellness and illness. It includes preventive, promotive, curative and rehabilitative care of children. It emphasizes on all round development of body, mind and spirit of the growing individual. Thus, pediatric nursing involves in giving assistance, care and support to the growing and developing children to achieve their individual potential for functioning with fullest capacity.
Concept about AIDS
AIDS (Acquired Immune Deficiency Syndrome):
AIDS (Acquired immune deficiency syndrome) is a fatal illness caused by the human immune deficiency virus (HIV), which breaks down the body’s immune system. Leaving the victim vulnerable to a host of life threatening opportunistic infections, neurological disorders or unusual malignancies.
Or,
Acquired immunodeficiency syndrome (AIDS) is a chronic, potentially life-threatening condition caused by the human immunodeficiency virus (HIV). By damaging body’s immune system, HIV interferes with body’s ability to fight the organisms that cause disease,
Incubation period: 6 months to 6 years
(Ref by-K. Park/22/343)
Definition of HIV:
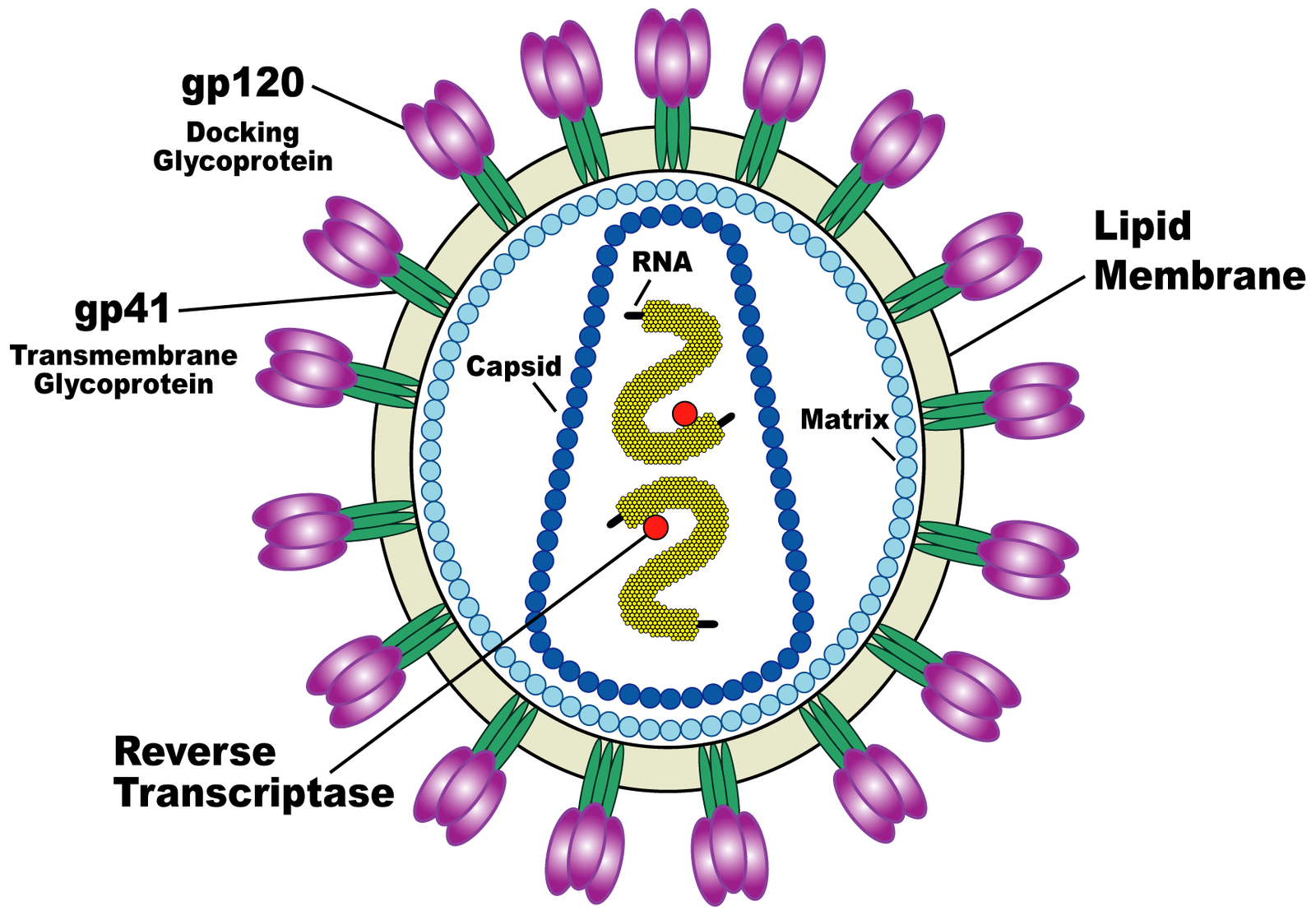
HIV (human immunodeficiency virus) is a virus that attacks the immune system, the body’s natural defense system. Without a strong immune system, the body has trouble fighting off disease. Both the virus and the infection it causes are called HIV.
Mode/Route of Transmission of AIDS:
Infection with HIV essentially requires exchange of semen, vaginal or other body secretion, milk, or blood products infected by the virus.
a) Sexual transmission:
- Route: Anal, Vaginal, Oral sex can spread AIDS.
- Mode: The main mode of transmission via heterosexual routes (over 75% of global cases)
b) Contaminated blood and blood products:
By transfusion of:
- Whole blood cells
- Platelets
- Factor 5 and 9 derived from human plasma
c) Maternal-fetal and mother to child transmission:
Infected mother to child transmission:
- Fetus through the placenta
- Infant during delivery or by breast feeding.
d) Contaminated needles:
- Intravenous drug users.
- Needle sticks injuries.
- Injections.
e) Organ and tissue donation:
- Bone marrow
- Kidney,
- Skin
- Corneas
- Semen.
Epidemiological Features of AIDS:
a) Occurrence: The problem has assumed pandemic proportion affecting industrialized and developing countries.
b) Agent:
- Agent: Human immune deficiency virus (HIV)
- Reservoir of infection – these are cases and carriers. Once a person is infected, it remains lifelong in the body.
- Source of infection:
- Greatest concentration
- Contaminated blood
- Semen
- CSF
Lower concentration:
- Saliva and tear
- Breast milk
- Cervical and vaginal secretion.
c) Host:
➤Age: Mostly 20-50 years, Children under 15 years (less than 3%).
➤Sex: Homosexual, Bisexual, and heterosexual all can be affected. Certain sex practices are at risk, such as multiple sex partners, anal intercourse and male homosexuality. Females are more vulnerable than male due to anatomical structure.
➤ High risk group:
- Male homosexual and bisexuals
- Prostitutes
- Intravenous drug users
- Transfusion recipients of blood and blood products.
- Hemophiliacs and clients of STD.
- Immunology: The victim had normal B-cell formation. But the antibodies are of the non-neutralizing variety. Their T-cell function was far from normal.
d) Mode of Transmission:-
- Sexual transmission
- Contaminated by blood and blood products.
- Mother to child
- Trans placental
- During birth
- After birth: Through Breast feeding
e) Incubation period: Few months to 10 years or even more.
Clinical Features of AIDS:
1. Asymptomatic.
2. Active infection syndrome is characterized by:
- Diarrhoea
- Fever
- Rash
- Arthralgia
- Lymphadenopathy
3. AIDS-related complex:
- Fever
- Weight loss
- Diarrhoea
- Skin rash
- Lymphadenopathy.
- Herpes simplex.
- Oral candidiasis.
- Oral or genital ulcers.
- PID.
- Tubo-ovarian mass.
- Thrombocytopenia
(Ref: D. C. Dutta’s Gynae/7th/126)
Preventive Measure of HIV/AIDS
A. Education:
a) Modification of sexual behavior.
- Avoidance of indiscriminate sex.
- Use of condom.
- Regular venerological screening for high risk groups, eg. Prostitutes.
b) Avoidance of shared razors and tooth brushes.
c) Avoidance the sharing of needles and syringes of intravenous drug users.
d) Women suffering from AIDS or who are at high risk of infection should avoid becoming pregnant through the use of contraceptives.
e) All mass media channels should be involved in educating the people on AIDS, its nature, transmission and prevention.
B. Prevention of blood born HIV transmission:
a) Exclude the high risk donors from donating blood, body organs, sperm and other tissue.
b) All blood should be screened for HIV-1 and HIV-2 before transfusion.
c) Strict sterilization practices should be ensured in hospitals and clinics.
d) Disposal syringes and needles should be used.
e) One should avoid injections unless they are absolutely necessary.
Risk Groups of HIV:
➤ Age: Mostly 20-50 years, Children under 15 years (less than 3%).
➤ Sex:
- Homosexual,
- Bisexual
- And heterosexual all can be affected. Certain sex practices are at risk, such as multiple sex partners, anal intercourse and male homosexuality.
- Females are more vulnerable than male due to anatomical structure.
➤High risk group:
- Male homosexual and bisexuals
- Prostitutes
- Intravenous drug users
- Transfusion recipients of blood and blood products.
- Hemophiliacs and clients of STD.
Diagnosis of AIDS:
a) Clinical features:
Major signs:
- Weight loss 10% of body weight
- Chronic diarrhea > 1 month
- Prolonged fever > 1 month (intermittent or constant)
Minor signs:
- Persistent cough for > 1 month
- Generalized pruritic dermatitis.
- History of herpes zoster
- Oro-pharyngeal candidacies
- Chronic progressive or disseminated herpes simplex infection
- Generalized lymphadenopathy
- Sore throat,
- Lethargy
b) Laboratory diagnosis of AIDS:
Detection of HIV antibody:
- Screening test
- ELISA
- Particle agglutination tests
- Confirmatory tests
- Western blot (WB) most commonly used.
Detection of HIV antibody in new born: PCR (Polymerase chain reaction)
Detection of HIV antigen and nucleic acid: P24, Viral load.
HIV culture
Non-specific tests:
- Lymphopenia
- Reversal of T4: T8 ratio
- Cutaneous energy
- Functional abnormalities of macrophage, B cells.
Complication of HIV or AIDS
A. Complications of the Central Nervous System:
- Cerebral toxoplasmosis
- Cryptococcal meningoencephalitis (or cryptococcoma)
- Viral meningoencephalitis
- Cytomegalovirus
- Herpes simplex virus
- Varicella zoster virus
- Progressive multifocal leukoencephalopathy
- Neurosyphilis
- Primary central nervous system lymphoma
B. Complications of the Gastrointestinal System:
- Cytomegalovirus infection
- HIV-induced enteropathy (or AIDS enteropathy)
- Intestinal malignancies (e.g., non-Hodgkin lymphoma, Kaposi sarcoma, anal squamous cell carcinoma)
- Fat malabsorption (pancreatic exocrine insufficiency)
- Proctitis and anorectal ulcers from sexually transmitted infections
- Protease inhibitor-related adverse effects
C. Other complication:
- Head and neck: Gingivitis, dental and salivary gland disease
- Cardiovascular: Cardiovascular disease, endocarditis
- Pulmonary: Chronic obstructive pulmonary disease, lung cancer (including Kaposi sarcoma and lymphoma)
- Musculoskeletal: Osteopenia, osteoporosis, osteonecrosis
- Hematologic or oncologic: Lymphoma, multiple myeloma
- Dermatologic: Papulosquamous disorders (e.g., eczema, seborrheic dermatitis, psoriasis); molluscum
- contagiosum; Kaposi sarcoma
Pathophysiology of AIDS:
HIV infection passes through a series of steps or stages before it turns into AIDS. These stages of infection as outlined in 1993 by the Centers for Disease Control and prevention are:
1. Seroconversion illness – this occurs in 1 to 6 weeks after acquiring the infection. The feeling is similar to about of flu.
2. Asymptomatic infection – After seroconversion, virus levels are low and replication continues slowly. CD4 and CDs lymphocyte levels are normal. This stage has no symptoms and may persist for years together.
3. Persistent generalised lymphadenopathy (PGL) – The lymph nodes in these patients are swollen for three months or longer and not due to any other cause.
4. Symptomatic infection – This stage manifests with symptoms. In addition, there may be opportunistic infections. This collection of symptoms and signs is referred to as the AIDS-related complex (ARC) and is regarded as a prodrome or precursor to AIDS.
5. AIDS this stage is characterized by severe immunodeficiency. There are signs of life- threatening infections and unusual tumours. This stage is characterized by CD4 T-cell count below 200 cells/mm3.
6. There is a small group of patients who develop AIDS very slowly, or never at all. These patients are called nonprogressors.
The pathological spectrum of HIV infection is changing as the infection spreads into new communities with different potential opportunistic diseases, and as medical science devises drugs against HIV replication.
Risk Factors of HIV/AIDS:
Anyone who is sexually active risks exposure to a sexually transmitted infection to some degree. Factors that may increase that risk include:
1. Having unprotected sex: Vaginal or anal penetration by an infected partner who isn’t wearing a latex condom significantly increases the risk of getting an STI. Improper or inconsistent use of condoms can also increase your risk.
2. Having sexual contact with multiple partners: The more people you have sexual contact with, the greater your risk. This is true for concurrent partners as well as monogamous consecutive relationships.
3. Having a history of STIs: Having one STI makes it much easier for another STI to take hold.
4. Anyone forced to have sexual intercourse or sexual activity: Dealing with rape or assault can be difficult, but it’s important to be seen as soon as possible. Screening. treatment and emotional support can be offered.
5. Abusing alcohol or using recreational drugs: Substance abuse can inhibit your judgment, making you more willing to participate in risky behaviors.
6. Injecting drugs: Needle sharing spreads many serious infections, including HIV, hepatitis B and hepatitis C.
7. Being young: Half of STIs occur in people between the ages of 15 and 24
Medical Management of HIV/AIDS:
Medical management focuses on elimination of opportunistic infections.
1. Treatment of opportunistic infections: For Pneumocystis pneumonia, TMP-SMZ is the treatment of choice; for mycobacterium avian complex, azithromycin or clarithromycin are preferred prophylactic agents; for cryptococcal meningitis, the current primary treatment is IV amphotericin B.
2. Prevention of opportunistic infections: TMP-SMZ is an antibacterial agent used to treat various organisms causing infection.
3. Antidiarrheal therapy: Therapy with octreotide acetate (Sandostatin), a synthetic analog of somatostatin, has been shown to be effective in managing severe chronicdiarrhea.
4. Antidepressant therapy: Treatment for depression in patients with HIV infection involves psychotherapy integrated with imipramine, desipramine or fluoxetine.
5. Nutrition therapy: For all AIDS patients who experience unexplained weight loss, calorie counts should be obtained, and appetite stimulants and oral supplements are also appropriate.

Nursing Management of HIV/AIDS:
The nursing care of patients with HIV/AIDS is challenging because of the potential for any organ system to be the target of infections or cancer.
A. Nursing Assessment
Nursing assessment includes identification of potential risk factors, including a history of risky sexual practices or IV/injection drug use.
- Nutritional status.
- Skin integrity.
- Respiratory status.
- Neurologic status.
- Fluid and electrolyte balance.
- Knowledge level.
B. Diagnosis
The list of potential nursing diagnoses is extensive because of the complex nature of the disease.
- Impaired skin integrity related to cutaneous manifestations of HIV infection, excoriation, and diarrhea.
- Diarrhea related to enteric pathogens of HIV infection.
- Risk for infection related to immunodeficiency.
- Activity intolerance related weakness, fatigue, malnutrition, impaired F&E balance, and hypoxia associated with pulmonary infections.
- Disturbed thought processes related to shortened attention span, impaired memory, confusion, and disorientation associated with HIV encephalopathy.
- Ineffective airway clearance related to PCP, increased bronchial secretions, and decreased ability to cough related to weakness and fatigue.
- Pain related to impaired perianal skin integrity secondary to diarrhea, KS, and peripheral neuropathy.
Imbalanced nutrition, less than body requirements related to decreased oral intake.
C. Planning & Goals
Goals for a patient with HIV/AIDS may include:
- Achievement and maintenance of skin integrity.
- Resumption of usual bowel pattern.
- Absence of infection.
- Improve activity intolerance.
- Improve thought processes.
- Improve airway clearance.
- Increase comfort.
- Improve nutritional status.
- Increase socialization.
- Absence of complications.
- Prevent/minimize development of new infections. Maintain homeostasis. Promote comfort.
- Support psychosocial adjustment.
- Provide information about disease process/prognosis and treatment needs.
D. Nursing Interventions
The plan of care for a patient with AIDS is individualized to meet the needs of the patient.
- Promote skin integrity. Patients are encouraged to avoid scratching; to use nonabrasive, nondrying soaps and apply non perfumed moisturizers; to perform regular oral care; and to clean the perianal area after each bowel movement with nonabrasive soap and water.
- Promote usual bowel patterns. The nurse should monitor for frequency and consistency of stools and the patient’s reports of abdominal pain or cramping.
- Prevent infection. The patient and the caregivers should monitor for signs of infection and laboratory test results that indicate infection.
- Improve activity intolerance. Assist the patient in planning daily routines that maintain a balance between activity and rest.
- Maintain thought processes. Family and support network members are instructed to speak to the patient in simple, clear language and give the patient sufficient time to respond to questions.
- Improve airway clearance. Coughing, deep breathing, postural drainage, percussion and vibration is provided for as often as every 2 hours to prevent stasis of secretions and to promote airway clearance.
- Relieve pain and discomfort. Use of soft cushions and foam pads may increase comfort as well as administration of NSAIDS and opioids.
- Improve nutritional status. The patient is encouraged to eat foods that are easy to swallow and to avoid rough, spicy, and sticky food items.
E. Evaluation
Expected patient outcomes may include:
- Achieved and maintained of skin integrity.
- Resumption of usual bowel pattern.
- Absence of infection.
- Improved activity intolerance.
- Improved thought processes.
- Improved airway clearance.
- Increased comfort.
- Improved nutritional status.
- Increased socialization.
- Absence of complications.
F. Discharge and Home Care Guidelines
Before discharge, the nurse should educate the patient and the family about precautions and the transmission of HIV/AIDS.
- Patients and their families or caregivers should receive instructions about how to prevent disease transmission, including hand-washing techniques and methods for safely handling and disposing of items soiled with body fluids.
- Patients are advised to avoid exposure to others who are sick or who have been recently vaccinated.
- Medication administration. Caregivers in the home are taught how to administer medications, including IV preparations.
- The patient’s adherence to the therapeutic regimen is assessed and strategies are suggested to assist with adherence.
- Infection prevented/resolved.
- Complications prevented/minimized.
- Pain/discomfort alleviated or controlled.

WHO clinical staging of AIDS in children:
1. Stage-1-Asymptomatic
- Persistent generalized lymphadenopathy
2. Stage 2-Unexplained chronic diarrhea
- Severe persistent or chronic candidiasis outside the neonatal period
- Weight loss or failure to thrive
- Persistent fever
- Recurrent severe bacterial infections
3. Stage 3-AIDS defining opportunistic infections
- Severe failure to thrive
- Progressive encephalopathy
- Malignancy
- Recurrent septicemia or meningitis
(Ref: Paediatric Nursing, Parul Datta/3rd/230)
Read more: