Antenatal care – This course is designed to understand the care of pregnant women and newborn: antenatal, intra-natal and postnatal; breast feeding, family planning, newborn care and ethical issues, The aim of the course is to acquire knowledge and develop competencies regarding midwifery, complicated labour and newborn care including family planning.
Concept about Antenatal care
Definition of Antenatal care (ANC):
Prenatal care, also known as antenatal care is a type of preventive healthcare with the goal of providing regular check-ups that allow doctors or midwives to treat and prevent potential health problems throughout the course of the pregnancy while promoting healthy lifestyles that benefit both mother and child.
or
Systemic supervision (examination and advice) of a woman during pregnancy which should be of a regular and periodic nature in accordance with the principles laid down or more frequently according to the need of the individual is called antenatal care.
Antenatal care comprises of:
➤ Careful history taking and examinations
➤ Advice given to the pregnant woman

Aims/Purposes of Antenatal Care (ANC):
1. To screen the ‘high risk’ cases
2. To prevent or to detect and treat at the earliest any complications
3. To ensure continued medical surveillance and prophylaxis
4. To educate the mother about the physiology of pregnancy and labour by demonstrations, charts and diagrams so that fear is removed and psychology is improved.
5. To discuss with the couple about the place, time, and mode of delivery, provisionally and care of the newborn.
6. To motivate the couple about to the need of family planning and also appropriate advice to couple seeking medical termination of pregnancy.
Objective of Antenatal Care:
1. The objective is to ensure a normal pregnancy with delivery of a healthy baby from a healthy mother.
2. The criteria of a normal pregnancy are:
- Delivery of a single baby in good condition at term (between 38-42 weeks)
- Fetal weight of 2.5 kg or more
- With no maternal complications
Values/Importance of Antenatal Care:
1. To screen out high risk cases.
2. Detection of high risk factors.
3. Regular supervision of pregnancy.
4. Antenatal care is said to be the strategy, the intra-natal care is the tactics in obstetrics.qti
5. To make the patient realize that the pregnancy is a physiological process & to give gurich psychological support
Importance of Antenatal check-up:
1. To confirm the pregnancy
2. To confirm that the size of uterus corresponds to the period of pregnancy.
3. To exclude the presence of any tumours or other abnormalities in the pelvis.
4. To diagnose any infections in the vagina or cervix.
5. To diagnose the presence of any ulcer or erosion in the cervix (mouth of the uterus).
6. To take a routine cervical smear to rule out any disease.
7. To assess the size of the pelvic cavity.
8. Since it confirms the presentation of the baby.
9. It helps the doctor to assess the condition of the cervix.
10. It gives a fair idea of the pelvis in comparison to the presenting part of the baby.
11. To screen out high risk cases.
12. Detection of high risk factors.
13. To make the patient realize that the pregnancy is a physiological process & to give psychological support.
14. Regular supervision of pregnancy.
15. A routine examination of urine will provide information about any infection, presence of protein or sugar in urine
Prenatal visit:
1. Health history taking.
2. Abdominal assessment
3. Subsequent visit
If pregnancy is normal, prenatal visits are scheduled every month for 7 months, every 2 weeks during the eight month and every week during the last month?

WHO Recommendation of Antenatal Visit:
In the developing countries, as per WHO, the antenatal visit is curtailed to at least four (4).
| A. 1st visit (by 16 weeks): |
|
| B. 2nd visit (between 24-28 weeks) |
|
| C. 3rd visit (at 32nd week): |
|
| D. 4th visit (at 36th week): |
|
Investigations which is done during ANC Visits:
| A. Routine investigations |
|
| B. Special investigations: |
|
| C. Repetition of the examinations should do at every antenatal visit |
|
Antenatal infection that are important to screening during pregnancy:
1. Rubella
2. Chickenpox (varicella zoster)
3. Cytomegalovirus
4. Measles
5. Toxoplasmosis.
6. Pelvic infection
7. Genital herpes simplex
8. Human immunodeficiency virus.
9. Hepatitis B
10. Syphilis
11. Urinary tract infections
12. Influenza
Prevention of toxoplasmosis of a pregnant women:
The most common ways to become infected with Toxoplasmosis are eating contaminated meat
or produce, or inhaling microscopic toxoplasmosis cysts or spores. Pregnant women can reduce risk of infection by:
➤ Eating fully cooked meat.
➤ Washing raw vegetables and fruit thoroughly.
➤ Washing hands thoroughly after handling raw meat or vegetables.
➤ Avoiding travel to developing countries with a high prevalence of toxoplasma.
➤ Avoiding cat feces.
There are no vaccines for toxoplasmosis and no medications that can be taken to prevent the infection. If women are planning a pregnancy, they should practice the preventive measures outlined above.
Determine fetal Well- being during Pregnancy:
The information gathered during the antenatal visits will help the midwife assess fetal wellbeing. It has some indicators including:
➤ Increasing maternal weight and increasing uterine size.
➤ Uterine size being equivalent to gestational age and remaining correct for gestational age.
➤ Fetal movements that follow a regular pattern (once fetal movements can be felt).
➤ Fetal heart rate is within normal range of 110-160 beats per minute (bpm) when it is auscultated.

Measurement of fundal height:
a. The mother lie on her back with some support under her head and knees
b. Explain to her about procedure before begin touching her abdomen.
c. Touch her abdomen firmly but gently.
d. Walk fingers up the side of her abdomen until feel the top of her pregnant uterus under the skin. It will feel like a hard ball.
e. Lay a soft plastic measuring tape on the mother’s abdomen, holding the zero on the tape at the top of the pubic bone (symphysis pubis)
f. Follow the curve of her abdomen and hold the tape at the top of her uterus.
f. Follow the curve of her abdomen and hold the tape at the top of her uterus.
g. Write down the number of centimeters (cm) from the tap of the public bone to the top of the uterus.
h. Fundal height should increase by 6 finger widths (two finger widths every month) in the second trimester.
i. Wash your hands.
Antenatal Advice of a Pregnant Mother:
A. Dietary advice:
1. The diet during pregnancy should be adequate to provide-
➤ Good maternal health
➤ Optimum fetal growth
➤ The strength and vitality required during labour and
➤ Successful lactation
2. The pregnancy diet ideally should be light, nutritious, easily digestible and rich in protein, minerals and vitamins.
3. The diet should consist in addition to the principal food at least half litre, if not, 1 litre of milk, plenty of green vegetables and fruits. The amount of salt should be of sufficient amount to make the food tasty,
B. Antenatal hygiene:
1. Rest and sleep
2. Bowel: Constipation is common. It may cause backache and abdominal discomfort. Regular bowel movement may be facilitated by regulation of diet taking plenty of fluids, vegetables and milk.
3. Bathing: The patient should take daily bath but be “careful against against slipping in the bathroom due to imbalance
4. Coitus:
➤ Generally coitus is not restricted during pregnancy.
➤ Release of prostaglandins and oxytocin with coitus may cause uterine contractions.
➤ Women with increasing risk of miscarriage or preterm labour should avoid coitus.
C. Smoking & alcohol:
1. It is better to stop smoking & alcohol consuming.
2. Hazards of smoking: Abortion, smaller baby (LBW).
3. Hazards of alcohol: IUGR & fetal mal-development
D. Immunization:
TT immunization: It not only protects the mother but also the neonates
➤ 1st dose: At 5th month;
➤ 2nd dose: At 7th months
E. General advices:
1. Advice to attend for antenatal check-up positively on the schedule date of visit.
2. The patient should be instructed to report as early as possible if some serious symptoms arise; such as intense headache, P/V bleeding or discharge absent or less fetal movements, disturbed sleep with restlessness, urinary trouble epigasun pam, vomming,
scanty micturition etc.
F. She is advised to come to hospital for consideration of admission in the following circumstances:
1. Painful uterine contractions at interval of about 10 minutes or earlier and continued for at least an hour suggestive of onset of labour
2. Sudden gush of watery fluid per vaginam- suggestive of premature rupture of the membranes
3. Active vaginal bleeding, however slight it may be.
Advice that give to a women during last trimester of pregnancy:
a. What to Do:
➤ Continue to take prenatal vitamins.
➤ Stay active unless there is swelling or pain
➤ Work out t in pelvic floor by doing kegel exercises.
➤ Eat a diet high in fruits, vegetables, low-fat forms of protein, and fiber.
➤ Drink lots of water.
➤ Eat enough calories (about 300 calories more than normal).
➤ Keep the teeth and gums healthy. Poor dental hygiene is linked to premature labor.
➤ Get plenty of rest and sleep
b. What to Avoid:
➤ strenuous exercise or strength training that could cause an injury y to stomach alcohol
➤ caffeine (no more than one cup of coffee or tea per day)
➤ smoking
➤ illegal drugs
➤ raw fish or smoked seafood
➤ shark, swordfish, mackerel, or white snapper fish (they have high levels of mercury)
➤ raw sprouts
➤ unpasteurized milk or other dairy products
➤ deli meats or hot dogs
➤ the following prescription drugs: isotretinoin (Accutane) for acne, acitretin (Soriatane) for psoriasis, thalidomide (Thalomid), and ACE inhibitors for high blood pressure
➤ long car trips and airplane flights, if possible
c. Prepare for childbirth:
➤ Attend a parenting class. This is an opportunity to learn about what to expect during labor and the different options available for delivery.
➤ Find a family member or friend who can care for pets or other children
➤ Have an overnight bag packed and ready with items for mother and baby
➤ Plan the route and mode of transportation for getting to the hospital.
➤ Develop a birth plan with doctor. This may include deciding who wants in labor room for support, concerns they have about hospital procedures, and pre-registering with
insurance information.
➤ Have a crib ready for baby and double-check that it’s safe.
➤ Check that smoke detectors and carbon monoxide detectors in home are working properly
➤ Have emergency numbers, including poison control, written somewhere close to phone.
➤ Stock up on baby supplies, like diapers, wipes, and baby clothing in different sizes.
➤ Celebrate pregnancy with friends and family.

Danger signs during antenatal period:
➤ Pain, pressure, or cramping in belly
➤ Contractions that happen more than 4 times an hour or are less than 15 minutes apart
➤ Leaking of fluid from the vagina
➤ Vaginal bleeding
➤ A lot of nausea and vomiting
➤ A temperature over 100°F (37.8°C)
➤ Very bad headache or a headache that lasts for several days
➤ New problems with vision
➤ Less movement and kicking by the baby
➤ Sudden weight gain (3 to 5 pounds within 5 to 7 days) with a lot of swelling of feet, ankles, face, or hands
➤ Seizures
➤ Blood in urine or burning and pain when urinate
➤ Diarrhea that doesn’t go away
➤ Vaginal discharge with a bad odor, irritation, or itching.
Prevent danger signs in antenatal period:
➤ Understands the common danger symptoms.
➤ Knows what to do and feels confident that she can come soon if she develops one of the danger symptoms.
➤ Helps the partner/husband to become aware of the danger symptoms the woman may encounter during the pregnancy.
➤ Maintain a healthy diet.
➤ Be aware of food safety.
➤ Take regular exercise.
➤ Avoid alcohol and tobacco.
➤ Will make him more caring and more concerned.
➤ Helps him to take action (early reporting) when danger symptoms appear.
➤ Alerts him to save money for possible emergencies, e.g. transport to the health facility.
➤ Alerts the family to decide on their preferred place of delivery.
➤ Helps the family get prepared for caring for the mother and her baby after the birth.
Base Line Investigations in ANC:
➤ Hb%
➤ ABO grouping & Rh typing to prevent Rh incompatibility & Rh isoimmunization)
➤ Random blood sugar (to detect DM).
➤ VDRL test (serological tests for syphilis).
Screening Investigations at Booking:
➤ VDRL.
➤ Serological tests for rubella & HBV.
➤ Tests for HIV virus.
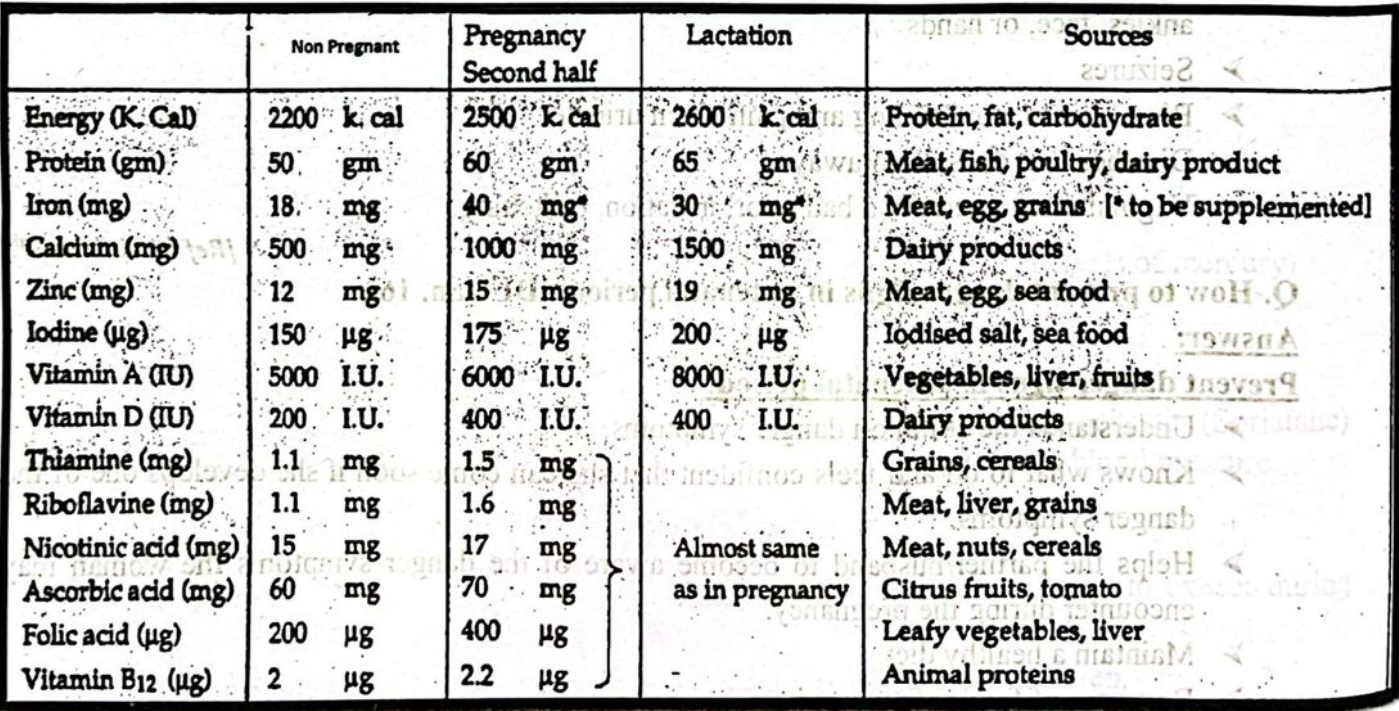
Please write from above & below chart
Obstetric History of a Pregnant Woman:
1. Particulars of the patient:
2. Chief complaints:
➤ Amenorrhoea,
➤ Nausea &/or vomitting,
➤ Increased frequency of micturation,
➤ Breast discomfort etc.
3. History of present illness
4. History of past illness
➤ TB, syphilis, rheumatic heart disease, HTN, DM, kidney diseases etc.
5. Family history: Family history of multiple pregnancies, congenital anomaly, DM, HTN
etc.
6. Personal history: Sleep pattern, bowel & bladder habit, dietary habit etc. –
7. Immunization history
8. Menstrual history
9. Obstetric history:
➤ Chart is to be drawn
➤ Summed up of obstetric history:
No. of living children………………………………..boys……………………………..
girls………………………………..
Health status of the baby……………………Immunization……………………………
Last issue…………………………….
Typical pregnancy visit (Antenatal visits)
First trimester
1. Early first trimester u/s for dating purposes
2. Prenatal labs at your first appointment
3. Sickle cell screening
4. Cystic fibrosis screening
5. Ashkenazi screening
6. Discussion about prenatal testing including
- 1st trimester screening for chromosome abnormalities
- 2nd trimester screening for chromosome abnormalities
- Chorionic villus sampling (cvs) and/or amniocentesis
7. Doptones for fetal heartbeat and urine dips
8. Visits continue monthly
Second trimester
1. Continued prenatal testing
2. 2nd trimester ultrasound for anatomy
3. Discuss classes, tours and pediatricians
4. One hour glucose screening at 28 weeks
5. Administration of rhogam if indicated
6. Fundal height measurements, urine dips, and doptones
7. Visits continue monthly
Third trimester
1. Visits begin every 2 weeks
2. Birth plans reviewed
3. Beta strep and genital cultures at 35-36 weeks
4. Labor instructions reviewed
5. Cervical exams between 38-40 weeks
